Conducting Zone of the respiratory tract is the subdivision of the respiratory system involved with the process of respiration in mammals. The respiratory tract is lined with respiratory mucosa or respiratory epithelium.[rx]
Air is breathed in through the nose to the nasal cavity, where a layer of nasal mucosa acts as a filter and traps pollutants and other harmful substances found in the air. Next, air moves into the pharynx, a passage that contains the intersection between the esophagus and the larynx. The opening of the larynx has a special flap of cartilage, the epiglottis, that opens to allow air to pass through but closes to prevent food from moving into the airway.
Nose and Paranasal Sinuses
The shape of the nose is determined by the ethmoid bone and the nasal septum.
KEY TAKEAWAYS
Key Points
- The shape of the nose is determined by the ethmoid bone and the nasal septum, which consists mostly of cartilage and separates the nostrils.
- The nose and paranasal sinuses are part of the upper respiratory tract.
- The functions of the nose include the sense of smell and conditioning of inhaled air by warming it and making it more humid.
- Hairs inside the nose prevent large particles from entering the lungs.
- Nasal mucosa and cilia help prevent pathogens and dust from reaching the lungs. Sneezing helps remove foreign particles that irritate the nasal mucosa.
- The paranasal sinuses are air-filled spaces around the nasal cavity that have many possible functions.
- The mucosa of the upper respiratory tract contain antimicrobial proteins that are a barrier component of the innate immune system.
Key Terms
- nostril: Either of the two orifices located on the nose (or on the beak of a bird); used as a passage for air and other gases to travel the nasal passages.
- paranasal sinuses: Four air-filled spaces around the nasal cavity that perform many functions, such as draining mucus from the nose.
The nose and paranasal sinuses form much of the upper respiratory tract, along with the pharynx. The upper respiratory tract is the entrance to the respiratory system, where air first enters the body. The overall function of the upper respiratory tract is to provide a pathway for air to reach the lower respiratory tract, where gas exchange occurs.
Anatomy and Physiology of the Nose

Internal diagram of the human nose: Air flows in through the nasal passage on the right and out through the nasopharynx on the posterior side.
The external part of the human nose is the protruding part of the face that bears the nostrils. The shape of the nose is determined by the ethmoid bone and the nasal septum.
The ethmoid bone is the bone that separates the nose from the brain and supports the shape and structure of the nasal and orbital cavities. The nasal septum is a wall of cartilage that separates the right and left nostril chambers from each other. On average, the nose of a male is larger than that of a female, due to differences in facial bone structure between genders.
The interior of the nasal cavity is lined with mucous membranes, nasal hairs, and cilia (microscopic hairs), that perform many of the specialized functions of the nose. The macroscopic nasal hairs prevent large particles from reaching the lungs, while the cilia and mucus trap pathogens and dust to take them to the pharynx, where they can be destroyed by digestion.
Another function of the nose is the conditioning of inhaled air, warming it and making it more humid. Sneezing occurs from irritation of the nasal mucus, which expels foreign particles, but can also spread microbial and viral infections between humans.
Finally, the nose has an area of specialized cells that are responsible for smelling, which is considered a nervous system function rather than a respiratory system function.
Anatomy and Physiology of the Paranasal Sinuses
The paranasal sinuses are a group of four, paired, air-filled spaces, lined with respiratory epithelium (ciliated columnar epithelium). These are named according to the bones within which the sinuses lie: surrounding the nasal cavity (maxillary sinuses), above the eyes (frontal sinuses), between the eyes (ethmoid sinuses), and behind the ethmoid bone (sphenoid sinuses).

Locations of the paranasal sinuses: The paranasal sinuses are four airspaces around the nasal cavity.
The functions of the sinuses are not fully understood, but there are many possible functions. The most important function is the sinuses’ role in draining mucus from the nasal cavity to the nasopharynx, which helps regulate pressure inside the nasal cavity. This may be a component of the barrier defenses of the innate immune system because of antimicrobial proteins found in the mucosa.
Other possible sinus functions include giving resonance to the voice, supporting the structure of the skull and facial bones, heating and humidifying inhaled air, and protecting the face from injury.
Pharynx
The human pharynx is part of the digestive system and also respiratory system.
KEY TAKEAWAYS
Key Points
- The human pharynx (plural: pharynges) is part of the digestive system and also respiratory system. It is situated immediately posterior to (behind) the mouth and nasal cavity, and superior to (above) the esophagus and larynx.
- The human pharynx is conventionally divided into three sections: the nasopharynx (epipharynx), the oropharynx (nasopharynx), and the laryngopharynx (hypopharynx).
- The Eustachian tubes connect the middle ear to the nasopharynx and serve to equalize the barometric pressure in the middle ear with that of the ambient atmosphere.
- Because both food and air pass through the pharynx, a flap of connective tissue called the epiglottis closes over the glottis when food is swallowed to prevent food from getting into the lungs.
- The laryngopharynx includes three major sites: the pyriform sinus, postcricoid area, and the posterior pharyngeal wall.
- Tonsils (lymphoid tissue) exist in the pharynx. Two of the major sets of tonsils are the adenoids in the nasopharynx and the palatine tonsils in the oropharynx.
- The oropharynx is the middle chamber of the pharynx that passes food from the mouth into the laryngopharynx. The nasopharynx opens above it as well.
- The laryngopharynx is the bottom part of the pharynx that marks the branching pathway between the digestive and respiratory systems.
Key Terms
- nasopharynx: The upper part of the pharynx that connects the nasal cavity to the throat.
- tonsils: Masses of lymphoid tissue found in the pharynx that play a small role in immune system function.
- laryngopharynx: The lower part of the pharynx above the larynx and below the oropharynx.
- oropharynx: The middle part of the pharynx that connects to the oral cavity and the other two chambers of the pharynx.
The Pharynx

The three main sections of the pharynx: This figure illustrates the three main subdivisions of the pharynx.
The human pharynx (plural: pharynges) is the part of the throat situated immediately posterior to the mouth and nasal cavity, and superior to the esophagus and larynx.
The human pharynx is divided into three sections: the nasopharynx (epipharynx), the oropharynx (mesopharynx), and the laryngopharynx (hypopharynx), which are all innervated by the pharyngeal plexus.
The pharynx is part of both the digestive system and the respiratory system. As a component of the upper respiratory tract, the pharynx is part of the conducting zone for air into the lungs. Therefore, one of its primary functions is to warm and humidify the air before it reaches the lungs.
The Nasopharynx

The Pharynx: This is a detailed diagram of the pharynx from Gray’s Anatomy, showing the major structures in each part of the pharynx.
The nasopharynx is the upper region of the pharynx. It extends from the base of the skull to the upper surface of the soft palate above the oral cavity. The nasopharynx connects the nasal cavity with the throat.
The nasopharynx connects to the eustachian tubes of the middle ear, which allows the nasopharynx to help balance pressure within the ear. However, it also allows infections to spread easily between the nasopharynx and ear. The nasopharynx contains pseudo-stratified squamous cell epithelial tissue that is ciliated (covered in tiny hairs that move mucus).
The adenoids (pharyngeal tonsils) are a mass of lymphatic tissue found in the roof of the nasopharynx. The adenoids play a minor role in embyonic development and have a minor role in producing T-lymphocytes for the immune system after birth.
The adenoids are often removed in childhood due to infection or hypertrophy (enlargement of the cells in its tissues), which can obstruct the flow of air from the nose to the lung if left untreated. While loss of the adenoids does not make a significant difference in immune system function, the procedure occasionally has complications.
The lateral walls of the nasopharynx are made of the pharyngeal Ostia (bone) of the auditory tube and supported by the torus Subarus, a mound of cartilage tissue from the auditory tube. Two folds arise from the cartilaginous opening of the auditory tube.
The salpingopharyngeal fold is a vertical fold of mucous membrane extending from the inferior part of the torus and is made up of salpingopharyngeus muscle. The salpingopalatine fold is a smaller fold extending from the superior part of the torus to the palate; it contains the levator veli palatini muscle.
Behind the bone of the auditory tube is a deep recess, the pharyngeal recess. Above the adenoid, in the midline, is an irregular flask-shaped depression of the mucous membrane called the pharyngeal bursa.
The Oropharynx
The oropharynx (nasopharynx) is the middle portion of the pharynx. It lies between the oral cavity, below the nasopharynx, and above the laryngopharynx, and has an opening to each of these other cavities. The anterior wall of the oropharynx consists of the base of the tongue and the superior wall consists of the bottom surface of the soft palate and the uvula.
The oropharynx is lined by non-keratinized squamous stratified epithelium, which is thicker than the epithelium found in other parts of the respiratory tract in order to prevent damage from food, but not as thick as skin as it lacks keratin.
The epiglottis lies between the oropharynx and the laryngopharynx, and it is a flap of elastic cartilage that closes during swallowing to ensure food enters the esophagus rather than the trachea.
The oropharynx contains the palatine tonsils, which are masses of lymphoid tissue found on the lateral walls of the oropharynx. Compared to the adenoids of the nasopharynx, the palatine tonsils contain many folds (called crypts), and aren’t ciliated like the adenoids are. These tonsils are also occasionally removed in people with infection or enlargement.
The Laryngopharynx
The laryngopharynx or hypopharynx is the caudal part of the pharynx; it is the part of the throat that connects to the esophagus and trachea. It lies inferior to the epiglottis and marks the division between the respiratory and digestive system pathways.
During swallowing, the epiglottis closes over the trachea and air passage temporarily stops. The laryngopharynx naturally continues into the esophagus tissue and is made up of a similar type of stratified squamous epithelium tissue.
The laryngopharynx itself has a few important demarcations and regions. The formal superior boundary that separates the laryngopharynx from the oropharynx is at the level of the hyoid bone.
The laryngopharynx includes three major regions: the pyriform sinus, the postcricoid area, and the posterior pharyngeal wall, which are separated by small folds of cartilage. Unlike the nasopharynx and oropharynx, there are no tonsils in the laryngopharynx.
Larynx
The larynx is an organ in the neck involved in breathing, sound production, and protecting the trachea against food aspiration.
KEY TAKEAWAYS
Key Points
- In adult humans, the larynx is found in the anterior neck at the level of the C3–C6 vertebrae and consists of nine cartilages: three single (epiglottic, thyroid, and cricoid) and three paired (arytenoid, corniculate, and cuneiform).
- Its interior can be divided in the supraglottis, glottis, and subglottis.
- The larynx houses the vocal folds—commonly but improperly termed the vocal cords. They are situated just below where the tract of the pharynx splits into the trachea and the esophagus; they are essential for phonation.
- The vocal folds are closed together by adducting the arytenoid cartilages so that they vibrate (see phonation).
- The vocal folds are controlled by the action of the vagus nerve.
- The larynx closes and rises during swallowing to move the epiglottis over the trachea.
- The larynx closes during a coughing reflex to protect the lungs from inhaling something that could damage it, and to remove foreign material from the trachea and lungs.
Key Terms
- vocal cords: Two folds of tissue located in the larynx that vibrates when air passes over them, producing the sound waves associated with talking and singing.
- cough reflex: This occurs when the larynx closes as it forces air out of the lungs to protect the lungs from aspirated materials.
- larynges: Part of the respiratory tract between the pharynx and the trachea, having walls of cartilage and muscle and containing the vocal cords enveloped in folds of mucous membrane.
The larynx (plural: larynges), commonly called the voice box, is an organ in the neck of humans and most animals that is involved in breathing, sound production, coughing, and protecting the trachea against food aspiration during eating.

External view of the larynx: This figure is a detailed view of the external aspect of the larynx.
Anatomy of the Larynx
In adult humans, the larynx is found in the anterior neck at the level of the C3–C6 vertebrae in the backbone. It connects the inferior part of the pharynx (laryngopharynx) with the trachea. The laryngeal skeleton consists of three single cartilages (thyroid, epiglottic, and cricoid).
- The thyroid cartilage is particularly notable for forming the Adam’s apple, the visible bulge made by the larynx when looking at the throat, and protects the larynx from injury.
- The epiglottic cartilage is the body of the epiglottis itself that connects to the larynx from above.
- The cricoid cartilage connects the larynx to the trachea from below.
There are also three sets of cartilages that are paired on either side of the larynx (arytenoid, corniculate, and cuneiform) that allow the position of the larynx to move during voice production.
The larynx connects to the hyoid bone (the bone that forms the floor of the mouth) from above. The larynx extends vertically from the tip of the epiglottis to the border of the cricoid cartilage that marks the formal beginning of the trachea.
The interior of the larynx consists of three regions, the supraglottis, glottis, and subglottis. The glottis is the midsection that contains the vocal folds (folds of muscular epithelium ), while the supraglottis and subglottis are the areas of the larynx that are above and below the glottis respectively. In newborn infants, the larynx is initially at the level of the C2–C3 vertebrae but descends as the child grows.
The glottis consists of two pairs of mucosal folds. These folds are false vocal folds (vestibular folds) and true vocal folds (folds). The false vocal folds are covered by respiratory epithelium, while the true vocal folds are covered by stratified squamous epithelium.
The false vocal folds are not responsible for sound production, but rather for resonance. These false vocal folds do not contain muscle, while the true vocal folds do have skeletal muscle. The two sets of folds are separated by the vocal ligament, with the false vocal folds above, and the true vocal cords below the ligament. The true vocal folds are often referred to as the vocal cords, however, the folds technically aren’t cords.
Physiology of the Larynx
The most notable and unique function of the larynx is phonation (voice production). The vocal folds of the larynx have two positions, open and closed. During breathing the folds remain open, but they close during swallowing or phonation.
When air from the lungs passes through closed folds during exhalation, the folds vibrate and create sound. The pitch produced depends on the length and tightness of the vocal folds.
The vagus nerves innervate the larynx and signal the muscles and paired cartilage (the arytenoid) of the larynx to work together to open and close the vocal folds as well as change their length and tension to alter pitch. Longer vocal folds have a lower pitch, which is part of the reason why men have deeper voices compared to women, because their larger larynxes have longer vocal folds.
Besides phonation, there are a few other important functions of the larynx. The folds of the larynx close and move upwards during swallowing, which causes the epiglottis to close off the trachea. This helps prevent aspiration of food into the lungs or choking from a blockage of food in the trachea.
The larynx closes off during coughing to help prevent harmful gasses from entering the lungs. During a cough reflex, air is forced out of the lungs, which can remove accumulated mucus, fluid, or blood from the lungs during injury, infection, or cancer of the lungs, as well as food or objects in the trachea during choking.
Finally, the larynx can be signaled to open its folds wider than usual to increase the flow of air into and out of the lungs during heavy breathing when the body requires more oxygen.
Structures Used in Voice Production
Voices produce sounds through a steady flow of air through the larynx, which causes vibrations and creates fluctuations in air pressure.
KEY TAKEAWAYS
Key Points
- The three basic mechanisms of voice production are air supply, vibration, and resonance.
- Pressure and air-flow speed through the larynx determine the strength and volume of voice.
- The articulation of consonants involves parts of the vocal tract obstructing phonation, and can be active or passive.
- A vowel is any articulation that comes from an open vocal tract.
- Vowel articulation depends mainly on the shape of the lips, the position of the tongue, but the shape of the vocal folds are involved as well.
Key Terms
- Resonance: The application of vibration by the structures of the upper respiratory tract, which can also influence the quality or tone of the sound.
- Articulation: The process by which raw phonation from the vocal cords is refined into specific sounds, such as consonants and vowels.
- glottis: An organ of speech located in the larynx and consisting of the true vocal cords and the opening between them.
Voice production is a complex process with many different layers and intricacies. The three basic mechanisms of voice production are air supply, vibration, and resonance.
Passive and active articulation shapes and refines phonation (vocal sound production) into the sounds and words used in communication. Voice production is an important physiological process because it enables complex communication between humans.
While the brain is responsible for higher organization and understanding language, the structures of the respiratory system are largely responsible for the production of sound itself.
Basic Mechanisms of Voice Production
Sound is produced by a combination of different structures of the respiratory system working together to create and resonate a sound. There are three basic mechanisms by which the human body produces a voice.
- Air Supply: In order for the voice to be produced, air must flow through the vocal folds. The supply of air for phonation comes from the lungs, and the speed and pressure by which it flows through the vocal folds is determined by the diaphragm. The speed of airflow also determines the strength and loudness of the voice.
- Vibration: The vocal folds in the glottis of the larynx vibrate as air passes through them. The vibration creates changes in air pressure that manifest as audible sound waves. They only vibrate if the vocal folds are in the closed position when the folds are held together by the movement of arytenoid cartilage. The pitch of the vibration depends on the length and tension of the vocal folds, which can be altered by muscle action.
- Resonance: The structures of the upper respiratory tract—particularly the soft palate of the mouth, the nasopharynx, and the paranasal sinuses —resonate and amplify the vibration of the vocal folds, making the sound louder and changing its tone. It works similarly to the way the sounding board of a guitar amplifies the vibration of the strings.
These basic mechanisms work together to create the voice. If they are altered, the produced voice will also be altered as well.
For example, during loud voice production, such as shouting or singing, a greater air supply and greater pressure for the flow of air through the vocal folds is required to produce the louder sound. The diaphragm must contract harder to support this greater flow of air compared to normal speech.
Similarly, whispering takes less air compared to normal speech, because the sound produced during whispering is much weaker in comparison.
Articulation
Articulation is the process by which phonation is refined into the specific consonants and vowels used to form words. The articulation of consonants occurs at a point of either active or passive articulation, which is a place in the vocal tract where an obstruction stops the sound.
After the sound is obstructed, the pressure from the air builds based on the shape of that obstruction, which changes the sound into the form it is vocalized as. Vowels are articulated sounds that do not come from obstruction, and instead come from an open vocal tract.
Passive Place of Articulation
The passive place of articulation is the place on the more stationary part of the vocal tract where the articulation occurs. It can be anywhere from the lips, upper teeth, gums, roof of the mouth, or the back of the throat. These areas are passive because no specific action or activity is involved within that area to pronounce the consonant.
Passive articulation is considered a continuum because the obstruction of many different places is needed to produce most of the consonants. There are also several different combinations of areas that can produce the same consonant; for example, many languages may distinguish consonants by articulating them in different areas. Passive places of articulation include:
- The upper lip (labial).
- The upper teeth, either on the edge of the teeth or inner surface (dental).
- The alveolar ridge, the gum line just behind the teeth (alveolar).
- The back of the alveolar ridge (post-alveolar).
- The hard palate on the roof of the mouth (palatal).
- The soft palate further back on the roof of the mouth (velar).
- The uvula hanging down at the entrance to the throat (uvular).
- The throat itself, also known as the pharynx (pharyngeal).
- The epiglottis at the entrance to the windpipe, above the voice box (epiglottal).
Active Place of Articulation
The articulatory gesture of the active place of articulation involves the more mobile part of the vocal tract. This is typically some part of the tongue or lips. It is considered active because these areas change the consonant pronounced by moving or changing.
The active places of articulation are not considered a continuum (unlike passive articulation) because they work independently of each other, but they have the capacity to work together for certain consonants. Active places of articulation include:
- The lower lip (labial).
- Various parts of the front of the tongue.
- The back of the tongue. The aryepiglottic folds at the entrance to the larynx (also epiglottal).
- The glottis (laryngeal).
Vowels
A vowel is a sound that comes from an open vocal tract, and does involve strict obstruction of the sound as with consonants. Therefore, there is more variation in the mechanisms used to create vowels compared to consonants. Vowels are mainly articulated by the shape of the lips, the position of the tongue (both vertical and horizontal), and by the phonation of the larynx itself.

Places of articulation for voice production: Places of articulation (active and passive): 1. Exo-labial (outer part of lip), 2. Endo-labial (inner part of lip), 3. Dental (teeth), 4. Alveolar (front part of alveolar ridge), 5. Post-alveolar (rear part of alveolar ridge & slightly behind it), 6. Pre-palatal (front part of hard palate that arches upward), 7. Palatal (hard palate), 8. Velar (soft palate), 9. Uvular (a.k.a. Post-velar; uvula), 10. Pharyngeal (pharyngeal wall), 11. Glottal (a.k.a. Laryngeal; vocal folds), 12. Epiglottal (epiglottis), 13. Radical (tongue root), 14. Postero-dorsal (back of tongue body), 15. Antero-dorsal (front of tongue body), 16. Laminal (tongue blade), 17. Apical (apex or tongue tip), and 18. Sub-laminal (also known as sub-apical; underside of tongue)
Trachea
The trachea, or windpipe, is a tube that connects the pharynx or larynx to the lungs, allowing the passage of air.
KEY TAKEAWAYS
Key Points
- The trachea is lined with pseudostratified ciliated columnar epithelium cells with goblet cells that produce mucus.
- There are about 15 to 20 C-shaped cartilaginous rings that reinforce the anterior and lateral sides of the trachea to protect and maintain the airway, leaving a membranous wall (pars membranacea) dorsally without cartilage where the C-shape is open.
- The cartilaginous rings are C-shaped to allow the trachea to collapse slightly at the opening so that food can pass down the esophagus.
- The trachealis muscle connects the ends of the open part of the C-shaped rings and contracts during coughing, reducing the size of the lumen of the trachea to increase the airflow rate.
- The esophagus lies posteriorly to the trachea.
- The mucociliary escalator helps prevent pathogens from entering the lungs.
- The trachea is part of the conducting zone and contributes to anatomical dead space.
Key Terms
- cilia: Tiny, hair-like projections from a cell.
- mucociliary escalator: The ladder formed by mucus and cilia in the trachea that pushes mucus up the trachea and into the pharynx to prevent mucus pathogens from entering the lungs.
- anatomical dead space: The space in the respiratory tract that isn’t involved in alveolar ventilation and is part of the normal conducting zone of the respiratory system.

The trachea: This is the trachea in relation to the rest of the respiratory system.
The trachea, or windpipe, is a tube that connects the pharynx or larynx to the lungs, allowing the passage of air. It is lined with pseudostratified ciliated columnar epithelium cells with goblet cells that produce mucus. The trachea is part of the conducting zone for air into and out of the lungs.
Anatomy of the Trachea
The trachea is a long tube that extends from the pharynx and larynx to the bronchi of the lungs. It typically has an inner diameter of about 25.4 millimeters (1.00 in) and a length of about 10 to 16 centimeters.
The trachea commences at the lower border of the larynx, level with the sixth cervical vertebra, and bifurcates into the primary bronchi at the vertebral level of thoracic vertebra T5, or up to two vertebrae lower or higher, depending on breathing.
At the top of the trachea and bottom of the larynx is the cricoid cartilage, the only complete ring of cartilage in the trachea. Extending downward throughout the length of the tube are about fifteen to 20 C-shaped cartilaginous rings that reinforce the outer structure and shape of the trachea—the open part of each C-shaped ring reveals a membranous wall on the inside of the trachea.

Histology of the Trachea: A cross section of the trachea, showing the hyaline cartilage, mucus glands, and ciliated epithelium.
The cartilage of the trachea is considered hyaline cartilage: simple, transparent, and made primarily of collagen. The trachealis muscle connects the open ends of the C-shaped rings of cartilage and contracts during coughing, reducing the size of the lumen of the trachea to increase the air flow rate.
The esophagus lies behind the trachea. The C-shaped cartilaginous rings allow the trachea to collapse slightly at its opening, so food can pass down the esophagus after swallowing.
The epiglottis closes the opening to the larynx during swallowing to prevent swallowed matter from entering the trachea.
Physiology of the Trachea
This mucus and cilia of the trachea from the mucociliary escalator, which lines the cells of the trachea with mucus to trap inhaled foreign particles. The cilia then waft upward toward the larynx and the pharynx, where it can be either swallowed into the stomach (and destroyed by acid) or expelled as phlegm.
The mucociliary escalator is one of the most important functions of the trachea and is also considered a barrier component of the immune system due to its role in preventing pathogens from entering the lungs. The epithelium and the mucociliary ladder can be damaged by smoking tobacco and alcohol consumption, which can make pneumonia (an infection of the alveoli of the lungs) from bacteria in the upper respiratory tract more likely to occur due to the loss of barrier function.
As a part of the conducting zone of the lungs, the trachea is important in warming and moistening air before it reaches the lungs. The trachea is also considered a part of normal anatomical dead space (space in the airway that isn’t involved in alveolar gas exchange) and its volume contributes to calculations of ventilation and physiological (total) dead space. It is not considered alveolar dead space, a term that refers to alveoli that don’t partake in gas exchange due to damage or lack of blood supply.
Or
Organs and Structures of the Respiratory System
By the end of this section, you will be able to:
- List the structures that make up the respiratory system
- Describe how the respiratory system processes oxygen and CO2
- Compare and contrast the functions of upper respiratory tract with the lower respiratory tract
The major organs of the respiratory system function primarily to provide oxygen to body tissues for cellular respiration, remove the waste product carbon dioxide, and help to maintain acid-base balance. Portions of the respiratory system are also used for non-vital functions, such as sensing odors, speech production, and for straining, such as during childbirth or coughing.

Figure 1. The major respiratory structures span the nasal cavity to the diaphragm.
Functionally, the respiratory system can be divided into a conducting zone and a respiratory zone. The conducting zone of the respiratory system includes the organs and structures not directly involved in gas exchange. The gas exchange occurs in the respiratory zone.
Conducting Zone
The major functions of the conducting zone are to provide a route for incoming and outgoing air, remove debris and pathogens from the incoming air, and warm and humidify the incoming air. Several structures within the conducting zone perform other functions as well. The epithelium of the nasal passages, for example, is essential to sensing odors, and the bronchial epithelium that lines the lungs can metabolize some airborne carcinogens.
The Nose and its Adjacent Structures
The major entrance and exit for the respiratory system is through the nose. When discussing the nose, it is helpful to divide it into two major sections: the external nose, and the nasal cavity or internal nose.
The external nose consists of the surface and skeletal structures that result in the outward appearance of the nose and contribute to its numerous functions. The root is the region of the nose located between the eyebrows. The bridge is the part of the nose that connects the root to the rest of the nose. The dorsum nasi is the length of the nose. The apex is the tip of the nose. On either side of the apex, the nostrils are formed by the alae (singular = ala). An ala is a cartilaginous structure that forms the lateral side of each naris (plural = nares), or nostril opening. The philtrum is the concave surface that connects the apex of the nose to the upper lip.
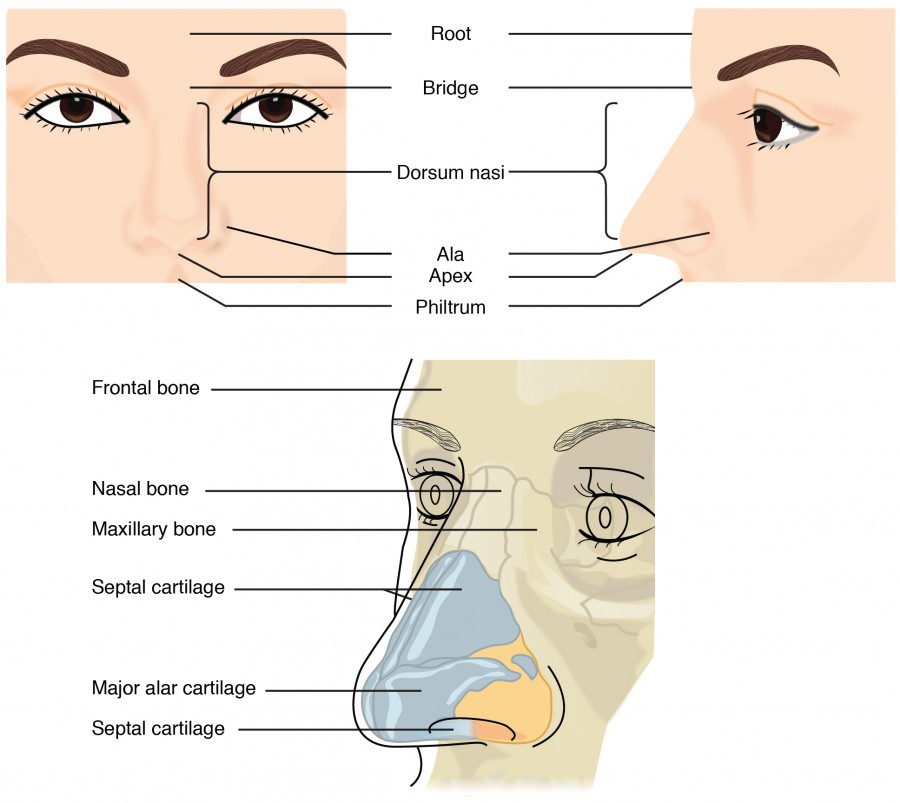
Figure 2. This illustration shows features of the external nose (top) and skeletal features of the nose (bottom).
Underneath the thin skin of the nose are its skeletal features. While the root and bridge of the nose consist of bone, the protruding portion of the nose is composed of cartilage. As a result, when looking at a skull, the nose is missing. The nasal bone is one of a pair of bones that lies under the root and bridge of the nose. The nasal bone articulates superiorly with the frontal bone and laterally with the maxillary bones. Septal cartilage is flexible hyaline cartilage connected to the nasal bone, forming the dorsum nasi. The alar cartilage consists of the apex of the nose; it surrounds the naris.

Figure 3. Upper Airway
The nares open into the nasal cavity, which is separated into left and right sections by the nasal septum. The nasal septum is formed anteriorly by a portion of the septal cartilage (the flexible portion you can touch with your fingers) and posteriorly by the perpendicular plate of the ethmoid bone (a cranial bone located just posterior to the nasal bones) and the thin vomer bones (whose name refers to its plough shape). Each lateral wall of the nasal cavity has three bony projections, called the superior, middle, and inferior nasal conchae. The inferior conchae are separate bones, whereas the superior and middle conchae are portions of the ethmoid bone. Conchae serve to increase the surface area of the nasal cavity and to disrupt the flow of air as it enters the nose, causing air to bounce along the epithelium, where it is cleaned and warmed. The conchae and meatuses also conserve water and prevent dehydration of the nasal epithelium by trapping water during exhalation. The floor of the nasal cavity is composed of the palate. The hard palate at the anterior region of the nasal cavity is composed of bone. The soft palate at the posterior portion of the nasal cavity consists of muscle tissue. Air exits the nasal cavities via the internal nares and moves into the pharynx.
Several bones that help form the walls of the nasal cavity have air-containing spaces called the paranasal sinuses, which serve to warm and humidify incoming air. Sinuses are lined with a mucosa. Each paranasal sinus is named for its associated bone: frontal sinus, maxillary sinus, sphenoidal sinus, and ethmoidal sinus. The sinuses produce mucus and lighten the weight of the skull.
The nares and anterior portion of the nasal cavities are lined with mucous membranes, containing sebaceous glands and hair follicles that serve to prevent the passage of large debris, such as dirt, through the nasal cavity. An olfactory epithelium used to detect odors is found deeper in the nasal cavity.
The conchae, meatuses, and paranasal sinuses are lined by respiratory epithelium composed of pseudostratified ciliated columnar epithelium. The epithelium contains goblet cells, one of the specialized, columnar epithelial cells that produce mucus to trap debris. The cilia of the respiratory epithelium help remove the mucus and debris from the nasal cavity with a constant beating motion, sweeping materials towards the throat to be swallowed. Interestingly, cold air slows the movement of the cilia, resulting in accumulation of mucus that may in turn lead to a runny nose during cold weather. This moist epithelium functions to warm and humidify incoming air. Capillaries located just beneath the nasal epithelium warm the air by convection. Serous and mucus-producing cells also secrete the lysozyme enzyme and proteins called defensins, which have antibacterial properties. Immune cells that patrol the connective tissue deep to the respiratory epithelium provide additional protection.

Figure 4. Respiratory epithelium is the pseudostratified ciliated columnar epithelium. Seromucous glands provide lubricating mucus. LM × 680. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Pharynx
The pharynx is a tube formed by skeletal muscle and lined by mucous membrane that is continuous with that of the nasal cavities. The pharynx is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx.
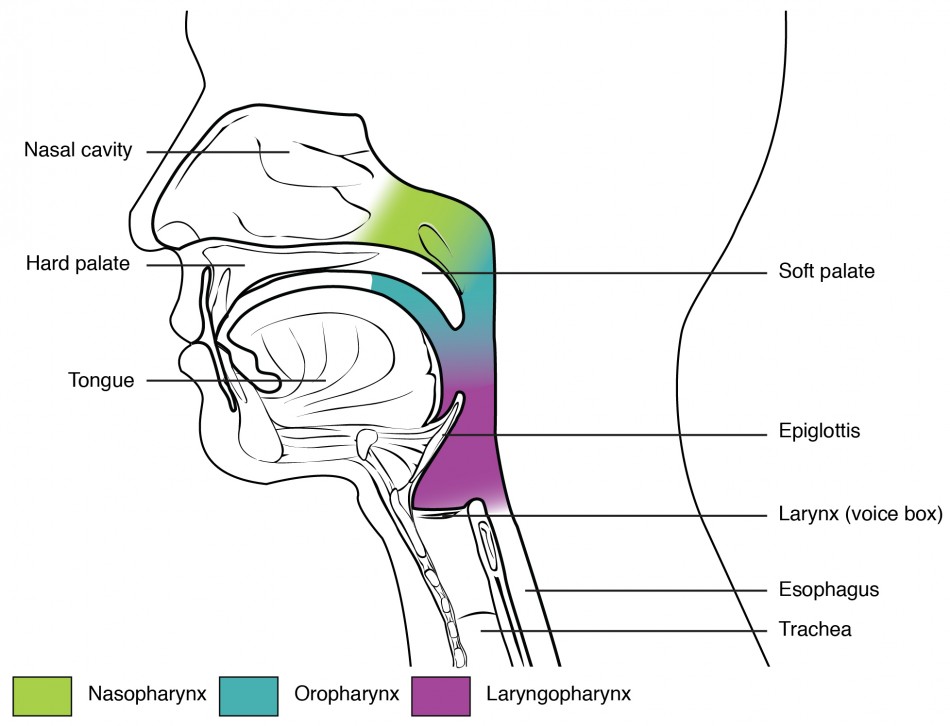
Figure 5. The pharynx is divided into three regions: the nasopharynx, the oropharynx, and the laryngopharynx.
The nasopharynx is flanked by the conchae of the nasal cavity, and it serves only as an airway. At the top of the nasopharynx are the pharyngeal tonsils. A pharyngeal tonsil, also called an adenoid, is an aggregate of lymphoid reticular tissue similar to a lymph node that lies at the superior portion of the nasopharynx. The function of the pharyngeal tonsil is not well understood, but it contains a rich supply of lymphocytes and is covered with ciliated epithelium that traps and destroys invading pathogens that enter during inhalation. The pharyngeal tonsils are large in children, but interestingly, tend to regress with age and may even disappear. The uvula is a small bulbous, teardrop-shaped structure located at the apex of the soft palate. Both the uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx to prevent ingested materials from entering the nasal cavity. In addition, auditory (Eustachian) tubes that connect to each middle ear cavity open into the nasopharynx. This connection is why colds often lead to ear infections.
The oropharynx is a passageway for both air and food. The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. The fauces is the opening at the connection between the oral cavity and the oropharynx. As the nasopharynx becomes the oropharynx, the epithelium changes from pseudostratified ciliated columnar epithelium to stratified squamous epithelium. The oropharynx contains two distinct sets of tonsils, the palatine and lingual tonsils. A palatine tonsil is one of a pair of structures located laterally in the oropharynx in the area of the fauces. The lingual tonsil is located at the base of the tongue. Similar to the pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid tissue, and trap and destroy pathogens entering the body through the oral or nasal cavities.
The laryngopharynx is inferior to the oropharynx and posterior to the larynx. It continues the route for ingested material and air until its inferior end, where the digestive and respiratory systems diverge. The stratified squamous epithelium of the oropharynx is continuous with the laryngopharynx. Anteriorly, the laryngopharynx opens into the larynx, whereas posteriorly, it enters the esophagus.
Larynx
The larynx is a cartilaginous structure inferior to the laryngopharynx that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs. The structure of the larynx is formed by several pieces of cartilage. Three large cartilage pieces—the thyroid cartilage (anterior), epiglottis (superior), and cricoid cartilage (inferior)—form the major structure of the larynx. The thyroid cartilage is the largest piece of cartilage that makes up the larynx. The thyroid cartilage consists of the laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in males. The thick cricoid cartilage forms a ring, with a wide posterior region and a thinner anterior region. Three smaller, paired cartilages—the arytenoids, corniculate, and cuneiforms—attach to the epiglottis and the vocal cords and muscles that help move the vocal cords to produce speech.

Figure 6. The larynx extends from the laryngopharynx and the hyoid bone to the trachea.

Figure 7. The true vocal cords and vestibular folds of the larynx are viewed inferiorly from the laryngopharynx.
The epiglottis, attached to the thyroid cartilage, is a very flexible piece of elastic cartilage that covers the opening of the trachea. When in the “closed” position, the unattached end of the epiglottis rests on the glottis. The glottis is composed of the vestibular folds, the true vocal cords, and the space between these folds. A vestibular fold, or false vocal cord, is one of a pair of folded sections of the mucous membrane. A true vocal cord is one of the white, membranous folds attached by muscle to the thyroid and arytenoid cartilages of the larynx on their outer edges. The inner edges of the true vocal cords are free, allowing oscillation to produce sound. The size of the membranous folds of the true vocal cords differs between individuals, producing voices with different pitch ranges. Folds in males tend to be larger than those in females, which creates a deeper voice. The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea. These movements produce a larger area for food to pass through while preventing food and beverages from entering the trachea.
Continuous with the laryngopharynx, the superior portion of the larynx is lined with stratified squamous epithelium, transitioning into pseudostratified ciliated columnar epithelium that contains goblet cells. Similar to the nasal cavity and nasopharynx, this specialized epithelium produces mucus to trap debris and pathogens as they enter the trachea. The cilia beat the mucus upward towards the laryngopharynx, where it can be swallowed down the esophagus.
Trachea
The trachea (windpipe) extends from the larynx toward the lungs. The trachea is formed by 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are connected by dense connective tissue. The trachealis muscle and elastic connective tissue together form the fibroelastic membrane, a flexible membrane that closes the posterior surface of the trachea, connecting the C-shaped cartilages. The fibroelastic membrane allows the trachea to stretch and expand slightly during inhalation and exhalation, whereas the rings of cartilage provide structural support and prevent the trachea from collapsing. In addition, the trachealis muscle can be contracted to force air through the trachea during exhalation. The trachea is lined with pseudostratified ciliated columnar epithelium, which is continuous with the larynx. The esophagus borders the trachea posteriorly.

Figure 8. (a) The tracheal tube is formed by stacked, C-shaped pieces of hyaline cartilage. (b) The layer visible in this cross-section of tracheal wall tissue between the hyaline cartilage and the lumen of the trachea is the mucosa, which is composed of pseudostratified ciliated columnar epithelium that contains goblet cells. LM × 1220. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Bronchial Tree
The trachea branches into the right and left primary bronchi at the carina. These bronchi are also lined by pseudostratified ciliated columnar epithelium containing mucus-producing goblet cells. The carina is a raised structure that contains specialized nervous tissue that induces violent coughing if a foreign body, such as food, is present. Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent their collapse. The primary bronchi enter the lungs at the hilum, a concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs. The bronchi continue to branch into the bronchial a tree. A bronchial tree (or respiratory tree) is the collective term used for these multiple-branched bronchi. The main function of the bronchi, like other conducting zone structures, is to provide a passageway for air to move into and out of each lung. In addition, the mucous membrane traps debris and pathogens.
A bronchiole branches from the tertiary bronchi. Bronchioles, which are about 1 mm in diameter, further branch until they become the tiny terminal bronchioles, which lead to the structures of gas exchange. There are more than 1000 terminal bronchioles in each lung. The muscular walls of the bronchioles do not contain cartilage-like those of the bronchi. This muscular wall can change the size of the tubing to increase or decrease airflow through the tube.
Respiratory Zone
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole, which then leads to an alveolar duct, opening into a cluster of alveoli.

Figure 9. Bronchioles lead to alveolar sacs in the respiratory zone, where gas exchange occurs.
Alveoli
An alveolar duct is a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts.
An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange. An alveolus is approximately 200 mm in diameter with elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange. Alveoli are connected to their neighbors by alveolar pores, which help maintain equal air pressure throughout the alveoli and lung.

Figure 10. (a) The alveolus is responsible for gas exchange. (b) A micrograph shows the alveolar structures within lung tissue. LM × 178. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
The alveolar wall consists of three major cell types: type I alveolar cells, type II alveolar cells, and alveolar macrophages. A type I alveolar cell is a squamous epithelial cell of the alveoli, which constitutes up to 97 percent of the alveolar surface area. These cells are about 25 nm thick and are highly permeable to gases. A type II alveolar cell is interspersed among the type I cells and secretes pulmonary surfactant, a substance composed of phospholipids and proteins that reduces the surface tension of the alveoli. Roaming around the alveolar wall is the alveolar macrophage, a phagocytic cell of the immune system that removes debris and pathogens that have reached the alveoli.
The simple squamous epithelium formed by type I alveolar cells is attached to a thin, elastic basement membrane. This epithelium is extremely thin and borders the endothelial membrane of capillaries. Taken together, the alveoli and capillary membranes form a respiratory membrane that is approximately 0.5 mm thick. The respiratory membrane allows gases to cross by simple diffusion, allowing oxygen to be picked up by the blood for transport and CO2 to be released into the air of the alveoli.
DISEASES OF THE RESPIRATORY SYSTEM: ASTHMA
Asthma is a common condition that affects the lungs in both adults and children. Approximately 8.2 percent of adults (18.7 million) and 9.4 percent of children (7 million) in the United States suffer from asthma. In addition, asthma is the most frequent cause of hospitalization in children.
Asthma is a chronic disease characterized by inflammation and edema of the airway, and bronchospasms (that is, constriction of the bronchioles), which can inhibit air from entering the lungs. In addition, excessive mucus secretion can occur, which further contributes to airway occlusion. Cells of the immune system, such as eosinophils and mononuclear cells, may also be involved in infiltrating the walls of the bronchi and bronchioles.
Bronchospasms occur periodically and lead to an “asthma attack.” An attack may be triggered by environmental factors such as dust, pollen, pet hair, or dander, changes in the weather, mold, tobacco smoke, and respiratory infections, or by exercise and stress.

Figure 11. (a) Normal lung tissue does not have the characteristics of lung tissue during (b) an asthma attack, which include thickened mucosa, increased mucus-producing goblet cells, and eosinophil infiltrates.
Symptoms of an asthma attack involve coughing, shortness of breath, wheezing, and tightness of the chest. Symptoms of a severe asthma attack that requires immediate medical attention would include difficulty breathing that results in blue (cyanotic) lips or face, confusion, drowsiness, a rapid pulse, sweating, and severe anxiety. The severity of the condition, frequency of attacks, and identified triggers influence the type of medication that an individual may require. Longer-term treatments are used for those with more severe asthma. Short-term, fast-acting drugs that are used to treat an asthma attack are typically administered via an inhaler. For young children or individuals who have difficulty using an inhaler, asthma medications can be administered via a nebulizer.
In many cases, the underlying cause of the condition is unknown. However, recent research has demonstrated that certain viruses, such as human rhinovirus C (HRVC), and the bacteria Mycoplasma pneumoniae and Chlamydia pneumoniae that are contracted in infancy or early childhood, may contribute to the development of many cases of asthma.
PRACTICE QUESTION
Watch this video to learn more about what happens during an asthma attack. What are the three changes that occur inside the airways during an asthma attack?
Chapter Review
The respiratory system is responsible for obtaining oxygen and getting rid of carbon dioxide and aiding in speech production and in sensing odors. From a functional perspective, the respiratory system can be divided into two major areas: the conducting zone and the respiratory zone. The conducting zone consists of all of the structures that provide passageways for air to travel into and out of the lungs: the nasal cavity, pharynx, trachea, bronchi, and most bronchioles. The nasal passages contain the conchae and meatuses that expand the surface area of the cavity, which helps to warm and humidify incoming air, while removing debris and pathogens. The pharynx is composed of three major sections: the nasopharynx, which is continuous with the nasal cavity; the oropharynx, which borders the nasopharynx and the oral cavity; and the laryngopharynx, which borders the oropharynx, trachea, and esophagus. The respiratory zone includes the structures of the lung that are directly involved in gas exchange: the terminal bronchioles and alveoli.
The lining of the conducting zone is composed mostly of pseudostratified ciliated columnar epithelium with goblet cells. The mucus traps pathogens and debris, whereas beating cilia move the mucus superiorly toward the throat, where it is swallowed. As the bronchioles become smaller and smaller, and nearer the alveoli, the epithelium thins and is simple squamous epithelium in the alveoli. The endothelium of the surrounding capillaries, together with the alveolar epithelium, forms the respiratory membrane. This is a blood-air barrier through which gas exchange occurs by simple diffusion.
Self Check
Answer the question(s) below to see how well you understand the topics covered in the previous section.
CRITICAL THINKING QUESTIONS
- Describe the three regions of the pharynx and their functions.
- If a person sustains an injury to the epiglottis, what would be the physiological result?
- Compare and contrast the conducting and respiratory zones.
Glossary
ala: (plural = alae) small, flaring structure of a nostril that forms the lateral side of the nares
alar cartilage: cartilage that supports the apex of the nose and helps shape the nares; it is connected to the septal cartilage and connective tissue of the alae
alveolar duct: small tube that leads from the terminal bronchiole to the respiratory bronchiole and is the point of attachment for alveoli
alveolar macrophage: immune system cell of the alveolus that removes debris and pathogens
alveolar pore: opening that allows airflow between neighboring alveoli
alveolar sac: cluster of alveoli
alveolus: small, grape-like sac that performs gas exchange in the lungs
apex: tip of the external nose
bronchial tree: collective name for the multiple branches of the bronchi and bronchioles of the respiratory system
bridge: portion of the external nose that lies in the area of the nasal bones
bronchiole: branch of bronchi that are 1 mm or less in diameter and terminate at alveolar sacs
bronchus: tube connected to the trachea that branches into many subsidiaries and provides a passageway for air to enter and leave the lungs
conducting zone: region of the respiratory system that includes the organs and structures that provide passageways for air and are not directly involved in gas exchange
cricoid cartilage: portion of the larynx composed of a ring of cartilage with a wide posterior region and a thinner anterior region; attached to the esophagus
dorsum nasi: intermediate portion of the external nose that connects the bridge to the apex and is supported by the nasal bone
epiglottis: leaf-shaped piece of elastic cartilage that is a portion of the larynx that swings to close the trachea during swallowing
external nose: region of the nose that is easily visible to others
fauces: portion of the posterior oral cavity that connects the oral cavity to the oropharynx
fibroelastic membrane: specialized membrane that connects the ends of the C-shape cartilage in the trachea; contains smooth muscle fibers
glottis: opening between the vocal folds through which air passes when producing speech
laryngeal prominence: region where the two lamina of the thyroid cartilage join, forming a protrusion known as “Adam’s apple”
laryngopharynx: portion of the pharynx bordered by the oropharynx superiorly and esophagus and trachea inferiorly; serves as a route for both air and food
larynx: cartilaginous structure that produces the voice, prevents food and beverages from entering the trachea, and regulates the volume of air that enters and leaves the lungs
lingual tonsil: lymphoid tissue located at the base of the tongue
meatus: one of three recesses (superior, middle, and inferior) in the nasal cavity attached to the conchae that increase the surface area of the nasal cavity
naris: (plural = nares) opening of the nostrils
nasal bone: bone of the skull that lies under the root and bridge of the nose and is connected to the frontal and maxillary bones
nasal septum: wall composed of bone and cartilage that separates the left and right nasal cavities
nasopharynx: portion of the pharynx flanked by the conchae and oropharynx that serves as an airway
oropharynx: portion of the pharynx flanked by the nasopharynx, oral cavity, and laryngopharynx that is a passageway for both air and food
palatine tonsil: one of the paired structures composed of lymphoid tissue located anterior to the uvula at the roof of isthmus of the fauces
paranasal sinus: one of the cavities within the skull that is connected to the conchae that serve to warm and humidify incoming air, produce mucus, and lighten the weight of the skull; consists of frontal, maxillary, sphenoidal, and ethmoidal sinuses
pharyngeal tonsil: structure composed of lymphoid tissue located in the nasopharynx
pharynx: region of the conducting zone that forms a tube of skeletal muscle lined with respiratory epithelium; located between the nasal conchae and the esophagus and trachea
philtrum: concave surface of the face that connects the apex of the nose to the top lip
pulmonary surfactant: substance composed of phospholipids and proteins that reduces the surface tension of the alveoli; made by type II alveolar cells
respiratory bronchiole: specific type of bronchiole that leads to alveolar sacs
respiratory epithelium: ciliated lining of much of the conducting zone that is specialized to remove debris and pathogens, and produce mucus
respiratory membrane: alveolar and capillary wall together, which form an air-blood barrier that facilitates the simple diffusion of gases
respiratory zone: includes structures of the respiratory system that are directly involved in gas exchange
root: region of the external nose between the eyebrows
thyroid cartilage: largest piece of cartilage that makes up the larynx and consists of two lamina
trachea: tube composed of cartilaginous rings and supporting tissue that connects the lung bronchi and the larynx; provides a route for air to enter and exit the lung
trachealis muscle: smooth muscle located in the fibroelastic membrane of the trachea
true vocal cord: one of the pair of folded, white membranes that have a free inner edge that oscillates as air passes through to produce sound
type I alveolar cell: squamous epithelial cells that are the major cell type in the alveolar wall; highly permeable to gases
type II alveolar cell: cuboidal epithelial cells that are the minor cell type in the alveolar wall; secrete pulmonary surfactant
vestibular fold: part of the folded region of the glottis composed of mucous membrane; supports the epiglottis during swallowing
References