The autonomic nervous system is a component of the peripheral nervous system that regulates involuntary physiologic processes including heart rate, blood pressure, respiration, digestion, and sexual arousal. It contains three anatomically distinct divisions: sympathetic, parasympathetic, and enteric.
The autonomic nervous system (ANS) is made up of pathways of neurons that control various organ systems inside the body, using many diverse chemicals and signals to maintain homeostasis. It divides into the sympathetic and parasympathetic systems. The sympathetic component is better known as “fight or flight” and the parasympathetic component is “rest and digest.” It functions without conscious control throughout the lifespan of an organism to control cardiac muscle, smooth muscle, and exocrine and endocrine glands, which in turn regulate blood pressure, urination, bowel movements, and thermoregulation.[rx]
Organ Systems Involved
The autonomic nervous system exerts influence over the organ systems of the body to upregulate and downregulate various functions. The two aspects of the ANS operate as opposing functions that act to achieve homeostasis. This next section will discuss this in terms of its divisions, the sympathetic and parasympathetic nervous systems.
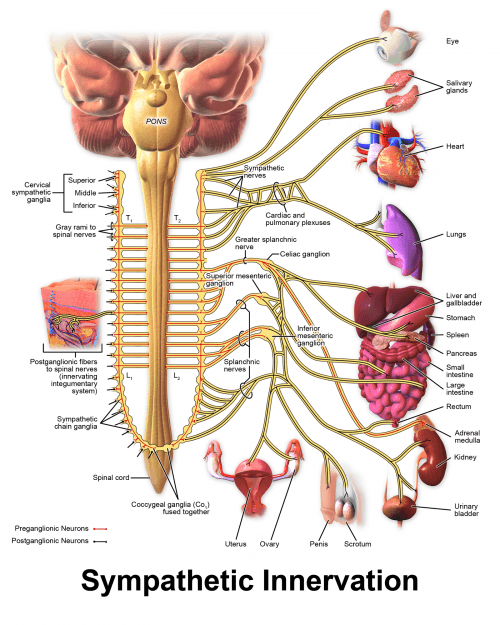
The sympathetic nervous system, also known as the “fight or flight” system, increases energy expenditure and inhibits digestion. The following changes take place on activation of the sympathetic nervous system:
-
Heart rate and cardiac muscle contractility increase
-
The ciliary muscle relaxes, and the pupil becomes dilated for the betterment of far vision.
-
Bronchodilation of the lungs
-
Decreased GI motility
-
Decreased urine output
-
Relaxation of the detrusor muscle of the bladder and contraction of urethral sphincters
-
Increased secretions from sweat glands
-
Increased blood flow to muscles because of relaxation of arterioles
-
Dilation of coronary arteries
-
Constriction of large arteries and large veins
-
Increased metabolism
-
Increased glucose production and mobilization by the liver
-
Increased lipolysis within fat tissue, ejaculation
-
Suppression of the immune system
These changes function to increase movement and strength. Stressful situations that threaten survival, exercise, or the moments just before wakening are just a few examples of increases in sympathetic nervous system activity.[4]
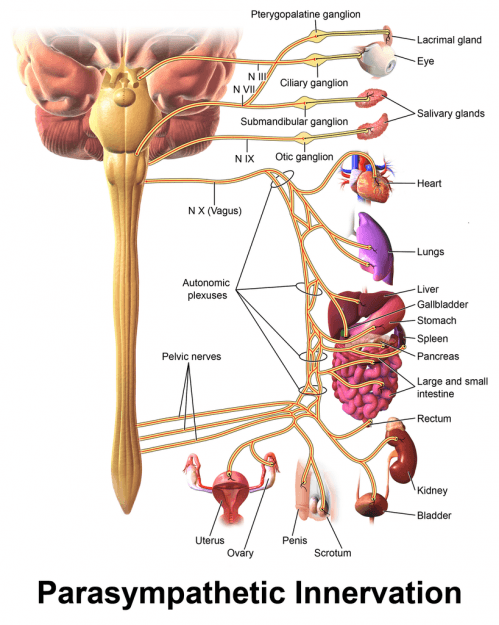
The parasympathetic nervous system, also known as “rest and digest,” can be thought of as functioning in opposition to the sympathetic nervous system. Its functions include:
-
A decrease in heart rate and contractility of cardiac muscle
-
Constriction of the ciliary muscle and the pupil for near vision
-
Increased secretion by lacrimal glands and salivary glands
-
Increased gut motility, bronchoconstriction of the lungs
-
Contraction of the detrusor muscle with the relaxation of urethral sphincters
-
Glycogen synthesis by the liver
-
Swelling of the clitoris and erection of the penis
-
Activation of the immune system
The parasympathetic nervous system does not appear to exert much control over vascular tone as the sympathetic nervous system does.[rx]
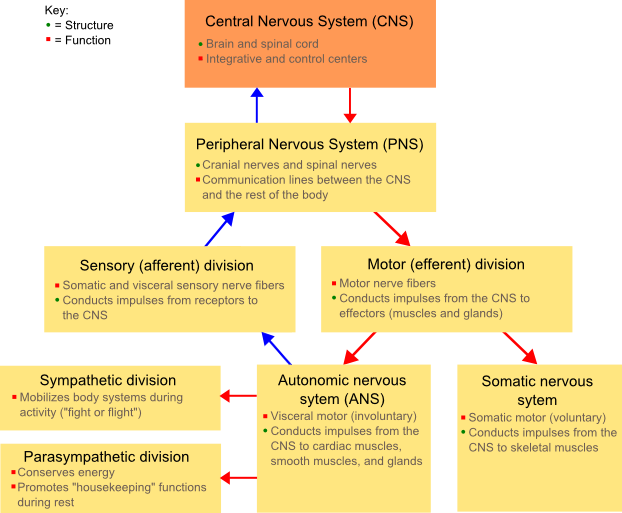
Comparing the Somatic and Autonomic Nervous Systems
The peripheral nervous system includes both a voluntary, somatic branch and an involuntary branch that regulates visceral functions.
Key Points
The somatic nervous system (SoNS) is the part of the peripheral nervous system associated with the voluntary control of body movements through the skeletal muscles and the mediation of involuntary reflex arcs.
The autonomic nervous system (ANS) is the part of the peripheral nervous system that controls visceral functions that occur below the level of consciousness.
The ANS can be subdivided into the parasympathetic nervous system (PSNS) and the sympathetic nervous system (SNS).
Key Terms
peripheral nervous system: Consists of the nerves and ganglia outside of the brain and spinal cord.
autonomic: Acting or occurring involuntarily, without conscious control.
somatic nervous system: The part of the peripheral nervous system that transmits signals from the central nervous system to skeletal muscles, and from receptors of external stimuli, thereby mediating sight, hearing, and touch.
EXAMPLES
Examples of body processes controlled by the ANS include heart rate, digestion, respiratory rate, salivation, perspiration, pupillary dilation, urination, and sexual arousal.
The peripheral nervous system (PNS) is divided into the somatic nervous system and the autonomic nervous system. The somatic nervous system (SoNS) is the part of the peripheral nervous system associated with the voluntary control of body movements via skeletal muscles.
The SoNS consists of efferent nerves responsible for stimulating muscle contraction, including all the non-sensory neurons connected with skeletal muscles and skin. The somatic nervous system controls all voluntary muscular systems within the body, and also mediates involuntary reflex arcs. The somatic nervous system consists of three parts:

The human nervous system: The major organs and nerves of the human nervous system.
- Spinal nerves are peripheral nerves that carry motor commands and sensory information into the spinal cord.
- Cranial nerves are the nerve fibers that carry information into and out of the brain stem. They include information related to smell, vision, eyes, eye muscles, the mouth, taste, ears, the neck, shoulders, and the tongue.
- Association nerves integrate sensory input and motor output; these nerves number in the thousands.
The autonomic nervous system (ANS) is the part of the peripheral nervous system that acts as a control system, functioning largely below the level of consciousness and controlling visceral functions. The ANS affects heart rate, digestion, respiratory rate, salivation, perspiration, pupillary dilation, micturition (urination), and sexual arousal.
Whereas most of its actions are involuntary, some, such as breathing, work in tandem with the conscious mind. The ANS is classically divided into two subsystems: the parasympathetic nervous system (PSNS) and the sympathetic nervous system (SNS).
The enteric nervous system is sometimes considered part of the autonomic nervous system and sometimes considered an independent system.
Divisions of the Autonomic Nervous System
The autonomic nervous system (ANS) contains two subdivisions: the parasympathetic (PSNS) and sympathetic (SNS) nervous systems.
Key Points
The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.
Sympathetic and parasympathetic divisions have complementary roles: the sympathetic division functions in actions requiring quick responses (fight or flight) and the parasympathetic division regulates actions that do not require rapid responsiveness (rest and digest).
The SNS and PSNS can be seen as constantly modulating vital functions, in a usually antagonistic fashion, to achieve homeostasis. This includes both cardiovascular and respiratory functions.
Key Terms
autonomic: Acting or occurring involuntarily, without conscious control.
fight or flight: This theory states that animals react to threats with a general discharge of the sympathetic nervous system, priming the animal for fighting or fleeing.
vasoconstriction: The constriction (narrowing) of a blood vessel.
EXAMPLES
Example functions of the SNS include diverting blood flow away from the gastrointestinal (GI) tract and increasing heart rate. Example functions of the PSNS include dilating the blood vessels that lead to the GI tract and stimulating salivary gland secretion.
The autonomic nervous system (ANS) is classically divided into two subsystems: the parasympathetic nervous system (PSNS) and sympathetic nervous system (SNS). The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.

The subdivisions of the autonomic nervous system: In the autonomic nervous system, preganglionic neurons connect the CNS to the ganglion.
Sympathetic and parasympathetic divisions typically function in opposition to each other. This opposition is often viewed as complementary in nature rather than antagonistic. For an analogy, one may think of the sympathetic division as the accelerator and the parasympathetic division as the brake.
The sympathetic division typically functions in actions requiring quick responses. The parasympathetic division functions with actions that do not require immediate reaction. Many think of sympathetic as fight or flight and parasympathetic as rest and digest or feed and breed.
However, many instances of sympathetic and parasympathetic activity cannot be ascribed to fight or rest situations. For example, standing up from a reclining or sitting position would entail an unsustainable drop in blood pressure if not for a compensatory increase in the arterial sympathetic tonus.
Another example is the constant, second-to-second modulation of heart rate by sympathetic and parasympathetic influences as a function of the respiratory cycles. More generally, these two systems should be seen as permanently modulating vital functions, in usually antagonistic fashion, to achieve homeostasis.
Some functions of the SNS include diverting blood flow away from the gastrointestinal (GI) tract and skin via vasoconstriction, enhancing blood flow to skeletal muscles and the lungs, dilating the bronchioles of the lung to allow for greater oxygen exchange, and increasing heart rate.
The PSNS typically functions in contrast to the SNS by dilating the blood vessels leading to the GI tract, causing constriction of the pupil and contraction of the ciliary muscle to the lens to enable closer vision, and stimulating salivary gland secretion, in keeping with the rest and digest functions.
Functional Organization of the Vegetative/Autonomic Nervous System
The vegetative or autonomic nervous system (from Greek: autos = self; nomos = law) uses both sensory and efferent neurons, which especially control the function of the internal organs.
The characteristic feature of the autonomic system is that its efferent nerves emerge as medullated fibers from the brain and spinal cord, are interrupted in their course by a synapse in a peripheral ganglion, and are then relayed for distribution as fine, non-medullated fibers. In this respect, they differ from the cerebrospinal efferent nerves, which pass without interruption to their terminations.
The autonomic nervous system allows the higher brain centers (the cerebral cortex and the limbic system) to subconsciously control organs of the autonomic nervous system. It controls functions such as sexual arousal, urination, digestion, and cardiorespiratory functions.
Autonomic nervous system divisions
The autonomic nervous system has 2 divisions based on anatomical, functional, and to a considerable extent, pharmacological grounds: the sympathetic and parasympathetic divisions. The 2 divisions have antagonistic effects on the internal organs they innervate.
Anatomically, the sympathetic nervous system has its motor cell stations in the lateral grey column of the thoracic and upper 2 lumbar segments of the spinal cord. The parasympathetic system is less neatly defined anatomically since it is divided into a cranial outflow, which passes along the cranial nerves 3, 7, 9, and 10, and a sacral outflow, with cell stations in the 2nd, 3rd, and sometimes 4th sacral segments of the cord.
Sensory neurons
The main input of the ANS particularly comes from autonomic sensory (viscerosensory) neurons, which are usually associated with interoceptors and act as sensory receptors in the blood vessels, the visceral organs, and the muscles. These neurons, which have the task to transduce information to the CNS, are usually located in the stomach and the lungs.
Unlike the signals that are triggered by a nice-smelling odor or a delicious-looking meal, the inner sensory signals are normally not experienced consciously, although the activation of the interoceptors can indeed advance into consciousness. Here, 2 typical examples would be the pain caused by damaged intestines or angina pectoris (chest pain) caused by inadequate perfusion of the myocardium.
Efferent neurons
On the other hand, efferent neurons forward the nerve impulses from the CNS to the target tissue (smooth muscle, heart muscle, or glands) and regulate visceral activities by an increase (excitation) or decrease (inhibiting).
Nerves of the sympathetic and parasympathetic nervous systems are responsible for these oppositional effects.
Sympathetic neurons accelerate the heartbeat, support the processes or effort of the body, and enable a ‘fight-or-flight’ reaction. This allows an improvement in performance and consequently, is stimulated in states of excitement, activity, and stress.
Parasympathetic neurons, in contrast, decelerate the heartbeat and induce a ‘rest-and-digest’ reaction. These neurons are responsible for relaxation, recreation, and inducing the regeneration of vital energy reserves.
Efferent responses are not controlled consciously, thus the activity of the ANS is unintentional. So-called ‘lie-detector tests’ are based on several autonomous reactions, since the pulse cannot be manipulated intentionally to half of the standard value. However, some people can alter their autonomic activities by applying adequate relaxing techniques.
Unlike the transmission of the impulse via the somatic motor neurons to the skeletal muscles, transmission to the visceral effectors involves 2 neurons.
Structure of the ANS/VNS
The 1st of the 2 motor neurons in every motoric signaling pathway is called a preganglionic neuron. Its soma is located in the brain or the spinal cord and its axon, on the other hand, leaves the CNS as a part of a cranial nerve or a spinal nerve.
Generally, the preganglionic neuron connects with an autonomic ganglion, where it forms a synapse with the second neuron of the signaling pathway, the postganglionic neuron. The soma and the dendrites of the postganglionic neurons are located in an autonomic ganglion, where they form synapses with 1 or more preganglionic neurons.
The ANS transduces nerve impulses from the preganglionic neurons to the autonomic neurons, where the signals are forwarded to the postganglionic neurons and then transmitted to the target tissue.
The following example deserves mention:
Spinal cord (CNS) → preganglionic neuron → autonomic ganglion → postganglionic neuron → heart (target tissue/effector)
Preganglionic neurons
Thoracolumbar part
The sympathetic part of the ANS is also called the thoracolumbar part since the somas of the preganglionic neurons are located in the lateral horn of the 12 thoracic segments, as well as the 1st 2 or 3 lumbar segments of the spinal cord.
Craniosacral part
On the other hand, the parasympathetic part of the ANS is also referred to as the craniosacral part because the somas of the parasympathetic, preganglionic neurons are located in the nuclei of 4 cranial nerves in the area of the brain stem, as well as in the lateral horns of the second to the fourth sacral segment of the spinal cord.
Autonomic ganglia
Autonomic ganglia are divided into 3 groups:
- Sympathetic chain ganglia
- Sympathetic prevertebral ganglia
- Parasympathetic ganglia
Sympathetic ganglia are located where the synapses between preganglionic and postganglionic sympathetic neurons interact.
Sympathetic chain ganglia
Ganglia of the sympathetic trunk (paravertebral ganglia) are arranged in a vertical column on each side of the spine and reach from the base of the skull down to the coccygeal bone. For the most part, organs above the diaphragm are innervated by the postganglionic axons of the ganglia of the sympathetic trunk.
Sympathetic prevertebral ganglia
Sympathetic prevertebral ganglia are located on the ventral side of the spine close to the large abdominal arteries. On the other hand, postganglionic axons of prevertebral ganglia innervate organs inferior to the diaphragm. The 3 largest prevertebral ganglia are:
- Coeliac ganglion (located right underneath the diaphragm)
- Superior mesenteric ganglion (located in the epigastric region)
- Inferior mesenteric ganglion (located in the umbilical region)
The branches of the sympathetic ganglionic chain have somatic and visceral distribution.
Somatic distribution
Each spinal nerve receives 1 or more grey rami from a sympathetic ganglion which distributes postganglionic non-medullated sympathetic fibers to the segmental skin area supplied by the spinal nerve. These fibers are vasoconstrictive to the skin arterioles, pseudo motor to sweat glands, and pilomotor to the cutaneous hairs.
Visceral distribution
Postganglionic fibers to the head and neck and to the thoracic viscera arise from the ganglion cells of the sympathetic chain. Those to the head ascend along the internal carotid and vertebral arteries, whereas those to the thoracic organs are distributed by the cardiac, pulmonary, and esophageal plexuses.
The abdominal and pelvic viscera are supplied by the postganglionic fibers which have their cell stations in more peripherally-placed prevertebral ganglia—the celiac, hypogastric, and pelvic plexuses—which receive their preganglionic fibers from the splanchnic nerves.
Parasympathetic Ganglia
Preganglionic axons of the parasympathetic nervous system form synapses with postganglionic neurons in terminal or intramural ganglia. For the most part, the ganglia are located near to or inside the wall of an organ.
Axons of preganglionic parasympathetic neurons are usually longer than most of the axons of preganglionic sympathetic neurons since they reach from the CNS all the way to an intramural ganglion of the innervated organ.
Afferent parasympathetic fibers
Visceral afferent fibers from the heart, lungs, and alimentary tract are conveyed in the vagus nerve. Sacral afferents are conveyed in the pelvic splanchnic nerves and are responsible for visceral pain experienced in the bladder, prostate, rectum, and uterus.
Although afferent fibers are conveyed in both sympathetic and parasympathetic nerves, they are completely independent of the autonomic system. They do not relay in the autonomic ganglia and have their cell stations, just like somatic sensory fibers, in the dorsal ganglia of the spinal and cranial nerves. They simply use the autonomic nerves as a convenient anatomical conveyor system from the periphery to the brain.
Postganglionic neurons
Axons of preganglionic sympathetic neurons can be connected to postganglionic neurons by the following 3 possibilities after they have headed to the ganglia of the sympathetic trunk:
- An axon can form a synapse with a postganglionic neuron directly in the first reached ganglion.
- An axon can ascend or descend to a higher or lower located ganglion before it is wired up with the postganglionic neuron, which runs vertically next to the sympathetic trunk.
- An axon can run through the sympathetic ganglion without forming a synapse and end in a prevertebral ganglion to be switched over to the postganglionic neuron.
A single preganglionic sympathetic fiber has many branches, which is the reason why it can be connected with more than 20 or more postganglionic neurons over synapses. The postganglionic axons typically end in different target tissues.
In these ganglia, presynaptic neurons only transmit to 4–5 postsynaptic neurons. They all individually provide a visceral target tissue and, as a consequence, this target tissue can be controlled separately by parasympathetic fibers.
Autonomic plexuses
Axons and sympathetic and parasympathetic neurons form networks that are called autonomic plexuses. They run along large arteries and can be found in the thorax, the abdomen, and the pelvis. The large cardiac plexus in the thorax is in charge of the innervation of the heart and the pulmonary plexus for the bronchial tree.
The largest autonomic plexus is the celiac (solar) plexus, which passes onto the liver, gallbladder, stomach, pancreas, spleen, kidneys, adrenal cortex, testicles, and the ovaries.
Neurotransmitter and Receptors of the ANS/VNS
Neurotransmitters are assigned to receptors – integral membrane proteins that are located in the plasma membrane of the postsynaptic neuron or a cell of the target tissue.
We differentiate between cholinergic and adrenergic neurons.
Cholinergic neurons and receptors
The ANS includes the following cholinergic neurons:
- All sympathetic and parasympathetic preganglionic neurons
- Sympathetic postganglionic neurons for most of the sweat glands
- All postganglionic parasympathetic neurons
Cholinergic neurons release the neurotransmitter acetylcholine (ACh) which is stored in synaptic vesicles and liberated by exocytosis. After that, it diffuses through the synaptic cleft and binds to specific cholinergic receptors.
Cholinergic receptors are further subdivided into the nicotinic and muscarinergic receptors that both bind to ACh.
Nicotinic receptors are embedded in the sympathetic and parasympathetic postganglionic neurons, as well as in the neuromuscular junction. They bear this term because nicotine simulates the action of ACh after binding to the receptors. In non-smokers, this substance is not traceable since nicotine is not a physiologically present substance in the human organism.
However, in the plasma membrane of all target tissues (the smooth muscle, myocardium, and the glands), the muscarinergic receptors are present, which are supplied by the parasympathetic postganglionic axons. An inhibition occurs in several receptors, whereas in others, an excitation occurs. Similarly, sweat glands have muscarinergic receptors which result in increased sweating.
ACh is quickly deactivated by the enzyme acetylcholine esterase and thus, the effects triggered by cholinergic neurons are short.
Adrenergic neurons and receptors
Noradrenaline (NA) is released in the ANS by adrenergic neurons. A great number of postganglionic sympathetic neurons are adrenergic. The NA is stored, just like ACh, in the synaptic vesicles, and released by exocytosis, which diffuses through the synaptic cleft and binds to specific adrenergic receptors of the postsynaptic membrane. The consequence is excitation or inhibition of the effector cell.
NA, as well as adrenaline, binds to the adrenergic receptors. The NA can be released as a neurotransmitter by sympathetic postganglionic neurons or as a hormone by the adrenal medulla, into the blood. Adrenaline is solely released as a hormone.
Also, the adrenergic receptors can again be subdivided into 2 subtypes which are innervated by most of the postganglionic sympathetic neurons. They are called alpha (α)-receptors and beta (β)-receptors, which are further subdivided according to their specific answers and the corresponding binding properties (α1, α2, β1, β2, etc.).
Broadly speaking, an activation of the α1- and β1-receptors induces an excitation, whereas α2- and β2-receptors yield an inhibition of the target tissue.
Autonomic reflexes
Answers that are triggered by the nerve impulses in an autonomic reflex arc are called autonomic reflexes. They play a key role in the following processes:
- Blood pressure (i.e. by adjusting the heart rate)
- Digestion (adjustment of motility and muscle tone in the GI tract)
- Defecation
- Urination (regulating the opening and closing of the sphincter)
The main control and integration center of the ANS is the hypothalamus, which receives sensory information about visceral functions (smell, taste, temperature etc.). Signals of the limbic system, which cohere with emotions, influence this process as well. The signals coming from the hypothalamus affect the autonomous centers in the brain stem, as well as in the spinal cord (medulla spinalis).
An autonomic reflex arc consists of the following components:
Receptor
- The distal end of a sensory neuron is the receptor of an autonomic reflex arc, which reacts to a stimulus and triggers a nerve impulse. Usually, autonomic sensory receptors are associated with interoceptors.
Sensory neurons
- The sensory neuron forwards nerve impulses to the CNS.
Integration center
- The main integration centers for the autonomic reflexes are located in the hypothalamus and the brain stem. Some autonomic reflexes are situated in the integration centers of the spinal cord, which are mostly responsible for urination and defecation.
- Connectivity: interneurons of the CNS forward signals from the sensory neurons to the motor neurons.
Motor neurons
- Signals triggered by the integration centers leave the CNS, via motor neurons, towards the target tissue. Two motor neurons connect the CNS in an autonomic reflex arc with the effector. The impulse is transduced by the preganglionic neuron to an autonomic ganglion from where it is forwarded through the postganglionic neuron to the target tissue.
Target tissue (effector)
- The effectors of the autonomic reflex are the smooth muscles, the heart muscle, or the glands.
Clinical Significance
Due to the extensive nature of the autonomic nervous system, it can be affected by a wide range of conditions. Some of these include[rx][rx][rx]
Inherited
-
Amyloidosis
-
Fabry disease
-
Hereditary sensory autonomic neuropathy
-
Porphyrias
Acquired
- Diabetes mellitus
- Uremic neuropathy/chronic liver diseases
- Vitamin B12 deficiency
- Toxin/drug-induced: alcohol, amiodarone, chemotherapy
- Infections: Botulism, Chagas disease, HIV, leprosy, Lyme disease, tetanus
- Autoimmune: Guillain-Barre, Lambert-Eaton myasthenic syndrome, rheumatoid arthritis, Sjogren, systemic lupus erythematosus
- Neurological: multiple system atrophy/Shy-Drager syndrome, Parkinson disease, Lewy body dementia/
Neoplasia: Brain tumors, paraneoplastic syndromes
Likewise, autonomic neuropathy can present in nearly any system. Orthostatic hypotension is the most common autonomic dysautonomia, but numerous other, less understood, findings may present[rx]
- Fixed heart rate
- Postural hypotension
- Resting tachycardia
- Dysphagia
- Gastroparesis; nausea, vomiting, abdominal fullness
- Constipation
- Bladder atony
- Absent/delayed light reflexes
- Decreased pupil size
- Erectile dysfunction
- Retrograde ejaculation
- Anhidrosis
- Gustatory sweating
- Cold extremities (due to loss of vasomotor responses)
- Edema (due to loss of vasomotor tone and increased vascular permeability)
The most prevalent symptoms of orthostatic hypotension are lightheadedness, tunnel vision, and discomfort in the head, neck, or chest. It may present concomitantly with supine hypertension due to increased peripheral resistance, which induces natriuresis, exacerbating orthostatic hypotension. There are numerous other, more benign stimuli that may either lower blood pressure (standing, food, Valsalva, dehydration, exercise, hyperventilation, etc.) or raise blood pressure (lying supine, water ingestion, coffee, head-down tilt, hypoventilation, etc.).[rx]
References