A prolapsed disc occurs when the soft, jelly-like center of a spinal disc (called the nucleus pulposus) pushes through a tear in the tougher exterior (annulus fibrosus). This can irritate nearby nerves, leading to pain, numbness, or weakness in an arm or leg. While it’s a common condition, especially among adults between 30 and 50 years old, it can affect anyone.
Key Points:
- Prolapsed disc and herniated disc are often used interchangeably.
- It typically occurs in the lower back (lumbar spine) or neck (cervical spine).
- The severity can range from mild discomfort to debilitating pain.
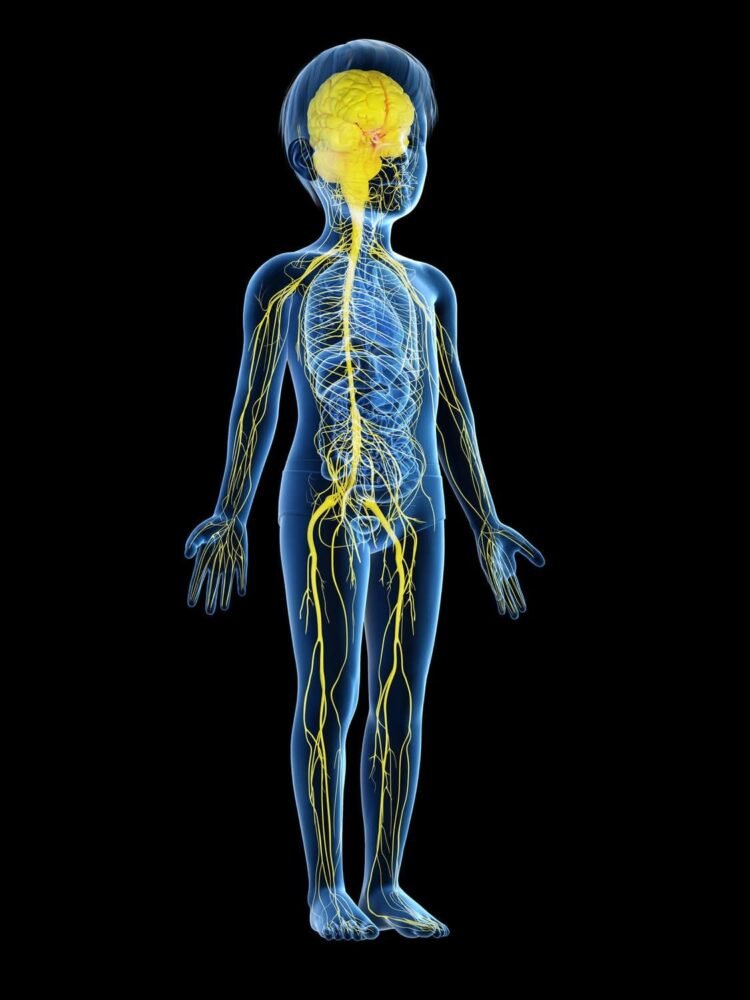
Anatomy of the Spine
Understanding the spine’s structure helps in grasping how a prolapsed disc affects the body.
The Spine
The spine is made up of 33 vertebrae, stacked one on top of the other. These vertebrae are divided into five regions:
- Cervical Spine: Neck region (7 vertebrae)
- Thoracic Spine: Upper and mid-back (12 vertebrae)
- Lumbar Spine: Lower back (5 vertebrae)
- Sacrum: Base of the spine (5 fused vertebrae)
- Coccyx: Tailbone (4 fused vertebrae)
Spinal Discs
Between each vertebra is a spinal disc, acting as a cushion to absorb shock and allow flexibility. Each disc has two parts:
- Nucleus Pulposus: The soft, gel-like center.
- Annulus Fibrosus: The tough, outer layer.
When the annulus fibrosus tears, the nucleus pulposus can bulge out, leading to a prolapsed disc.
Spinal Nerves
Spinal nerves emerge from the spinal cord and pass through spaces between vertebrae. A prolapsed disc can press on these nerves, causing pain and other symptoms.
Types of Prolapsed Discs
Prolapsed discs are categorized based on their location in the spine and the nature of the herniation.
Based on Location
- Lumbar Prolapsed Disc: Occurs in the lower back; most common type.
- Cervical Prolapsed Disc: Occurs in the neck.
- Thoracic Prolapsed Disc: Rare, occurs in the upper and mid-back.
Based on Herniation
- Protrusion: The nucleus pushes against the annulus but hasn’t broken through.
- Extrusion: The nucleus breaks through the annulus but remains connected.
- Sequestration: The nucleus breaks free from the annulus and moves away.
Causes of Prolapsed Disc
Several factors can contribute to the development of a prolapsed disc. Here are 20 common causes:
- Aging: Disc degeneration over time reduces flexibility.
- Wear and Tear: Repetitive movements can strain discs.
- Heavy Lifting: Lifting objects improperly can cause disc injury.
- Sudden Movements: Quick twisting or bending can lead to disc prolapse.
- Obesity: Excess weight increases pressure on spinal discs.
- Genetics: Family history can predispose individuals to disc problems.
- Smoking: Reduces blood flow to discs, accelerating degeneration.
- Poor Posture: Slouching or improper sitting can strain the spine.
- Lack of Exercise: Weak muscles provide less support to the spine.
- Trauma: Accidents or falls can damage discs.
- Repetitive Strain: Jobs requiring repetitive motions can stress discs.
- Dehydration: Discs lose water content, making them less flexible.
- Improper Sleeping Positions: Can strain the back.
- High-Impact Sports: Activities like football or gymnastics can stress the spine.
- Psychological Stress: Can lead to muscle tension, affecting spinal health.
- Dietary Deficiencies: Lack of essential nutrients weakens spinal structures.
- Hormonal Changes: Can affect disc health, especially in women.
- Chronic Coughing or Sneezing: Puts pressure on spinal discs.
- Occupational Hazards: Jobs involving heavy lifting or prolonged sitting.
- Improper Footwear: Poor shoes can affect posture and spinal alignment.
Symptoms of Prolapsed Disc
The symptoms can vary depending on the disc’s location and the extent of herniation. Here are 20 possible symptoms:
- Lower Back Pain: Common in lumbar disc prolapse.
- Neck Pain: Common in cervical disc prolapse.
- Radiating Pain: Pain spreading to arms or legs.
- Numbness: Loss of sensation in affected areas.
- Tingling: “Pins and needles” sensation.
- Muscle Weakness: Affected muscles may weaken.
- Loss of Reflexes: Reduced reflex actions in limbs.
- Difficulty Walking: Especially with lower back prolapse.
- Pain Worsens with Movement: Activities like bending or twisting exacerbate pain.
- Pain at Night: Discomfort may intensify during sleep.
- Foot or Hand Weakness: Depending on the disc’s location.
- Incontinence: Rare, but severe prolapse can affect bladder or bowel control.
- Limited Range of Motion: Difficulty moving the affected area.
- Sharp or Burning Pain: Especially along nerve pathways.
- Shooting Pain: Sudden, intense pain episodes.
- Headaches: In cervical prolapse, headaches can occur.
- Difficulty Holding Items: Due to arm or leg weakness.
- Balance Issues: Difficulty maintaining stability.
- Foot Drop: In severe cases, inability to lift the front part of the foot.
- Chronic Pain: Persistent discomfort lasting weeks or months.
Diagnostic Tests for Prolapsed Disc
Diagnosing a prolapsed disc involves a combination of medical history, physical exams, and imaging tests. Here are 20 diagnostic methods:
- Physical Examination: Assessing pain areas and physical function.
- Neurological Examination: Checking reflexes, muscle strength, and sensation.
- X-Rays: Viewing the spine’s structure and alignment.
- MRI (Magnetic Resonance Imaging): Detailed images of soft tissues, including discs and nerves.
- CT Scan (Computed Tomography): Cross-sectional images of the spine.
- Myelogram: Injecting dye into the spinal canal before X-ray or CT.
- EMG (Electromyography): Testing nerve and muscle function.
- Nerve Conduction Studies: Measuring electrical signals in nerves.
- Discography: Injecting dye into a disc to identify the source of pain.
- Bone Scan: Detecting bone abnormalities.
- Ultrasound: Less common, can assess soft tissues.
- DEXA Scan: Measuring bone density to rule out osteoporosis.
- Spinal Tap (Lumbar Puncture): Analyzing spinal fluid.
- Flexion and Extension X-Rays: Viewing spine movement.
- SPECT Scan (Single Photon Emission Computed Tomography): Detailed bone images.
- Radionuclide Scans: Assessing blood flow to spinal areas.
- Standing X-Rays: Evaluating spine under natural weight-bearing conditions.
- Posture Analysis: Assessing spinal alignment.
- Gait Analysis: Observing walking patterns for abnormalities.
- Pain Mapping: Identifying pain sources through various techniques.
Non-Pharmacological Treatments
Managing a prolapsed disc doesn’t always require medications. Here are 30 non-drug treatments:
- Rest: Short periods of inactivity to reduce inflammation.
- Physical Therapy: Guided exercises to strengthen back muscles.
- Chiropractic Care: Spinal adjustments to alleviate pressure.
- Massage Therapy: Relieves muscle tension around the spine.
- Hot and Cold Therapy: Alternating heat and ice to reduce pain and swelling.
- Yoga: Improves flexibility and strengthens core muscles.
- Pilates: Enhances spinal stability and posture.
- Acupuncture: Stimulates nerves to reduce pain.
- TENS (Transcutaneous Electrical Nerve Stimulation): Uses electrical impulses for pain relief.
- Traction: Gently stretches the spine to relieve pressure.
- Ergonomic Adjustments: Improving workplace setups to support the spine.
- Weight Loss: Reduces strain on spinal discs.
- Posture Training: Learning proper sitting and standing techniques.
- Core Strengthening Exercises: Strengthens abdominal and back muscles.
- Swimming: Low-impact exercise that supports the spine.
- Walking: Gentle movement to maintain spine flexibility.
- Mindfulness and Meditation: Manages pain through mental techniques.
- Biofeedback: Teaches control over certain body functions to reduce pain.
- Heat Packs: Apply warmth to soothe muscles.
- Ice Packs: Reduce inflammation and numb pain.
- Stretching Exercises: Maintains flexibility and reduces stiffness.
- Low-Impact Aerobics: Enhances overall fitness without stressing the spine.
- Kinesio Taping: Supports muscles and reduces pain.
- Ergonomic Furniture: Using chairs and mattresses that support spinal health.
- Proper Lifting Techniques: Prevents further disc injury.
- Avoiding Prolonged Sitting: Regular breaks to reduce spine strain.
- Swimming Pool Therapy: Buoyancy reduces spine pressure during exercises.
- Tai Chi: Gentle movements improve balance and flexibility.
- Spinal Decompression Therapy: Non-surgical method to relieve pressure.
- Lifestyle Modifications: Incorporating healthier habits to support spine health.
Drugs for Prolapsed Disc
Medications can help manage the pain and inflammation associated with a prolapsed disc. Here are 20 commonly used drugs:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs):
- Ibuprofen (Advil)
- Naproxen (Aleve)
- Indomethacin
- Acetaminophen:
- Tylenol
- Muscle Relaxants:
- Cyclobenzaprine (Flexeril)
- Methocarbamol (Robaxin)
- Corticosteroids:
- Prednisone
- Dexamethasone
- Oral Steroids:
- Methylprednisolone
- Opioids:
- Hydrocodone
- Oxycodone
- Antidepressants:
- Amitriptyline
- Duloxetine (Cymbalta)
- Anticonvulsants:
- Gabapentin (Neurontin)
- Pregabalin (Lyrica)
- Topical Analgesics:
- Diclofenac gel
- Capsaicin cream
- Local Anesthetics:
- Lidocaine patches
- Non-Opioid Analgesics:
- Tramadol
- Bisphosphonates:
- Alendronate
- Calcitonin:
- Miacalcin
- Chiropractic Medications:
- Topical NSAIDs
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs):
- Venlafaxine
- Selective Serotonin Reuptake Inhibitors (SSRIs):
- Fluoxetine
- NMDA Receptor Antagonists:
- Memantine
- Botulinum Toxin (Botox):
- For muscle spasticity
- Vitamin B12 Supplements:
- Supports nerve health
- Glucosamine and Chondroitin:
- Joint support supplements
Note: Always consult a healthcare professional before starting any medication.
Surgeries for Prolapsed Disc
When conservative treatments fail, surgery might be necessary. Here are 10 surgical options:
- Discectomy:
- Removal of the herniated portion of the disc.
- Laminectomy:
- Removal of part of the vertebra to relieve pressure.
- Microdiscectomy:
- Minimally invasive discectomy with smaller incisions.
- Spinal Fusion:
- Joining two or more vertebrae to stabilize the spine.
- Artificial Disc Replacement:
- Replacing the damaged disc with an artificial one.
- Foraminotomy:
- Enlarging the nerve passageway to relieve pressure.
- Endoscopic Discectomy:
- Using an endoscope to remove disc material.
- Laser Discectomy:
- Using laser technology to remove disc fragments.
- Vertebroplasty:
- Injecting bone cement to stabilize fractured vertebrae.
- Kyphoplasty:
- Similar to vertebroplasty but includes balloon inflation to restore vertebral height.
Considerations:
- Surgery risks include infection, nerve damage, and recurrence.
- Recovery time varies based on the procedure and individual health.
Preventions of Prolapsed Disc
Preventing a prolapsed disc involves maintaining spinal health and avoiding risk factors. Here are 10 preventive measures:
- Maintain a Healthy Weight: Reduces stress on the spine.
- Exercise Regularly: Strengthens back and core muscles.
- Practice Good Posture: Prevents unnecessary strain on the spine.
- Lift Properly: Use your legs, not your back, when lifting objects.
- Avoid Smoking: Enhances blood flow to spinal discs.
- Stay Hydrated: Keeps spinal discs healthy and flexible.
- Use Ergonomic Furniture: Supports proper spinal alignment.
- Stretch Daily: Maintains flexibility and reduces muscle tension.
- Avoid Prolonged Sitting or Standing: Take regular breaks to move.
- Wear Supportive Footwear: Ensures proper posture and reduces spine strain.
When to See a Doctor
If you experience symptoms of a prolapsed disc, it’s essential to consult a healthcare professional. Seek medical attention if you:
- Have severe or persistent back or neck pain.
- Experience numbness or tingling in limbs.
- Notice muscle weakness or loss of strength.
- Encounter difficulty controlling bladder or bowels.
- Suffer trauma from an accident or injury.
- Experience pain that worsens over time despite home treatments.
- Have difficulty walking or maintaining balance.
- Notice pain at night that disrupts sleep.
- Experience unexplained weight loss with back pain.
- Have a history of cancer with new spinal pain.
Early diagnosis and treatment can prevent complications and improve outcomes.
Frequently Asked Questions (FAQs)
1. What Causes a Disc to Prolapse?
A prolapsed disc can result from age-related wear and tear, heavy lifting, sudden movements, obesity, genetics, smoking, poor posture, lack of exercise, trauma, and repetitive strain.
2. How is a Prolapsed Disc Diagnosed?
Diagnosis typically involves a physical examination, medical history review, and imaging tests like MRI or CT scans to visualize the herniated disc and assess nerve involvement.
3. Can a Prolapsed Disc Heal on Its Own?
Yes, many prolapsed discs heal with conservative treatments like rest, physical therapy, and medications. However, severe cases may require surgical intervention.
4. What Exercises are Safe with a Prolapsed Disc?
Low-impact exercises such as walking, swimming, yoga, and specific physical therapy routines can be beneficial. Always consult a healthcare provider before starting any exercise regimen.
5. Is Surgery Always Necessary for a Prolapsed Disc?
No, surgery is not always required. Most cases respond well to non-surgical treatments. Surgery is considered when symptoms are severe or persistent despite conservative measures.
6. What is the Recovery Time After Disc Surgery?
Recovery time varies based on the type of surgery and individual health. Generally, it can range from a few weeks to several months.
7. Can a Prolapsed Disc Recur?
Yes, there is a possibility of recurrence, especially if preventive measures are not followed. Maintaining spinal health is crucial to reduce the risk.
8. How Does a Prolapsed Disc Affect Daily Life?
It can limit mobility, reduce the ability to perform physical activities, cause chronic pain, and affect overall quality of life. Proper management can mitigate these impacts.
9. Are There Alternative Therapies for a Prolapsed Disc?
Yes, therapies like acupuncture, massage, chiropractic care, and mindfulness techniques can complement traditional treatments and help manage symptoms.
10. What Lifestyle Changes Can Prevent a Prolapsed Disc?
Maintaining a healthy weight, regular exercise, good posture, proper lifting techniques, avoiding smoking, staying hydrated, and using ergonomic furniture are key preventive measures.
Conclusion
A prolapsed disc is a manageable condition with the right knowledge and treatment. Understanding its causes, symptoms, and treatment options empowers you to take proactive steps toward spinal health. Whether through lifestyle changes, non-pharmacological treatments, medications, or, in some cases, surgery, effective management is achievable. Always consult healthcare professionals for personalized advice and treatment plans.







