
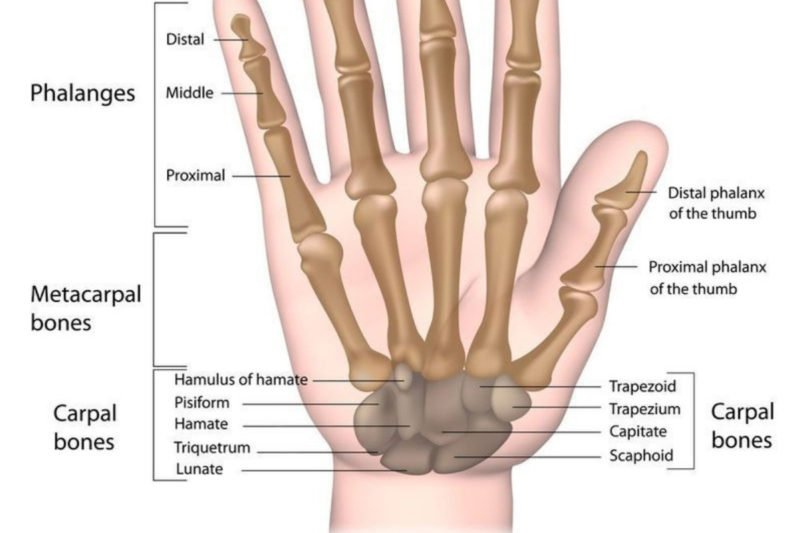
Avascular Necrosis of the Lunate/Kienbock’s Disease, also known as avascular necrosis of the lunate, is a condition in which the lunate bone, one of eight small bones in the wrist, loses its blood supply, leading to the death of the bone. The lunate is a central bone in the wrist that is important for proper movement and support of the joint. It works closely with the two forearm bones (radius and ulna) to help the wrist move.
Kienbock disease refers to avascular necrosis of the lunate carpal bone, known as keratomalacia. It was first recognized and described by Austrian radiologist Robert Kienböck in 1910.[rx]

Staging of Kienbock’s Disease
Staging of Kienböck disease is essential for treatment planning and divides into morphological and functional staging.
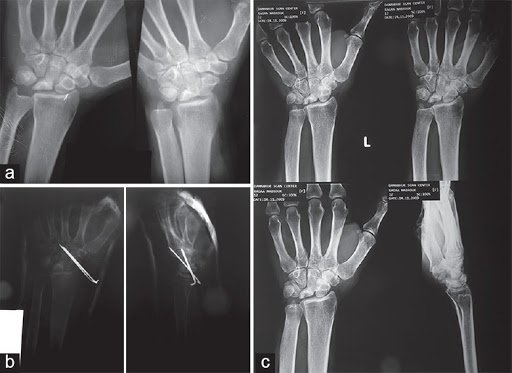
Morphologic Staging follows the Lichtman Classification, which is based on radiographic and MR imaging findings and has low interobserver variability.[rx][rx][rx]
Stage 1: Normal radiograph, lunate signal intensity changes on MRI.
Stage 2: Lunate sclerosis on radiography with or without fracture lines. The lunate shape is normal.
Stage 3: Collapse of the lunate articular surface.
-
3A: with preserved carpal alignment and height.
-
3B: with scaphoid flexion and loss of carpal height.
-
3C: with an associated coronal fracture
Stage 4: Stage 3B + radio-carpal or mid-carpal arthrosis.
Functional Staging – relies on contrast-enhanced MRI to assess osseous perfusion and the extent of necrosis. It is helpful to guide revascularization techniques during surgery for morphologic stages 2 and 3A. The pre- and post-contrast images are acquired using a T2 fat-suppressed sequence.[rx][rx]
Stage 1: Intense homogeneous contrast enhancement reflects bone marrow ischemia and edema and a viable lunate (corresponds to morphologic stage 1).
Stage 2: Patchy, inhomogeneous enhancement reflects partial necrosis. The remaining viable portion is usually distal.
Stage 3: Absent contrast enhancement reflects complete necrosis.
Causes of Kienbock’s Disease
No consensus is present regarding the primary causative factor of Kienböck disease. It is multifactorial, related to the following variables:
- Ulnar negative variance (or ulna minus) – This refers to a disproportionately shortened ulna when compared to the radius. As deduced from the previous section, a shortened ulna results in excessive mechanical stress and repetitive microtrauma exerted on the lunate by the relatively long radius. In some studies, up to 78% of Kienböck cases correlate with this finding.[rx]
- Vascular supply to the lunate bone – The lunate receives its blood supply from a variable number of dorsal and volar penetrating arteries that branch off of the dorsal and palmar radiocarpal and intercarpal arches. Intraosseous collaterals are sparse. The lower the number of penetrating arteries (especially volar branches from the radiocarpal palmar arch), the greater the likelihood of developing the disease.[rx][rx]
- Lunate morphology – The risk of developing Kienböck disease increases as lunate size decreases, forcing the lunate to carry a larger axial load. The lunate can either have a square/rectangular shape (type II or type III), or a more triangular shape whereby the medial articular facet is absent (type I). The latter has a weaker trabecular pattern and is a risk factor for disease development and progression.[rx]
- Radial inclination angle – the radial inclination angle is a measurement of the angle formed between the horizontal and a line drawn from the ulnar tip of the radial articular surface to the tip of the radial styloid. The risk of developing Kienböck disease increases as the radial inclination angle decreases.[rx]
- Skeletal variations – The ulna can be shorter than the radius, which may cause issues. Or, the shape of the lunate bone may be irregular.
- Trauma – A single incident or multiple incidents may cause this disease.
- Other medical conditions – Kienbock’s disease can be found more commonly in people who have medical conditions that affect blood supply, and it is also associated with diseases like lupus, sickle cell anemia and cerebral palsy.
Symptoms of Kienbock’s Disease/Avascular Necrosis of the Lunate
Common signs and symptoms are:
- Swelling, pain, and stiffness in the wrist
- Clicking or clunking in the wrist
- The weakening of grip strength
- Tenderness directly over the lunate bone
- Difficulty or pain when turning the hand upward
- Wrist pain
- Tenderness directly over the lunate bone
- Decreased motion or stiffness of the wrist
- Swelling
Diagnosis of Kienbock’s Disease/Avascular Necrosis of the Lunate
History
Your doctor in the emergency department may ask the following questions
-
How – How was the fracture created, and, if chronic, why is it still open? (underlying etiology)
-
When – How long has this fracture been present? (e.g., chronic less than 1 month or acute, more than 6 months)
- Where – Where on the body parts is it located? Is it in an area that is difficult to offload, complicated, or keep clean? Is it in an area of high skin tension? Is it near any vital organ and structures such as a major artery?
- What is your Past – Has your previous medical history of fracture? Are you suffering from any chronic disease, such as hypertension, blood pressure, diabetes mellitus, previous major surgery? What kind of medicine did you take? What is your food habits, geographic location, Alcohol, tea, coffee consumption habit, anabolic steroid uses for athletes, etc?
Physical
Physical examination is done by your doctor, consisting of palpation of the fracture site, eliciting boney tenderness, edema, swelling. If the fracture is in the dept of a joint, the joint motion, normal movement will aggravate the pain.
- Inspection – Your doctor also check superficial tissue, skin color, involving or not only the epidermal layer or Partial-thickness affects the epidermis and extend into the dermis, but full-thickness also extends through the dermis and into the adipose tissues or full-thickness extends through the dermis, and adipose exposes muscle, bone, evaluate and measure the depth, length, and width of the fracture. Access surrounding skin tissue, fracture margins for tunneling, rolled, undermining fibrotic changes, and if unattached and evaluate for signs and symptoms of infect warm, pain, delayed healing.
- Palpation – Physical examination may reveal tenderness to palpation, swelling, edema, tenderness, worm, temperature, open fracture, closed fracture, microtrauma, and ecchymosis at the site of fracture. Condition of the surrounding skin and soft tissue, quality of vascular perfusion and pulses, and the integrity of nerve function.
- Motor function – Your doctor may ask the patient to move the injured area to assist in assessing muscle, ligament, and tendon function. The ability to move the joint means only that the muscles and tendons work properly, and does not guarantee bone integrity or stability. The concept that “it can’t be fractured because you can move it” is not correct. The jerk test and manual test are also performed to investigate the motor function.
- Sensory examination – assesses sensations such as light touch, worm, paresthesia, itching, numbness, and pinprick sensations, in its fracture side. Sensory 2-point discrimination
- Range of motion – A range of motion examination of the fracture associate joint and it’s surrounding joint may be helpful in assessing the muscle, tendon, ligament, cartilage stability. Active assisted, actively resisted exercises are performed around the injured area joint.
- Blood pressure and pulse check – Blood pressure is the term used to describe the strength of blood with which your blood pushes on the sides of your arteries as it’s pumped around your body. An examination of the circulatory system, feeling for pulses, blood pressure, and assessing how quickly blood returns to the tip of a toe to heart and it is pressed the toe turns white (capillary refill).
Lab Test
Laboratory tests should be done as an adjunct in overall medical status for surgical treatment.
- CBC, ESR test
- Random blood sugar, glucose, and routine diabetes test if the patient has diabetes mellitus.
- Microscopic urine examination test, and stool test.
- ECG, EKG test for heart abnormality is present
- Ultrasonography test in some cases.
- Normalized hemoglobin, hematocrit test
- Coagulation profile with bleeding time and coagulation time test, prothrombin time (PT) test for surgery if needed,
- Partial thromboplastin time (PTT), and platelet counts will be needed for operative intervention.
- Serum creatinine test,
- Serum lipid profile
- Serum uric acid test
Kienböck disease is a clinical and imaging diagnosis. Both radiography/computed tomography and magnetic resonance imaging (MRI) is highly specific. However, MRI is the most sensitive and detects radiographically occult cases.
- Magnetic Resonance Imaging – Diffuse decrease in lunate bone marrow signal on T1-weighted images is a hallmark of the disease. Signal changes on T2-weighted images or short-TI inversion recovery (STIR, which nullifies signal from fat) images vary with progression and extent of osteonecrosis. MRI also assesses the integrity of the articular cartilage.[rx][rx]
- Radiography – Normal early in the disease. Findings, when present, depend on the morphological stage and include diffuse lunate sclerosis, cystic changes, articular surface collapse, carpal collapse, mid-carpal, and/or radio-carpal secondary arthrosis. Coronal fractures may occur in lunates with a type I morphology.[rx][rx]
- Computed Tomography – This is useful for surgical planning. It is also more sensitive than radiography for detecting subtle subchondral fractures, coronal lunate fractures, fragmentation, carpal instability, and the degree of trabecular disruption. Patients are frequently re-staged after CT imaging.[rx]
- Nuclear Scintigraphy – Findings are non-specific. It was previously found used as an adjunct for diagnosing early-stage disease. It has fallen out of favor since introducing MRI.[rx]
- Ulnar impaction syndrome – More common with ulnar positive variance and results from repetitive microtrauma to the lunate from a relatively long ulna. Similar to Kienböck disease, ulnar impaction syndrome results in decreased T1-weighted signal coupled with increased T2 signal if hyperemia exists, or decreased T2 signal if the disease has already progressed to lunate sclerosis. The signal changes in Kienböck disease, however, are more diffuse or more severe on the radial side of the lunate. Additionally, ulnar impaction syndrome affects the ulnar head and triquetrum, which are intact in Kienböck patients.[rx][rx].
- Lunate intraosseous ganglion – Intraosseous ganglia are true cysts that have low T1 signal and high T2 signal on MRI. Sharp, smooth margins on both MRI and radiography allow distinction from Kienböck disease.[rx]
- Bone contusion – It May be difficult to distinguish early-stage Kienböck disease on MRI. A history of recent trauma and concomitant injuries to the wrist/hand, in this case, would aid in making the diagnosis.[rx]
- Arthritis – Bone marrow signal changes in inflammatory or degenerative arthritides may mimic those seen in Kienböck disease. Distinguishing features include demographics, clinical presentation, and absence of ulna minus in arthritis.[rx]
- Osteoid osteoma – Osteoid osteoma of the carpal bones is rare, and only a few case reports exist in the literature. Clinical presentation and the finding of a lucent nidus within a sclerotic rim on CT differentiate it from Kienböck disease.[rx]
- Enostosis/bone island – Has low signal intensity on all sequences, however, it shows preserved bone morphology and the area of “sclerosis” is stellate and interdigitated with the normal trabeculae.[rx]
Treatment of Kienbock’s Disease/Avascular Necrosis of the Lunate
The goal of treating Kienböck disease is pain relief, wrist motion preservation, and preservation of grip strength.[rx]
Treatment of Kienböck disease depends on the stage of the disease and its causative factors. Stage I is always treated with splinting or cast immobilization. Stage II can also be treated with immobilization if necrosis is incomplete. Stages II with complete necrosis, III, and IV require “joint-leveling” surgery possibly coupled with vascular bone grafting or transfer of branches from adjacent arteries. Later stages with lunate collapse and secondary wrist degenerative arthrosis may also require proximal row corpectomy or intercarpal arthrodesis. Radial shortening osteotomy is the most common procedure performed to unload the lunate in cases with coexistent ulnar negative variance. Treatment may improve symptoms and functionality without affecting imaging findings in the advanced stages.[rx][rx][rx] Treatment usually depends on how early the disease is diagnosed. A physical therapist can advise on less painful ways to use the wrist.
Non-surgical options
- Resting the wrist – During the early stages, it might be possible to splint and cast the wrist for several months. Resting the wrist increases the chance of restoring blood flow to the lunate bone.
- Anti-inflammatory drugs – Ibuprofen, aspirin, and other painkillers may help manage swelling and pain during the early stages.
- Cortisone injections – These may help with symptoms. If over-the-counter (OTC) anti-inflammatory medications start to become less effective, the doctor may recommend surgery.
A physical therapist can teach the patient how to use the wrist in a way that is less painful and slows down the progression of the disease.
Do no HARM for 72 hours after injury
- Heat – Heat applied to fracture and injured side by hot baths, electric heat, saunas, heat packs, etc has the opposite effect on the blood flow. Heat may cause more fluid accumulation in the fracture joints by encouraging blood flow. Heat should be avoided when inflammation is developing in the acute stage. However, after about 72 hours, no further inflammation is likely to develop and heat can be soothing.
- Alcohol – stimulates the central nervous system that can increase bleeding and swelling and decrease healing.
- Running and movement – Running and walking may cause further damage, and causes healing delay.
- Massage – A massage also may increase bleeding and swelling. However, after 72 hours of your fracture, you can take a simple message, and applying heat may be soothing the pain.
Medication
The following medications may be considered by your doctor to relieve acute and immediate pain, long term treatment
- Antibiotic – Cefuroxime or Azithromycin, or Flucloxacillin or any other cephalosporin/quinolone, meropenem antibiotic must be used to prevent infection or clotted blood removal to prevent further swelling, inflammation, and edema.
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include first choice NSAIDs is Ketorolac, then Etoricoxib, then Aceclofenac, naproxen. As you are taking pain medication or NSAIDs, your doctor must prescribe a standard anti-ulcer drug, such as omeprazole, pantoprazole, esomeprazole, dexlansoprazole, etc.
- Muscle Relaxants – These medications provide relief from spinal muscle spasms, spasticity. Muscle relaxants, such as baclofen, tolperisone, eperisone, methocarbamol, carisoprodol, and cyclobenzaprine, may be prescribed to control postoperative muscle spasms, spasticity, stiffness, contracture.
- Calcium & vitamin D3 – To improve bone health, blood clotting, helping muscles to contract, regulating heart rhythms, nerve functions, and healing fractures. As a general rule, too absorbed more minerals for men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day to heal back pain, fractures, osteoarthritis.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, tingling sensation, and paresthesia.
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tighten the loose tendon, cartilage, ligament, and cartilage, ligament regenerates cartilage or inhabits the further degeneration of cartilage, ligament. The dosage of glucosamine is 15oo mg per day in divided dosage and chondroitin sulfate approximately 500mg per day in different dosages, and diacerein minimum of 50 mg per day may be taken if the patient suffers from osteoarthritis, rheumatoid arthritis, and any degenerative joint disease.[rx]
- Topical Medications and essential oil – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation in acute trauma, pain, swelling, tenderness through the skin. If the fracture is closed and not open fracture then you can use this item.
- Antidepressants – A drug that blocks pain messages from your brain and boosts the effects of endorphins in your body’s natural painkillers. It also helps in neuropathic pain, anxiety, tension, and proper sleep.
- Corticosteroids – Also known as oral steroids, these medications reduce inflammation. To heal the nerve inflammation and clotted blood in the joints.
- Dietary supplement – To eradicate the healing process from fracture your body needs a huge amount of vitamin C, and vitamin E. From your dietary supplement, you can get it, and also need to remove general weaknesses & improved health.
- Cough Syrup – If your doctor finds any chest congestion or fracture-related injury in your chest, dyspnoea, post-surgical breathing problem, then advice you to take bronchodilator cough syrup.
What To Eat and What to avoid
Eat Nutritiously During Your Recovery
All bones and tissues in the body need certain micronutrients in order to heal properly and in a timely manner. Eating a nutritious and balanced diet that includes lots of minerals and vitamins is proven to help heal broken bones and all types of fractures. Therefore, focus on eating lots of fresh food produce (fruits and veggies), whole grains, cereal, beans, lean meats, seafood, and fish to give your body the building blocks needed to properly repair your fracture. In addition, drink plenty of purified mineral water, milk, and other dairy-based beverages to augment what you eat.
- Broken bones or fractures bones need ample minerals (calcium, phosphorus, magnesium, boron, selenium, omega-3) and protein to become strong and healthy again.
- Excellent sources of minerals/protein include dairy products, tofu, beans, broccoli, nuts and seeds, sardines, sea fish, and salmon.
- Important vitamins that are needed for bone healing include vitamin C (needed to make collagen that your body essential element), vitamin D (crucial for mineral absorption, or machine for mineral absorber from your food), and vitamin K (binds calcium to bones and triggers more quickly collagen formation).
- Conversely, don’t consume food or drink that is known to impair bone/tissue healing, such as alcoholic beverages, sodas, fried fast food, most fast food items, and foods made with lots of refined sugars and preservatives.
Surgical procedures
Several different surgical procedures are available for patients with Kienböck’s disease.
The options depend on several factors, including the stage of the disease, the person’s activity level, and their personal goals.
- Revascularization – Revascularization involves restoring or increasing the blood supply to the lunate bone. The surgeon removes a portion of bone with all its attached blood vessels from another bone and inserts it into the lunate bone. This is possible during stages 1 and 2, before the bone deteriorates too far. An external fixator may be used to hold the bones stay in place while they heal. An external fixator is a metal device that is attached to the outside of the wrists, with pins that insert into the bone.
- Joint leveling – Joint leveling is an option when the two bones of the forearm, the radius, and the ulna, have different lengths. Bone grafts may be applied to lengthen the bone, or a section of bone is removed to shorten it. Joint leveling may stop the disease from progressing by reducing the forces that compress the lunate bone.
- Proximal row corpectomy – Proximal row corpectomy (PRC) involves the removal of the lunate bone and the two bones on either side of it. It is an option if the bone is broken into pieces or severely collapsed. If the lunate is severely collapsed or broken into pieces, it can be removed. In this procedure, the two bones on either side of the lunate are also removed. This procedure, called a proximal row corpectomy, will relieve pain while maintaining partial wrist motion.
- Joint leveling – If the two bones of the lower arm are not the same length, a joint leveling procedure may be recommended. Bones can be made longer using bone grafts or shortened by removing a section of the bone. This leveling procedure reduces the forces that compress the lunate and often stops the progression of the disease.
- Fusion – Fusion can be partial or complete. Partial fusion involves fusing some of the wrist bones together, effectively making one solid bone. This can reduce symptoms of pain and maintain some wrist motion. If the patient has severe arthritis of the wrist, the doctor may recommend fusing all the bones to reduce pain and improve wrist function. Wrist motion will be lost, but the patient will still be able to rotate their forearm.
- Implant arthroplasty – The lunate bone is replaced with a prosthetic replica made of a special, durable, pyrolytic carbon material while preserving the normal anatomy of the other bones. This is a relatively new procedure, so the long-term results are not yet known. Some patients may undergo several different procedures during their lifetime.
- Metaphyseal core decompression – In this procedure, the surgeon “scrapes off” part of the radius and ulna without actually removing any osseous tissue.[rx]
- Capitate-shortening osteotomy – A central bony wedge of the capitate is removed, followed by fusing the two remaining capitate bone segments.[rx]
- Total wrist joint replacement – (arthroplasty)[rx]
Prognosis of Avascular Necrosis of the Lunate
Kienbock disease is invariably progressive, and joint destruction occurs within 3-5 years of onset.[rx]
Prognosis depends on:
- Functional Staging – The greater the extent of viable bone, the better the prognosis.[rx]
- Negative ulnar variance – The greater the negative variance, the more severe the disease and the more likely it is to progress.[rx]
- Age at diagnosis – Patients diagnosed at an older age are more likely to have the advanced-stage disease and are more likely to progress.[rx]
It is significant to note that the severity of symptoms does not always correlate with the morphologic stage.