Hypocalcemia, Hypoglycemia, Malignancies, Diabetic Ketoacidosis, Lactic Acidosis is low calcium levels in the blood serum. Mildly low levels that develop slowly often have no symptoms. Otherwise symptoms may include numbness, muscle spasms, seizures, confusion, or cardiac arrest.
Hypocalcemia also spelled hypocalcemia, is low calcium levels in the blood serum. The normal range is 2.1–2.6 mmol/l(8.8–10.7 mg/dl, 4.3–5.2 mEq/l) with levels less than 2.1 mmol/l defined as hypocalcemia.Mildly low levels that develop slowly often have no symptoms.Otherwise symptoms may include numbness, muscle spasms, seizures, confusion, or cardiac arrest
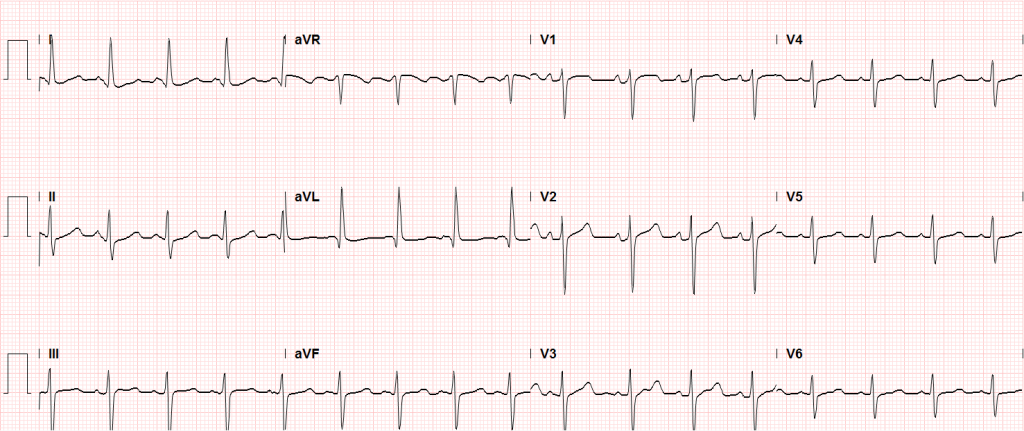
34M with a history of HTN, polysubstance abuse, presenting with muscle cramps. He reported onset of diffuse muscle cramping 1-hour prior to presentation while showering. Symptoms involved bilateral upper and lower extremities and resolved spontaneously.
On initial evaluation, the patient was tachycardic and hypertensive. Examination was notable for tremors in bilateral upper extremities with outstretched hands, as well as of extended tongue. Other notable findings included spasm of the upper extremity during blood pressure measurement, hyperreflexia and clonus.
Laboratory evaluation was notable for normal total calcium level, low ionized calcium level, primary respiratory alkalosis, and elevated anion gap metabolic acidosis.
The patient was treated with intravenous fluids, benzodiazepines for alcohol withdrawal, and calcium gluconate 4g IV and was admitted.
Calcium Homeostasis
Fraction
- 15% bound to anions (phosphate, lactate, citrate)
- 40% bound to albumin
- 45% free (regulated by PTH, Vit-D)
Conditions causing changes in total calcium (without affecting ionized calcium)
- Low albumin causes hypocalcemia. Corrected = measured + [0.8 x (4-albumin)]
- Elevated albumin causes hypercalcemia
- Multiple myeloma causes hypercalcemia
Conditions causing changes in ionized calcium (without affecting total calcium)
- Alkalemia causes increased ionized calcium binding to albumin and decreases ionized calcium levels
- Hyperphosphatemia causes increased ionized calcium binding to phosphate and decreases ionized calcium levels
- Hyperparathyroidism causes decreased ionized calcium binding to albumin and increases ionized calcium levels
Causes of Hypocalcemia
Symptoms
| ACUTE | CHRONIC |
|---|---|
Neuromuscular
Cardiac
|
CNS
Ophthalmologic
|
Treatment
Severe (symptomatic, QT prolongation)
- Calcium gluconate 1-2g IV in 50mL of D5W over 10-20min followed by slow infusion of additional 2g over 2 hours.
Asymptomatic
- Calcium gluconate 1g PO q6h
- Calcitriol 0.2mcg PO BID
Oncologic Emergencies
Complications
- Airway obstruction
- PNA
- Pleural effusion
- Pericardial effusion
- VTE
SVC syndrome
- Symptoms: dyspnea (airway edema), chest fullness, blurred vision, headache (increased ICP)
Massive hemoptysis
- Management: ETT (large-bore for bronschoscopy), affected side down
Brain Metastases
- Cancers: melanoma, lung, breast, colorectal
- Management: dexamethasone 10mg IV load, elevated HOB, hypertonic saline or mannitol, prophylactic anti-eplipetics
Meningitis
- Pathogens: Listeria (ampicillin), Cryptococcus (amphotericin)
- Evaluation: CSF sampling with cytology (diagnose leptomeningeal metastases)
Metabolic Disturbances
Hypercalcemia
- Cancers: MM, RCC, lymphoma, bone metastases (breast, lung, prostate)
- Mechanism: metastatic destruction, PTH-RP, tumor calcitriol
- Prognosis: 50% 30-day mortality
Symptoms
- Chronic: anorexia, nausea/vomiting, constipation, fatigue, memory loss
- Acute: CNS (lethargy, somnolence)
Findings
- Calcium: >13.0mg/dL
- ECG: QT shortening
Treatment
- Mild: IVF
- Severe: IVF, loop diuretics, bisophosphanate (pamidronate 90mg IV infused over 4 hours), consider calcitriol, consider hemodialysis if cannot tolerate fluids or unlikely to respond to diuretics
Hyponatremia
- Cancers: lung (small-cell), pancreatic, ovarian, lymphoma, thymoma, CNS
- Mechanism: SIADH
- Symptoms: muscle twitching, seizure, coma
- Management: fluid restriction, if seizing administer 3% hypertonic saline at 100cc/hr until resolution
Hypernatremia
- Mechanism: decreased intake, increased GI losses from chemotherapy
- Management: cautious fluid resuscitation
Tumor Lysis Syndrome (TLS)
- Cancers: hematologic, rapid-growth solid tumors
- Mechanism: release of intracellular contents (uric acid, K, PO4, Ca)
- Timing: 1-4 days after therapy (chemo, radiation)
Diagnosis
- Uric acid >8mg/dL
- Potassium >6mEq/L
- Calcium <7mg/dL
- PO4 >4.5mg/dL
- Acute kidney injury
Management
- IVF, allopurinol, rasburicase, urinary alkalinization
- Consider hemodialysis if volume overloaded
Localized Complications
Musculoskeletal Complications > Spinal cord compression
- Cancers: prostate, breast, lung, RCC, non-Hodgkin lymphoma, MM (5-10% of all cancer patients)
- Sites: thoracic (60%), lumbosacral (30%), cervical (10%)
- Symptoms: pain (worse lying flat, cough/sneeze, heavy lifting)
- Evaluation: MRI (se 93%, sp 97%)
- Management: dexamethasone 10mg IV load, 4mg q6h, neurosurgical consultation, radiation oncology consultation
Pathologic fracture
- Features: sudden onset, low-force mechanism
Therapy Complications
Neutropenic fever
- Definition: ANC <500 or ANC <1000 with expected nadir <500 (nadir typically occurs 5-10d after chemotherapy) with Tmax >38.3°C or >38.0°C for >1h
- Examination: subtle signs of infection, thorough examination is critical (skin, catheter, perineum)
- Treatment: carbapenem monotherapy, vancomycin if indwelling catheter, oncology consultation for colony stimulating factors
Chemotherapy-induced vomiting
- Management: ondansetron with dexamethasone, consider NK-1 antagonist (aprepitant)
Hematologic Malignancies
- Acute leukemia
- Signs/Symptoms: leukopenia (infection), anemia (weakness/fatigue), thrombocytopenia (bleeding)
- Diagnosis: >5% blasts
- Thrombocytopenia
- Management
- No bleeding, goal >10,000
- Fever, coagulopathy, hyperleukoctosis, goal >20,000
- One unit of platelets increases count by 5,000
- Management
- Hyperleukocytosis
- Definition: WBC > 50-100k
- Complications: microvascular congestion (pulmonary, cerebral, coronary)
- Symptoms
- CNS: confusion, somnolence, coma
- Pulmonary: dyspnea, respiratory alkalosis
- Management: cytoreduction (induction chemotherapy, increased risk TLS)
- Hyperviscosity
- Cancer: macroglobulinemia, MM
- Symptoms: epistaxis, purpura, GIB, neuro deficits
- Diagnosis: serum viscosity > 1.4-1.8
- Management: emergent plasmapheresis
- Polycythemia
- Diagnosis: Hb >17
- Differential: dehydration, hypoxia, smoking, altitude
- Symptoms: HA, vertigo, angina, claudication, pruritus (after showering)
- Complications: thrombosis (stroke), bleeding
- Management: emergent phlebotomy (500cc if otherwise healthy)
- Thrombocytosis
- Diagnosis: platelet >1,000,000
- Symptoms: vasomotor (HA, lightheadedness, syncope, chest pain, paresthesias)
- Management: low-dose aspirin
Acid-Base Disturbances
Method
- Primary disturbance (acidemia/alkalemia)
- Primary process (metabolic/respiratory)
- Presence of mixed disorder
- Increase PCO2 of 10, increases HCO3 by 1 (acute) or 3 (chronic)
- Decreased PCO2 of 10, decreases HCO3 by 2 (acute) or 5 (chronic)
- Increase HCO3 of 1, increases PCO2 by 0.7
- Decreased HCO3, add 15, result should equal PCO2 and number after decimal of pH
- Anion gap
Causes
Anion Gap
- Methanol
- Uremia
- DKA/AKA
- Paraldehyde, propylene glycol
- INH
- Lactate
- Ethylene glycol
- Salicylate
Non-Anion Gap
- Fistulae
- Ureteral fistulae
- Saline
- Diarrhea
- Carbonic anhydrase inhibitors
- Spironolactone
- RTA
Metabolic Alkalosis
- Vomiting
- Volume depletion
- Diuretics
- Steroids
Respiratory Acidosis
- CNS lesion
- Myopathies
- Chest wall abnormalities
- Obstructive lung disease
Respiratory Alkalosis
- Anxiety
- Fever
- Hyperthyroidism
- Hypoxia
- Sympathomimetic
Hypoglycemia
Case 1
In the medical intensive care unit, a patient who had sustained a cardiac arrest with return of spontaneous circulation but no recovery of neurological function develops septic shock complicated by end-stage renal disease, shock liver, and now refractory hypoglycemia.
Case 2
An approximately 60 year-old male with diabetes is brought in by ambulance after family called 911 for unresponsiveness. His initial glucose was 35mg/dL, his home medications are unknown.
Symptoms
- Autonomic: tremor, palpitations, anxiety, diaphoresis
- Neuroglycopenic: cognitive impairment, psychomotor, seizure, coma
Diagnosis
- Serum glucose <60mg/dL
- Generally symptomatic at <55mg/dL though threshold is variable depending on chronicity
Whipple Triad:
- Symptoms suggestive of hypoglycemia
- Low glucose
- Resolution of symptoms after administration of glucose
Differential Diagnosis of Hypoglycemia
Common Anti-hyperglycemic Drugs and Pharmacology
| DRUG | PHARMACOLOGY | ||
|---|---|---|---|
| ONSET | PEAK | DURATION | |
Rapid-acting insulin
|
15-30min | 1-2h | 3-5h |
Short-acting insulin
|
30-60min | 2-4h | 6-10h |
Intermediate-acting insulin
|
1-3h | 4-12h | 18-24h |
Long-acting insulin
|
2-4h | None | 24h |
Sulfonylurea
|
– | 2-6h | 12-24h |
Evaluation of Hypoglycemia
Patients with known diabetes who are not systemically ill and can identify a clear precipitant, no extensive workup is required. In severely ill patients, consider:
- BMP
- LFT
- EtOH
- Infectious workup: CXR, UA, urine and blood cultures
- ECG, troponin
- Other studies: insulin, C-peptide, pro-insulin, glucagon, growth hormone, cortisol, B-OH, insulin antibodies
Management and Monitoring
Disposition
Admission or observation for oral anti-hyperglycemic agent or intermediate- to long-acting insulin. Consider discharge after 4h uneventful observation if:
- Hypoglycemia fully and rapidly reversed without continuous infusion of dextrose
- Tolerated a full meal in ED
- Clear and innocuous cause identified with recurrence unlikely
- Adequate patient understanding, home support/monitoring, and ability to detect/prevent recurrence with close primary care follow-up
Diabetic Ketoacidosis
Algorithm for the Management of Diabetic Ketoacidosis
Altered Mental Status
Components of Consciousness
Causes of Altered Mental Status
History
- Rate of onset
- Abrupt: CNS
- Gradual: Systemic
Physical Examination
Vital Signs
- Blood Pressure: low (shock), high (SAH, stroke, ICP)
- Heart Rate: low (medication overdose, conduction block), high (hypovolemia, infection, anemia, thyrotoxicosis, drug/toxin)
- Temperature: low/high (infection, drug/toxin, environmental)
- Respiratory Rate: low/high (CNS, drug/toxin, metabolic derangement)
Eyes
- Unilateral dilation: CNS/structural cause
- Papilledema: ICP
- EOM: cranial nerve dysfunction
- Oculocephalic: brainstem function
Head: trauma
- Mucous membranes: hydration, laceration
- Neck: meningeal irritation
- Pulmonary: respiratory effort
- CV: murmur, arrhythmia, CO
- Abdomen: pulsatile mass, sequelae of liver failure
- Skin: rash, needle tracks
Labs
- Glucose
- ECG: arrhythmia, ischemia, electrolyte abnormalities
- BMP: electrolytes, renal failure, anion gap
- ABG: hypoxemia, hypercarbia
- Urinalysis: infection, SG
- Utox
- CBC: leukocytosis, leukopenia, severe anemia, thrombocytopenia
- Ammonia: hepatic encephalopathy
- TFT: thyrotoxicosis, myxedema coma
- CSF: meningitis, encephalitis
Imaging
- CT head: Non-contrast sufficient to identify ICH. Use contrast if mass/infection suspected
- CTA head/neck: If aneurysm, AVM, venous sinus thrombosis or vertebrobasilar insufficiency suspected
- CXR: PNA
Lactic Acidosis
HPI:
59F with a reported history of congestive heart failure, presenting with intermittent chest discomfort for three days.
She characterized this discomfort as “heartburn”, describing a mid-epigastric burning sensation radiating up her neck, not associated with exertion, lasting 1-2 hours and resolving with antacids. The patient has poor exercise tolerance at baseline and for the past several years has been able to ambulate only short distances around her home, and states that these symptoms have been worsening in the past week. She denies chest pain on exertion, orthopnea or paroxysmal nocturnal dyspnea. She states that she was diagnosed with congestive heart failure five years ago, but was never prescribed medications.
On further questioning, the patient reports several weeks of mouth and lip pain which has limited oral intake, though no dysphagia to solids or liquids. She otherwise denies fevers/chills, abdominal pain, nausea/vomiting, cough, changes in urinary or bowel habits.
In the emergency department, the patient was noted to have an elevated serum troponin, though ECG showed no changes of acute ischemia/infarction.
PMH:
- Congestive heart failure
PSH:
- None
FH:
- Mother with diabetes
- Father with MI at age 65
SHx:
- 4-5 drinks of alcohol/day
- No tobacco or drug use
Meds:
- None
Allergies:
NKDA
Physical Exam:
| VS: | T | 37.4 | HR | 106 | RR | 18 | BP | 145/82 | O2 | 100% RA |
| Gen: | Morbidly obese female, lying in bed, in no acute respiratory distress, speaking in complete sentences. | |||||||||
| HEENT: | Dry, cracked lips, slightly erythematous, otherwise moist mucous membranes, poor dentition. Mild scleral icterus. No cervical lymphadenopathy. | |||||||||
| CV: | Rapid rate, regular rhythm, normal S1/S2, II/VI systolic ejection murmur at LUSB, no radiation appreciated. No jugular venous distension. | |||||||||
| Lungs: | Clear to auscultation in posterior lung fields bilaterally, no crackles appreciated. | |||||||||
| Chest: | Well-circumscribed erythematous patch in folds beneath left breast, no underlying fluctuance, no significant tenderness to palpation. On contralateral breast, some hyperpigmentation but no erythema. | |||||||||
| Abdomen: | Obese, non-tender, non-distended. Patch of erythema below pannus, mildly tender to palpation. | |||||||||
| Ext: | Bilateral lower extremities with marked edema and overlying scaly plaques, some slightly ulcerated weeping serous fluid. Peripheral pulses are difficult to palpate, capillary refill difficult to assess. | |||||||||
Labs/Studies:
- CBC: 11.1/11.1/34.5/212 (MCV 114.2)
- BMP: 140/4.5/97/20/10/1.14/64
- Anion Gap: 23
- LFT: AST: 73, ALT: 26, AP: 300, TB: 4.6, DB: 2.1, Alb: 3.0, INR 1.3
- BNP: 158
- Troponin: 1.284
Imaging:
CT Pulmonary Angiography:
No evidence of central pulmonary embolism, thoracic aortic dissection, or thoracic aortic aneurysm. Evaluation of the peripheral vessels is limited due to motion artifact. No focal consolidation or pneumothorax.
CT Abdomen/Pelvis non-contrast:
No evidence of intra-abdominal abscess or definite source of infection. Marked hepatic steatosis.
CT Lower Extremity non-contrast:
Diffuse circumferential subcutaneous edema involving both lower extremities from the level of the mid thighs distally through the feet. There are bilateral subcutaneous calcifications which are likely venous calcifications in the setting of chronic venous stasis disease. There is some overlying skin thickening.
TTE:
There is moderate concentric left ventricular hypertrophy with hyperdynamic LV wall motion. The Ejection Fraction estimate is >70%. Grade I/IV (mild) LV diastolic dysfunction. No hemodynamically significant valve abnormalities.
US Abdomen:
Hepatomegaly, echogenic liver suggesting fatty infiltration. Moderately blunted hepatic vein waveforms suggesting decreased hepatic parenchymal compliance.
Assessment/Plan:
The patient was admitted to the cardiology service for management of NSTEMI and evaluation of undiagnosed CHF. She was started on a heparin continuous infusion. In addition, a CT pulmonary angiogram was obtained to evaluate for pulmonary embolism as an explanation of her progressive dyspnea on exertion. No PE, consolidation or effusion was identified.
Despite the patient’s reported history of congestive heart failure, there was no evidence that her symptoms were a result of an acute exacerbation with only a mildly elevated BNP but no jugular venous distension or evidence of pulmonary edema. The patient’s significant lower extremity edema was more suggestive of chronic venous stasis.
One notable laboratory abnormality that was explored was her elevated anion gap metabolic acidosis. Studies submitted included serum lactate, salicylates, osmolarity, CK, and urinalysis for ketonuria. This evaluation was notable for an elevated serum lactate of 13.2mmol/L and an arterial blood gas that showed adequate respiratory compensation (and no A-a gradient). Given the patient’s modest leukocytosis (with neutrophil predominance), and tachycardia, the concern for sepsis was increased though the source remained unclear. Prominent possibilities included a skin and soft-tissue infection vs. less likely intra-abdominal source though the patient’s physical examination was not suggestive of a process that would produce such a substantial lactic acidosis. Blood cultures were drawn and the patient was started on empiric antibiotics for the suspected sources. In addition, the patient was cautiously volume resuscitated given her reported history of CHF while pending a transthoracic echocardiogram to evaluate cardiac function. Additional imaging including CT abdomen/pelvis and lower extremities was obtained (though without contrast due to the patient’s recent exposure), and no obvious source was identified.
Over the next two days, the patient’s serum lactate downtrended to normal range, as did the serum troponin. A transthoracic echocardiogram showed an LVEF >70% with mild concentric hypertrophy and diastolic dysfunction. Blood and urine cultures were without growth.
Additional issues managed during the hospitalization included elevated serum transaminases (AST > ALT), conjugated hyperbilirubinemia and evidence of decreased hepatic synthetic function with hypoalbuminemia and elevated INR. Given the patient’s history of EtOH use, as well as other corroborating findings including macrocytic anemia, hypomagnesemia, folate and B12 deficiency, this was attributed to alcoholic hepatitis(discriminant function <32). Infectious hepatitis serologies were negative. The patient was started on nutritional supplements. Finally, the patient persistently complained of lip and oral mucosal pain. Examination was without discrete lesions but some mucosal redness was identified. Despite poor dentition, there was no evidence of abscess and HSV/HIV testing was negative. This was thought to be stomatitis caused by her identified nutritional deficiencies.
Differential Diagnosis of Elevated Serum Lactate
Algorithm for Evaluation of Acidemia
Algorithm for Evaluation of Alkalemia
References