Anatomy of the Upper Limb /upper extremity or arm is a functional unit of the upper body. It consists of three sections, the upper arm, forearm, and hand. It extends from the shoulder joint to the fingers and contains 30 bones. It also consists of many nerves, blood vessels (arteries and veins), and muscles.
Surface Anatomy and Osteology: Phalanges
Any discussion of finger joints in human anatomy requires differentiation of:
- Metacarpophalangeal joints (MCP)
- Proximal interphalangeal joints (PIP)
- Distal interphalangeal joints (DIP)
Individual motor skills are attributed to the distinct mobility of the finger joints facilitated by the 3-movement axes.
Metacarpophalangeal articulations: The horizontal axis lies in the 3rd metacarpal and runs in a radial-ulnar direction to facilitate extension and flexion, although the degree of extension is not equal for all fingers. The sagittal axis lies in the middle of the 3rd metacarpal and runs in a dorsal-palmar direction, which enables abduction and adduction. The rotation occurs via a longitudinal axis, which is equal to the long axis of the 1st metacarpal. The average levels of active mobility are:
- 90–100° of flexion
- 0–40° of extension
- 20–30° of abduction
- 10–20° of adduction
Note: Axial rotation is only passive and is approx. 5° for both inner and outer rotation.
Proximal and distal interphalangeal articulations: The PIP and DIP joints merely move via the horizontal axis during flexion and extension. They lie in the convex head of the proximal phalanx of both the proximal and middle phalanges in a radial-ulnar direction. The average active degrees of mobility are:
| PIP | DIP |
|
|
Translational gaps can be triggered in the joints via mobilization impulse. However, these movements are of no major functional significance for active mobility during extension and flexion, and therefore, need not be tested during neutral-null method.
Metacarpophalangeal Articulations
Metacarpophalangeal articulations: Osseous structures and joint surfaces
The metacarpal head (caput metacarpal) articulates with the base of the proximal phalanx (basis phalanges proximal) via the metacarpophalangeal joints.
- Caput metacarpale – The caput metacarpale is convex. The joint surface is coated with cartilage on the dorsopalmar side and is larger than on the radioulnar side. The average thickness of the cartilage is about 0.8 mm and is especially distinct in the index and middle fingers.
- Basis phalanges proximal – The base of the proximal phalanx, contrary to the metacarpal head, is concave and is substantially smaller. The fibrous cartilage plate enlarges the joint surface in the distal area, which is fastened like a hinge at the palmar end and consists solely of fiber cartilage, as the name itself implies. Proximally, this turns into conjunctive tissue and is considered a type of glenoid ligament, but the nomenclature can be easily confused with the joint surface of the scapula to the humerus in the shoulder joint.
The contact surface of the cartilage plate where it rubs against the caput is the greatest in the neutral-null position. It is reduced under increased flexion because of its proximal translation. Ultimately, the cartilage plate provides insertion points for the deep metacarpal ligament, which joins the cartilage plate and the caput, as well as a few fibers of the interosseous muscles. The synovial tendon sheaths of the flexors are also attached via ring ligaments.
Metacarpal articulations: Joint capsule
The capsule surrounds the bone-cartilage threshold of the apex of the fiber cartilage plates. It completely envelops the joints and forms a dorsal and palmar recess. Additional smaller recesses are located in the radius and ulna. The joint capsule is reinforced by the palmar ligament (ligamentum palmare) at the basis of the phalanx and is dorsally infiltrated by several fibers of the dorsal aponeurosis.
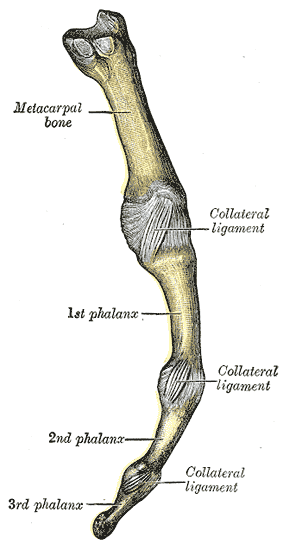
Metacarpal articulations: Ligaments
The metacarpophalangeal joints are connected with ligaments. Along with the radial and ulnar collateral ligaments, collateral accessory ligament and the phalangeoglenoidal ligaments ensure sufficient protection of the osseous structures. They neutralize palmar pulling forces during flexion, which primarily target the ligament bands.
Ligamentum collaterale radiale et ulnare
Both the radial and ulnar lateral ligaments are oriented in the same direction and display a similar force of movement. They both emerge dorsally from the flexion and extension axis along with the metacarpal head and insert into the lateral base of the proximal phalanx. The radial lateral ligament has a more slanted course than the ulnar ligament, due to the asymmetric joint surfaces. During flexion, the ligaments are strained, to prevent passive gapping and active abduction and adduction in the metacarpophalangeal joints during this movement. These movements are facilitated by extension as the lateral ligaments are not under strain.
Ligamentum collateral accessories
This ligament inserts into the metacarpal head proximal to the lateral ligament and connects with the radial and ulnar edge of the palmar cartilage plate. Consequently, this ligament connects with the respective lateral ligament and supports tension during flexion. However, contrary to the ligamentum collaterale radiale et ulnare, the ligamentum accessorium is also strained in extension, although it does not prevent lateral movements of the finger, showing that these do not exhibit similar pulling force as the lateral ligaments.
Ligamentum phalangoglenoidale
This ligament is not generally observed, although it facilitates lateral reinforcement of the joint capsule, and thus the joint itself, similar to lateral ligaments. It stems from the base of the proximal phalanx, runs in a proximal-palmar direction over the lateral ligament and inserts into the cartilage plate and into ring ligament A1 with its distal fibers.
Proximal and distal interphalangeal hand articulations
Both the PIP and DIP joints are hinge joints.
Articulations interphalangeal manus proximal et distances: Osseous structures and joint surfaces
In the PIP and DIP joints, the caput phalangis articulates with the basis phalangis.
Caput phalanges – The caput phalanges of the proximal and middle phalanx is made up of the proximal convex joint surfaces of the PIP and DIP joints. It is coated with a layer of cartilage with an average thickness of 0.5–1 mm.
Basis phalanges – The basis phalanges is the concave distal joint partner of the PIP and DIP joints. The layer of cartilage is much thinner compared with the caput, at 0.2–0.5 mm. A fiber cartilage plate is located at the palmar corner of the base of the middle phalanx and is thicker in the PIP than in the DIP joint.
Proximal and distal interphalangeal hand articulations: Joint capsule
The joint capsule is inserted both into the bone-cartilage threshold and the tip of the fiber cartilage plate of the PIP and DIP joints. From the palm, the fiber cartilage plate is entirely inserted into the capsule. From the dorsal and palmar sides, it forms recesses in the proximal interphalangeal joints, whereby the recess in the dorsal DIP joint region is more distinct than in the palmar DIP region.
Proximal and distal interphalangeal hand articulations: Ligaments
The names of the ligament structures in the PIP and DIP joints are the same as those of the metacarpophalangeal joints. Nevertheless, they have different origins and beginnings, the respective localization of which must be remembered.
Ligamentum collaterale ulnare et radiale
The ulnar and radial lateral ligaments emerge dorsally and proximally from the caput phalanges and insert into the tuberculum laterale of the palmar basis of the middle and distal phalanx. They are taut during flexion and relaxed during extension.
Ligamentum collaterale accessorium – Both radius and ulna carry this ligament carries its origin in the caput of the proximal and middle phalanges. It inserts into the edge of the fiber cartilage plate, and along with specific fibers enters the ring ligament A3 (PIP) and ring ligament A5 (DIP). It is taut during flexion, while extension has no direct effect.
Ligamentum phalangoglenoidale – This ligament emerges in the radial and ulnar direction from the base of the middle phalanx and its roots are in the palmar cartilage plate. It is more common in the PIP joint than in the DIP joint. In some individuals, it is even missing entirely from the DIP joint.
The Thumb Joints: General Information
The thumb (pollex) is a functional peculiarity among the fingers. Its segments include:
- Carpometacarpalis pollicis
- Carpometaphalangealis pollicis
- Interphalangealis pollicis
Articulatio carpometacarpalis pollicis
The horizontal axis runs through the distal portion of the os trapezium. Flexion and extension are facilitated by this axis. Abduction and adduction are enabled via sagittal axis, which runs through the os metacarpale I. No rotation occurs in the articulatio carpometacarpalis pollicis. Instead, opposition and reduction are possible, with no actual axis described for these biomechanical movements. The opposition is a combination of flexion, adduction and axial rotation. Reduction merely describes the return of the thumb from opposition to a neutral-null position. The average degrees of active movement are:
- 20° of flexion
- 45° of extension
- 45° of abduction
- 0° adduction
- 20–30° of opposition
- The reduction is not numbered in the study cited.
Articulatio caropmetaphalengealis pollicis
Flexion and extension run through the horizontal axis located in the caput metacarpale. The sagittal axis for abduction and adduction is also localized in the metacarpal head, facilitating only passive movements. The rotation occurs in the longitudinal axis, which is equal to the beam axis of the proximal phalanx. The average degrees of active movement are:
- 50° of flexion
- 5° of extension
- Rotation is not numbered in the literature used.
Articulatio interphalangealis pollicis
This joint is located at the caput phalangis of the proximal phalanx, and only allows flexion and extension in the horizontal axis. The average degrees of active movement are:
- 80° of flexion
- 5–10° of extension
Articulatio carpometacarpal pollicis
The carpometacarpal joint I is defined as a saddle joint.
Articulatio carpometacarpal pollicis: Osseous structures and joint surfaces
In the carpometacarpal joint I, the basis metacarpals I articulate with the os trapezium of the distal carpal series.
Basis metacarpals I – The basis of metacarpals I is radially convex and dorsally concave and is important for oppositional motion via a combination of flexion, adduction, and axial rotation.
Os trapezium – The joint surface of the os trapezium is curved opposite to that of the basis metacarpal I. It is radially concave and dorsally convex. The metacarpal joint is thus a congruent joint.
Articulatio carpometacarpal pollicis: Joint capsule
The joint capsule of the carpometacarpal joint I is wide and loose, which allows for large degrees of motion. The insertion points are located in the respective bone-cartilage thresholds of the aforementioned osseous structures. The capsule forms both dorsal and palmar recesses.
Articulatio carpometacarpal pollicis: Ligaments
The ligament structures of this joint lie directly atop the joint capsule and thus facilitate optimal stabilization in every position of the thumb.
- Ligamentum carpometacarpal palmaria – These are very thin ligaments originating in the os trapezium and the ligamentum carpi transversum, with their roots in the basis metacarpals I. They are taut during extension and abduction.
- Ligamentum carpometacarpal dorsale – This ligament links the os trapezium with the basis metacarpalis I and is a component of the joint capsule. It is taut during flexion and opposition.
- Ligamentum carpometacarpal obliquum anterius – Extending outward from the tuberculum ossis trapezii, the ligament runs radially along with the basis metacarpalis I. Similar to the ligamentum carpometacarpalia palmaria, it is taut during extension and abduction.
- Ligamentum carpometacarpale obliquum posterius – The posterior counterpart originates dorsally from the os trapezium, with its roots located on the palmar surface of the basis metacarpalis I. It is taut during flexion and abduction.
Articulatio metacarpophalangealis pollicis
The basal joint of the thumb is an ellipsoidal joint.
Articulatio metacarpophalangeal pollicis: Osseous structures and joint surfaces
The basal joint of the thumb is formed by the caput metacarpal I and basis phalanges.
- Caput metacarpal I – The caput metacarpal I form the proximal convex joint partner at the basal joint of the thumb. The cartilage layer is about 1 mm thick at the location of both radial and ulnar sesamoid bones on the palmar side. It serves as an origin for, among others, the ligamentum collaterale accessorial and the second fiber segment of the ligament collaterale radiale et ulnare pollicis.
- Basis phalanges – The base of the proximal phalanx is the distal concave joint partner located in the basal joint of the thumb. Measuring approx. 0.5 mm, the cartilage layer is much thinner than the caput metacarpals I and carries a proximal fiber cartilage plate in its palmar corner.
Articulatio metacarpophalangealis pollicis: Joint capsule
The joint capsule of the basal joint of the thumb inserts into the caput metacarpals I along with the bone-cartilage threshold via both membranes. It forms small dorsal and palmar recesses and is laterally braced by the collateral ligaments. In addition, the musculus extensor pollicis brevis is joined with the dorsal capsule. The membrane fibrosis carries a palmar connection with the ring ligaments that fasten the musculus flexor pollicis longus to the cartilage plate.
Articulatio carpometacarpal pollicis: Ligaments
Again, the ligament structures bear the same names as those of the articulatio interphalangeal manus proximates et distal and articulatio metacarpophalangeal. They merely carry an additional ‘pollicis’ for the lateral ligaments, and the ligament collaterale accessorium is its fiber segment in the thumb.
Ligamentum collaterale radiale et ulnare pollicis – The lateral ligaments of the thumb are divided into 2 fiber segments. The 1st fiber segment is known as the ligamentum collaterale proprium. It originates in the caput metacarpal I and inserts into the base of the proximal phalanx. The 2nd fiber segment is known as the b > lig. collaterale accessorium and originates next to the 1st fiber segment but inserts into the radial and ulnar sesamoid bone.
Lig. phalangoglenoidale – This ligament is localized on the surface, originates in the radial and ulnar sides of the basis phalangis, with roots in the respective sesamoid bone.
Articulatio interphalangeal pollicis
The interphalangeal joint of the thumb is a hinge joint.
Articulatio interphalangeal pollicis: Osseous structures and joint surfaces
The interphalangeal joint of the thumb consists of the caput phalangis proximalis and the basis phalangis distalis.
- Caput phalangis proximalis – The caput phalangis proximalis is the proximal convex joint partner of the articulatio interphalangealis pollicis.
- Basis phalangis distalis – The basis phalangis distalis is the distal concave joint partner of the interphalangeal joint of the thumb. A fiber cartilage plate is located in the palmar corner of the basis of the middle phalanx.
Articulatio interphalangealis pollicis: Joint capsule
Both membranes insert into the bone-cartilage threshold of the fiber cartilage plate of the basis phalangis distalis. The joint capsule forms small dorsal and palmar recesses and largely consists of fatty and synovial tissue.
Articulatio interphalangealis pollicis: Ligaments
This continues into the interphalangeal joint of the thumb. However, there is no ligamentum phalangoglenoidale here.
Ligamentum collaterale ulnare et radiale – The lateral ligaments arise both ulnar and radial to the dorsal side of the caput phalangis proximalis and insert into the palmar base of the end phalanx. They are taut during flexion and loose during extension.
Ligamentum collaterale accessorium – This ligament stems from both the radial and ulnar sides of the caput phalangis, proximal-palmar to the lateral ligaments. Its roots are located in both the radial and ulnar edges of the fiber cartilage plate in the basis phalangis distalis. They are taut during flexion, while their tension in extension is not further discussed in the current literature.
Examples of Diseases of the Finger and Thumb Joints
Due to the wide variety of pathologies associated with the structures discussed above, we will focus on the most important diseases with a high incidence rate.
Rheumatoid arthritis
As described above, a majority of rheumatoid diseases affect the hand and finger joints. Synovial proliferation results in skeletal erosion, destruction of the capsular and ligamentous structures, and lesions in the tendon tissue, which results in malpositions of the hand and fingers. In the metacarpophalangeal joints, it is known as ulnar deviation; in the thumb, it is referred to as buttonhole deformity (90–90 deformity, Z-deformity) or swan-neck deformity (M-deformity).
Subluxation of the basal joints

Image: Joint dislocation of interphalangeal joint of the thumb. By Hellerhoff, License: CC BY-SA 3.0
The progressive inflammation involving the joints and the resulting destruction of bone and cartilage tissue result in malposition of the ulnar hand joint toward the palm. The radial extensors pull the hand in a radial abduction via supination.
The finger position in ulnar deviation may lead to subluxation or complete dislocation of osseous structures. Normal finger movements are no longer possible in this state, and patients report incredible pain.
Heberden’s mode
Heberden’s node often forms in the distal finger joints as a result of arthritic incidents, with women more commonly affected than men. These are known as mucoid cysts that form along the edge of the extensor tendons. They are filled with synovial fluid and emerge from the capsule of the DIP joint like a hernia.
If the node is not treated effectively, it results in compensatory malflexion with subsequent contractures that are very painful for the patient. Conservative treatment with inflammation-inhibiting medication and radiation, as well as physical therapy and ergotherapy, is recommended.
Rhizarthritis
The arthritic changes involving the carpometacarpal joint of the thumb are referred to as rhizarthritis. Progressive instability of the joint results in both dorsal and radial subluxation of the thumb, which advances into pain and cartilage decay. The restricted movement due to pain results in pollex adductus, malposition of the basal joint of the thumb in flexion and adduction combined with a palm position.
All encumbering movements, especially the opposition, are described as very painful by those affected. Patients also complain of increasing loss of strength, which impairs the performance of ADLs. Rhizarthritis is usually treated conservatively with medication, physical therapy, and ergotherapy. Advanced cases of arthritis are treated via surgical implantation of a replacement prosthetic with arthrodesis in a flexion position.
Skier’s thumb
A fall with reflexive, abrupt leaning on the ski pole, may result in the so-called skier’s thumb syndrome. The ulnar lateral ligament is overextended or (partially) ruptured due to the traumatic abduction and extension of the metacarpophalangeal joint. Severe cases may involve osseous avulsion with luxation of the basal joint of the thumb.
Stener lesion results when the end of the tendon of the musculus adductor pollicis strikes against the joint. Overextensions and partial ruptures are usually treated conservatively, while total ruptures with skeletal involvement and the Stener lesion are indications for surgical intervention.