Post Surgical Back Pain /Failed back surgery syndrome (FBSS) is a complex set of post-surgical pain symptoms encountered after a patient has had surgery on the lumbar spine for disc-related abnormal pathology. The patient may feel present with recurrent pain and persistent pain, with or without radiculopathy, following spinal surgery. Pain may appear after surgery and persist despite the intervention for up to 3 months or more, with chronic pain.[rx] There are other name of this condition definitions for the same disorder such as postlumbar surgery syndrome, postlaminectomy syndrome, failed back syndrome, and postoperative persistent syndrome.[rx,rx]
Failed back surgery syndrome or “failed back syndrome” refers to persistent pain after spinal surgery about 3 months later. It man have a number of serious problems that may including iatrogenic vigorous effects in the spine or incision area such as the development of scar tissue, nerve damage, or weakening of physical structures and posture. A disability may increase and the demand for medication may also increase. This opinion piece will discuss broadly the background and scale of failed back surgery syndrome. There will be a description of the medical and psychological factors that have been reported as causes of poor outcomes from spinal surgery.
Types of Post Surgical Back Pain
Below are the types of back and neck pain people with failed back surgery syndrome may experience. In these cases, some patients have one or more types.
- Chronic pain – It may be sustained significant pain that lasts for more than 12 weeks. Chronic pain is the opposite of acute pain, which is short-term pain that may be severe. Acute pain is expected during spine surgery recovery, but the pain should fade as the spine heals.
- Nociceptive pain – It is a Localized pain that may be dull or sharp. This is the type of pain patients may experience immediately after surgery (eg, the heightened pain felt around the incision site). When most people think of pain, nociceptive pain is what comes to mind.
- Neuropathic pain (neuropathy) – The pain arises due to nerve-related pain is caused by damage to the nerves or spinal cord compression in the root of the nerve. Unlike nociceptive pain, which can be traced to a single site or area, neuropathic pain often shoots and moves, affecting large areas of your body and buttock. Examples of this type of pain include numbness, burning, tingling, weakness, and other abnormal sensations (called paresthesia).
- Radicular pain (radiculopathy) – A subset of nerve pain abnormality (neuropathy) is called radiculopathy, or a group of radicular pain. The characteristic of radicular pain radiate from one area to another (eg, upper back or lumber reason to the low back down the buttocks, legs, and feet, such as sciatica).
Causes of Post Surgical Back Pain
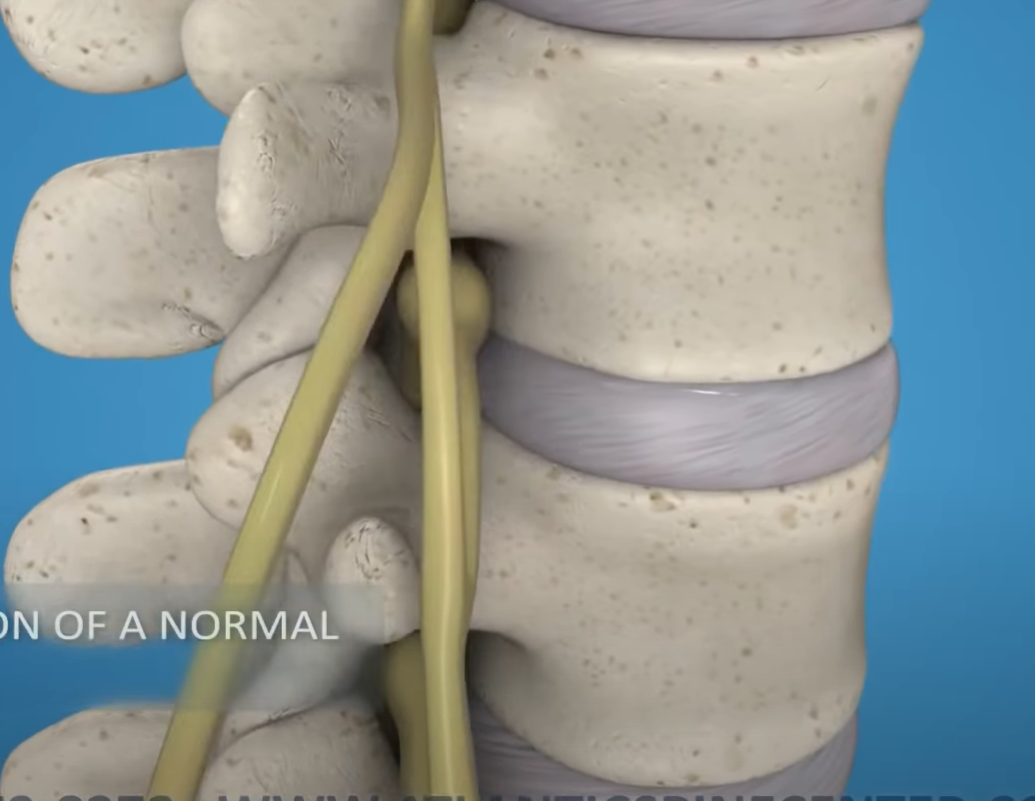
Pain in the leg likely indicates and feel nerve compression from the condition of stenosis, epidural fibrosis, or disc herniation, and it may be more while low back pain is more common in facet joint arthropathy, sacroiliac joint issues, or myofascial etiologies. Failed back surgery syndrome is a condition with a complex etiology and many factors that predispose patients towards chronic pain. These predictive factors generally divide into preoperative (patient) factors, intraoperative factors, and postoperative factors.[rx][rx][rx][rx]
- Preoperative Causes – It is previous and after causes of the patient associated with failed back surgery syndrome include anxiety, depression, or other psychiatric comorbidities, obesity, smoking, the presence of litigation or worker’s compensation claims, and physical or radiologic findings such as stenosis, fibrosis, and disc herniation.[rx][rx]
- Psychosocial causes – It is the second most psychological causes that have been shown to have the strongest association with the development of FBSS.[rx] Additionally, the choice of an inappropriate surgical candidate, or theory and technique, or surgical approach correlates with a higher risk of developing FBSS.[rx] Patients who have undergone multiple prior back surgeries have the highest chance of developing FBSS and a lower chance of achieving successful pain resolution with surgery than surgeons have done.[rx]
- Intraoperative causes – It is the sense for developing failed back surgery syndrome to include operating at either the wrong way surgery vertebral level or operating at a single level while the origin of pain spans several levels, thus providing insufficient pain relief.[rx][rx]
- The wrong vertebral – The Vertebralcoloumn level may pertain to factors such as lumbarization, sacralization, or even more important when the etiology gets attributed to a non-attributable pathological condition. These factors represent the symptoms in clearly identifying a locus in patients with multi-segment changes. Improper technique or unconsciousness during surgery may also lead to failure of the back syndrome to relieve pain or the onset of new pain.[rx]
- Fusion surgery considerations – The surgery to fixed the two adjuvant vertebrae such as failure to fuse and/or implant abnormality failure, or a transfer lesion to another level after a spine fusion, when the next level degenerates more pain and becomes a pain generator.
- Lumbar decompression back surgery considerations – It is such a condition as recurrent spinal canal stenosis, or disc herniation, PLID, inadequate decompression of a nerve root, preoperative nerve damage or postoperative that does not heal after decompressive surgery, or nerve damage that occurs during the surgery)
- Scar tissue considerations – It causes after surgery in such as forming epidural fibrosis, which refers to a formation of scar tissue around the nerve root and spinal column
- Postoperative rehabilitation – Due to adequate consciousness of continued pain from a secondary pain generator.
- Post-Surgery Pain – It is the most dangerous indication of failed back surgery symptoms that happened in past a certain point certain causes of the pain from surgery should begin to remember while the effects of the surgery reducing pain should take hold. If you continue to have the same level of pain or struggle with even more pain, despite 6 weeks of recovery, it’s likely that something went wrong either during or after the procedure of back failed surgery. Your doctor may be advised to stay in touch with a pain management professional or your doctor and with your doctor and to schedule regular checkups to be sure including imaging if you’re left with a significant amount of pain and abnormality about 3 months or more after surgery.
- Nerve Pain – All pain is “nerve pain”, but certain forms of pain due to nerve root compression specifically point towards pinched nerves, recurring disc herniation, failed spinal fusion, or the formation of scar tissue around the surgical site putting pressure on a specific nerve or nerve root all of which are possible symptoms of a failed back symptoms surgery. Each major nerve exhibits and causes different symptoms, but common issues include severe leg pain, the paresthesia to long walk or sitting, running down the side of the leg, lower back pain getting worse, etc.
- Spasms & Joint Lockage – Another bad sign pointing towards failure or the possibility of another issue is joint lockage and muscle spasms. Muscle spasms and cramps are not too uncommon immediately after surgery, but they shouldn’t occur after recovery. If you struggle to bend your leg or get sudden spasms and cramps preventing you from walking, then you must immediately consult a professional.
- Severe Weakness – Nerves are responsible for sending signals into the body from the brain, and lumbar disc herniation often leaves people with limb paresis (partial paralysis or immobility in the limbs). Surgery to correct disc herniation quite often relieves patients of these symptoms and gives them back more control over their limbs. While it isn’t guaranteed that any given patient makes a full recovery, continued muscle weakness – or increased muscle weakness, and partial paralysis – may be a sign of FBSS.
The most non-surgical causes include
- Herniated nucleus propulsors (HNP) at a non-surgical site
- Facet arthrosis
- Spinal Stenosis
- Spondylolysis with or without Spondylolisthesis
- Referred to pain.
- myofascial pain
- segment instability
- Epidural hematoma,
- Recurrent HNP at the operative site,
- Infection such as diskitis,
- Osteomyelitis or arachnoiditis,
- Epidural scar
- Meningocele or CSF fistula.
Symptoms of Post Surgical Back Pain
- Persistent or recurrent pain – in the back/neck or limbs despite surgery or treatment thought likely to relieve pain.
- Chronic radicular pain – that has recurred or persists in the same distribution despite anatomically satisfactory previous spinal surgery. (Leveque)[rx]
- Lumbar (cervical) pain – of unknown origin either persisting despite the surgical intervention or appearing after surgical intervention for spinal (origin) pain originally in the same topographical distribution.[rx]
- Chronic back and leg pain – that persists or recurs despite the application of the back surgery clinical pathway.
- Radicular symptoms – in the failed back patient may be due to a multitude of reasons including herniated disc, postoperative adhesions, a thickened ligamentum flavum, spondylolisthesis with or without an associated par defect, osteophyte formation from facet arthropathy, or other degenerative changes that may lead to central or transforaminal stenosis.
- Original symptoms return – When the symptoms surgery intended to correct come back, it may indicate failed back surgery.
- New problems arise – Spine surgery may have fixed original symptoms, but new pain (pain in a different part of the spine or a different type of pain) warrants a discussion with your doctor.
- Reduced mobility – It takes time to recover from spine surgery and that process can affect your endurance, flexibility, and movement. However, reduced mobility or limitations in movement that is different from expected or develops after the recovery period should be discussed with your doctor. An example is a limited range of motion in your neck or low back.
- Headaches develop – If they weren’t part of your medical history before your surgery, the headache may signal a nerve problem after a cervical spine (neck) procedure.
The symptoms that may indicate life-threatening conditions; include, but are not limited to: saddle anesthesia or bowel/bladder incontinence, indicative of cauda equina syndrome; fever, chills, or weight loss indicating infection; and signs of malignancy.[rx][rx] Patients should also have an evaluation for anxiety, depression, and other psychiatric conditions due to their high comorbidity with FBSS.[rx]
Diagnosis of Post Surgical Back Pain
An accurate and thorough history and physical examination of patients with persistent pain after lower back surgery are the most crucial for correct diagnosis.[rx] [rx]
History
- Allow extra time to evaluate initially or properly
- Essential to have prior records of medical record
- Preoperative vs.Postoperative complaints and associate test
- Was there a new problem immediately after surgery or not?
- Current medication usage and issues of dependency.
- Careful assessment of the psychological status
- Vocational status and workers’ compensation
- Postoperative systemic complaints(often subtle)
- Back vs Leg pain that radiates or not
- Unusual pain pattern (reflex sympathetic dystrophy, complex regional pain, )
- Postoperative rehabilitation (aerobic, flexibility, strengthening, body mechanics, physical therapy).
- Relieving and exacerbating positions and activities.
Physical Examination
- Observe closely for pain behavior as a warning of associated problems.
- Careful neurologic exam for focal localizing findings.
- Evaluate for the potential major joint problem as referral source (hip, knee)
- Palpation at surgery site for hematoma, local fluid, abscess, and pseudo meningocele.
- Examination of extremity for sympathetic or RSD -type changes.
- Screening for neural tension signs (SLR, Adson’s test)
- Long tract signs (Babinski’s sign, clonus, Hoffman’s sign)
- Vascular assessment (diabetics, elderly patients)
- Local soft tissues (psoas muscle, iliotibial band, gluteal muscles)
Manual Examination
- Straight Leg Raising Test – A manual test for pain from a disc herniation or nucleus proposal may present with a positive sign on straight leg raise.[rx] Focal neurological deficits in FBSS patients warrant further testing.[rx] Deficits in strength or sensation in the lower extremities may help narrow down which nerve roots are affected and cause pain.[rx]
- Waddell signs – are one of the vital manual tests that can be used to evaluate for psychogenic etiology of lower back pain; while the interpretation of these tests is controversial, they may be useful especially if there is a suspicion of secondary gain.[rx][rx]
- One leg hyperextension test/stork test – It a simple and manual or home test the patient can do it own have the patient stand on one leg and (while being supported by the provider) have them hyper-extend their back. Repeat this maneuver on both sides. If pain with hyperextension is the resulting increase positive for a pars interarticularis defect or associate abnormalities.[rx]
- Adam test – Patient has to bend over with feet together and arms extended with palms together. The practitioner should observe from the front side of you. If a thoracic lump is present on one left side or the other right side lower back pain, it is an indication of scoliosis.[rx] There are numerous other examination techniques; however, they have mixed and anonymous evidence for inter-practitioner reliability and poor sensitivities or specificities lower back pain.[rx][rx][rx][rx]
Lab test
- Blood tests – CBC, Hb, RBS, CRP, Serum Creatinine, Serum Electrolyte.
- Erythrocyte sedimentation rate and C-reactive protein – may be used to evaluate for possible infection, especially in patients with constitutional symptoms or a predisposition towards infection.[rx] .[rx] Adherence to strict standards of accurate needle placement, contrast injection, as well as a limited active agent is essential in improving the sensitivity and specificity of these blocks.
- Bone scan – It is a bone scan that may be used for detecting bone tumors or compression of nerve root fractures caused by brittle bones and osteoporosis. The patient may receive an injection of a tracer (a radioactive substance) into a vein at the same time. The tracer collects or examiner in the bones and helps the doctor detect bone problems with the aid of a special camera.
- Electromyography (EMG) – It one kind of test that helps assess the electrical activity in a muscle and nerve impulse velocity or nerve root compression and can detect if muscle weakness results from a problem with the nerves that control the muscles. Very fine needles are inserted in muscles to measure electrical activity transmitted from the brain or spinal cord to a particular area of the body that are causing pain.
- Evoked potential studies – It may involve two sets of electrodes are placed one set to stimulate a sensory nerve, and the other placed on the scalp to record the speed of nerve signal that is transmitted to the brain.
- Nerve conduction studies (NCS) – It also uses two sets of electrodes to stimulate the nerve that runs to a particular muscle and record the nerve’s electrical signals to detect any nerve damage for lower right and left side back pain.
- C-Reactive Protein (CRP) – CRP is another blood test that shows acute inflammation. Higher CRP levels may indicate infection (like discitis) or inflammatory diseases (such as arthritis) that can weaken the disc’s outer layer and mimic or complicate a herniation diagnosis.
- Complete Blood Count (CBC) – A CBC counts different types of blood cells, including white blood cells (which fight infection). If the white cell count is high, it could signal an infection in the spine. In a straightforward herniation without infection, the CBC usually remains normal.
- Blood Cultures – If there’s suspicion of a bacterial infection in the disc space (discitis), the doctor may draw blood to test for bacteria. Positive blood cultures can confirm that germs are spreading through the blood to the spine, which might cause a disc to weaken and herniate secondarily.
- Rheumatoid Factor (RF) – RF is an antibody often elevated in people with rheumatoid arthritis, an autoimmune condition that causes chronic joint inflammation. If RF levels are high, it suggests that arthritis might be affecting spinal joints and possibly contributing to disc degeneration and herniation.
- Antinuclear Antibody (ANA) Test – The ANA test looks for autoantibodies that attack the body’s own cells. A positive ANA can point to systemic autoimmune diseases, such as lupus, that may inflame supporting tissues of the spine and lead to disc problems.
- HLA-B27 Testing – HLA-B27 is a genetic marker associated with inflammatory spondyloarthropathies like ankylosing spondylitis. If you have back pain and a positive HLA-B27, your doctor may investigate whether chronic inflammation and abnormal spinal alignment contributed to a thoracic disc herniation.
- Serum Protein Electrophoresis (SPEP) – SPEP examines different proteins in your blood. Abnormal patterns can indicate certain cancers (like multiple myeloma) that weaken bone and discs. If a tumor or cancerous process is suspected to cause a herniation, SPEP helps check for abnormal protein levels in the blood.
- Tumor Marker Tests (e.g., CEA, PSA) – Tumor markers are substances produced by cancer cells. Elevated levels of specific markers—such as carcinoembryonic antigen (CEA) in colon cancer or prostate-specific antigen (PSA) in prostate cancer—might indicate that a metastatic tumor has invaded the vertebral column and weakened the disc structure.
- Cerebrospinal Fluid (CSF) Analysis – If spinal cord compression is severe, your doctor may perform a lumbar puncture to collect CSF. Analysis can rule out infections, inflammatory conditions (like meningitis), or bleeding that could present with similar neurological symptoms as a herniated disc.
- Disc Tissue Biopsy – If imaging or lab tests suggest infection or tumor involving a disc, your doctor may obtain a small sample of disc material through a needle guided by CT or fluoroscopy. Examining the tissue under a microscope can confirm infection (discitis) or malignancy as the underlying cause of disc weakening.
- Bone Turnover Markers – Certain blood or urine tests measure how quickly bone is breaking down or forming. Abnormal levels might suggest osteoporosis or other metabolic bone diseases that can alter vertebral shape and indirectly increase stress on the discs, predisposing them to herniation.
- Vitamin D Level – Low vitamin D can weaken bones and muscles, leading to poor spinal support. A deficiency may contribute to degenerative changes in the thoracic spine, making disc herniation more likely. Measuring vitamin D helps identify and correct this risk factor.
- Thyroid Function Tests (T3, T4, TSH) – An underactive thyroid (hypothyroidism) can slow metabolism, leading to weight gain and muscle weakness. Both factors increase stress on spinal discs. By checking thyroid hormones, the doctor rules out metabolic causes that might indirectly weaken discs.
- Blood Glucose (Fasting and HbA1c) – Diabetes can damage blood vessels that supply the discs, accelerating degeneration. Measuring fasting blood sugar or hemoglobin A1c levels provides insight into long-term blood sugar control and whether diabetes might be contributing to disc health problems.
- Lyme Disease Serology – Lyme disease, caused by a tick-borne bacterium, can infect joints and sometimes the spine. If a patient at risk for tick exposure complains of mid-back pain and neurological signs, Lyme serology helps determine if an infection could have weakened the disc.
- Brucellosis Serology – Brucellosis is an infection common in certain agricultural regions. It can infect the spine, causing discitis and weakening discs. A positive Brucella antibody test suggests that a bacterial infection might be the root cause of thoracic disc degeneration and herniation.
- HIV Testing – HIV weakens the immune system, making patients more prone to opportunistic infections—including those that can affect the spine. If an infection is suspected in a patient with risk factors or HIV, testing confirms status and guides treatment plans to protect disc health.
- Serum Calcium and Phosphate Levels – Abnormal calcium or phosphate levels can signal conditions like hyperparathyroidism, which weakens bones. When vertebrae are porous or fragile, they can collapse slightly and change disc loading, indirectly increasing the risk of disc herniation.
- Lateral Mass Biopsy (for Suspected Tumor) – For cases where imaging suggests a spinal tumor is pushing on thoracic discs, a minimally invasive biopsy of suspect vertebral bone may be performed. Examining this bone under a microscope confirms whether cancer is present, which might alter how a herniation is managed.
- Tuberculosis (TB) Screening (PPD or IGRA) – Spinal tuberculosis (Pott’s disease) can destroy vertebral bodies and discs. A positive skin test (PPD) or blood test (IGRA) for TB, along with other signs, indicates that an infection may be weakening the disc and causing a herniation.
- Hepatitis B and C Serology – Chronic liver infections can cause inflammation and weaken the immune system. If a patient with chronic hepatitis complains of spinal pain and shows signs of infection, these blood tests help confirm that infection might be related to discitis and secondary herniation.
- Syphilis Serology (RPR/VDRL) – Syphilis can affect the spine in advanced stages, leading to bone or disc damage. If suspected based on risk factors or clinical signs, testing for syphilis antibodies helps determine if an untreated infection could be underlying a thoracic disc problem.
- Autoimmune Panel (ENA Panel) – An extractable nuclear antigen (ENA) panel includes tests for antibodies seen in autoimmune diseases like lupus or mixed connective tissue disease. If an autoimmune process is suspected to inflame spinal tissues, this panel helps clarify whether the disc herniation is related to systemic autoimmunity.
Electrodiagnostic Tests
- Electromyography (EMG) – EMG measures the electrical activity of muscles at rest and during contraction. Small needles are placed into various muscles innervated by thoracic nerve roots. If the herniated disc compresses a nerve, EMG can detect abnormal electrical signals in the muscles served by that nerve.
- Nerve Conduction Study (NCS) – NCS tests how fast electrical signals travel through specific peripheral nerves. In thoracic disc herniation, doctors may use NCS to rule out other causes of chest wall pain (like peripheral neuropathy). Normal conduction speeds combined with abnormal EMG at certain muscles help localize the lesion to the thoracic spine.
- Somatosensory Evoked Potentials (SSEPs) – During an SSEP, small electrodes are placed on the scalp and a peripheral nerve (for example, in your leg). A brief electrical pulse is sent along the nerve, and the response is recorded at different points in the central nervous system. If the thoracic spinal cord is compressed, the signal traveling through that segment is slowed or reduced in amplitude, indicating a problem.
- Motor Evoked Potentials (MEPs) – MEPs measure the electrical response of muscles after stimulating the motor cortex in the brain using magnetic or electrical pulses. Delayed or diminished responses in muscles of the abdomen or legs suggest that the spinal cord pathway through the thoracic region is compromised by a herniation.
- F-Wave Studies – F-waves are a specific type of response measured during NCS. A brief stimulus is sent to a nerve, and the resulting signal that travels back to the spinal cord and then returns to the muscle (an F-wave) is recorded. Prolonged F-wave latency can indicate that there is compression of the spinal cord or roots in the thoracic region.
Imaging Tests
- X-rays – are a simple and inexpensive first imaging evaluation to detect the bone and vertebrae related problem for suspected failed back surgery syndrome. X-rays are more specific use for detecting vertebral and sacroiliac defects and/or misalignment and are superior to MRIs for the detection of spondylolisthesis.[rx] Adjacent segment degeneration and loss of lordosis are common abnormalities found on radiography.[rx] However, X-rays are unable to detect spinal stenosis, the most common pathological finding in FBSS, and are also unable to evaluate soft tissue, such as intervertebral discs, epidural scarring, or fibrosis.[rx][rx]
- MRI – with and without gadolinium contrast is one of the latest tests that continues to be the gold standard imaging modality for failed back surgery syndrome due to its excellent ability to detect soft tissue abnormalities such as epidural fibrosis and disc herniation.[rx][rx] Contrast is especially indicated in patients with a history of disc herniation surgery.[rx] In patients with ferromagnetic implants, a CT myelogram is used to avoid implant artifacts created on MRI.[rx][rx]
- CT myelography -It is a special kind when the patient has either a contraindication to having an MRI such as heart problem, open-heart surgery, or having a pacemaker device or defibrillator or be used when a standard CT or MRI is negative or equivocal. Myelography is a CT scan or an MRI with intrathecal administration of contrast for lower back pain. CT myelography visualizes a patient’s spinal nerve roots in their passage through the neuroforamina area. CT myelography can be used to assess the underlying root sleeve and nerve root compression. A CT is a poor test for the visualization of nerve roots, making it challenging to diagnose radicular disease.[rx][rx]
- Electromyography (EMG) – It is complete after three weeks of symptoms, not before the lower right and left back pain. Diagnostic tests such as EMG or nerve conduction studies are accurate only after three weeks of persistent symptoms of right or left lower back pain. The primary reason or why using an EMG or nerve conduction study is to identify the delayed three weeks or more time following the development of pain is because of fibrillation potentials after an acute injury in the brain and spinal cord lead to an axonal motor loss. These do not develop until two to three weeks following injury for the lower right and left back pain.[rx][rx]
- Cerebrospinal fluid analysis – It is a useful test for investigating the right and left lower back pain if there is an involvement of neoplasm or infectious cause or radiculopathy symptoms and radiating pain syndrome. The recommendation for lower right and left back pain in lumbar puncture is in the case of a patient with negative or nondiagnostic neuroimaging, without knowing primary cancer and its related condition, who has progressive neurological symptoms and has failed back syndrome to improve it properly.[rx]
- Bone scintigraphy – It is a special type of test that is done when some or above mention test failed to identify the causes of right and left lower back pain with single-photon emission computed tomography (SPECT) is more sensitive in detecting facet joint lesions and bony lesion, none spurs and allows more accurate anatomical localization of lower back pain. A recent study suggested that SPECT could help to identify patients with lower back pain who would benefit from facet joint intraarticular injections [rx]. Facet joint block (FJB)injection is an indispensable diagnostic instrument in order to identify painful or painless back pain from painless facet joints and to plan the intervention strategy.
- Foraminal nerve root entrapment test – It is best visualized on T1-weighted MRI where are used to identify the high contrast fat tissue and the nerve root sheath that is of great help for lower and right or left ba. In here usually, a combination of hypertrophic degenerative facets with osteophytes spurs posteriorly, and vertebral osteophytes and/or disc herniation anteriorly diminishes the anteroposterior diameter of the foramen and it associate condition. Foraminal height is erased by degenerative disc disease and subsequent disc height loss or not. In this case, the normal rounded (oval) appearance of the nerve root sheath is lost in combination with loss of the surrounding fat tissue, nerve root compression should be considered to identifying the lower right and left side back pain.
- Plain Radiograph – A standard X-ray of the thoracic spine is often the first imaging test done. While X-rays cannot directly show a disc herniation, they can reveal bone abnormalities—such as spinal alignment, fractures, or calcified (ossified) discs—that suggest possible disc issues.
- Flexion-Extension X-Rays – These specialized X-rays are taken while you bend forward (flexion) and backward (extension). They help reveal abnormal motion between vertebrae (instability) that may contribute to disc herniation. If one segment moves excessively, the disc in that area is likely strained or damaged.
- Computed Tomography (CT) Scan – A CT scan uses X-rays to create detailed cross-sectional images of the spine. CT can show both bone structures and the outline of calcified disc fragments. It can identify bone spurs, small fractures, or calcified herniations that might not appear on a plain X-ray.
- Magnetic Resonance Imaging (MRI) – MRI is the best test to directly visualize a disc herniation. It uses powerful magnets and radio waves to create detailed pictures of soft tissues, including intervertebral discs, spinal cord, and nerve roots. On MRI, a herniated thoracic disc appears as a bulging or extruded disc pressing on neural structures.
- CT Myelography – In a CT myelogram, a contrast dye is injected into the space around the spinal cord (the subarachnoid space) before performing a CT scan. The dye highlights the spinal canal on images, showing how a herniated disc deforms the spinal cord or nerve roots. It is useful if a patient cannot have an MRI.
- Myelography (Fluoroscopic Myelography) – This older technique involves injecting contrast dye into the spinal canal and viewing real-time X-ray (fluoroscopy) images. As you tilt or move, the dye outlines the spinal cord and can reveal where a disc herniation causes a blockage or indentation. Although less common now, it can help when MRI is contraindicated.
- Discography (Provocative Discogram) – During discography, contrast dye is injected directly into the suspected thoracic disc under X-ray or CT guidance. If the injection reproduces your typical pain and the dye outlines a tear or fissure in the disc, it confirms that the disc is the pain source. However, this test is used sparingly due to its invasive nature.
- Ultrasound (Musculoskeletal Ultrasound) – While ultrasound cannot directly visualize a thoracic disc, it can help rule out other causes of chest or back wall pain, such as soft tissue injuries (muscle or ligament tears). A normal ultrasound in the presence of persistent pain increases suspicion that pain originates from deeper structures like the discs.
- Bone Scan (Technetium-99m Bone Scintigraphy) – A bone scan involves injecting a small amount of radioactive tracer into your bloodstream. Areas of increased bone activity—such as from infection, inflammation, or tumor—absorb more tracer and appear “hot” on the scan. While not specific for a herniated disc, a bone scan can detect conditions that weaken vertebrae and affect discs.
- Positron Emission Tomography (PET) Scan – A PET scan uses a special tracer that highlights areas of high metabolic activity, such as cancerous lesions. If a tumor is suspected to be causing disc weakening or herniation, a PET scan helps locate active cancer cells in the spine or elsewhere in the body.
- Single-Photon Emission Computed Tomography (SPECT) – SPECT is a nuclear imaging test similar to a bone scan but provides three-dimensional images. It can detect early changes in bone metabolism around the disc, indicating conditions like infection or tumor that may have contributed to a herniation.
- Fluoroscopy-Guided Injections (Diagnostic Discography Alternative) – For patients who cannot tolerate a full discogram, the doctor can use fluoroscopic guidance to inject a small amount of contrast dye or anesthetic near the suspected disc. If your typical pain temporarily subsides after numbing that disc, it supports the diagnosis of a symptomatic herniation.
- CT with Multi-Planar Reconstruction – This advanced CT technique reconstructs images in multiple planes (sagittal, coronal, and axial) to give a clearer view of the disc herniation location and its relationship to the spinal cord. It’s especially helpful for planning surgical approaches when the herniation is complex or calcified.
- Digital Subtraction Angiography (DSA) for Vascular Assessment – In rare cases when a herniated disc is near major blood vessels, or if vascular malformation is suspected, DSA can visualize blood flow around the spine. This helps ensure that surgical removal of a herniated disc does not endanger spinal arteries.
- Dynamic MRI (Kinematic MRI) – Dynamic MRI captures images while you move your spine slightly, such as bending forward or backward. This can reveal herniations that only press on the spinal cord or nerves during certain positions, helping explain why some patients have pain or numbness only when bending or twisting.

Treatment of Post Surgical Back Pain
Non-Pharmacological Treatment for failed back surgery syndrome
- Physical therapy – Physical therapy can help the patient optimize gait and posture and can improve muscle strength and physical function.[rx,rx] Other conservative measures that may help postoperative back pain involve psychotherapy measures including stress reduction and cognitive behavioral therapy to body and mind fit.[rx] Finally, noninvasive procedures or systems including acupuncture and scrambler therapy can be used to minimize the pain associated with FBSS.[rx,rx] These conservative measures should be done in conjunction with medication management to optimize pain relief.
- Transcutaneous electrical nerve stimulation – may provide an alternative/complement to medication in patients with FBSS. Its effectiveness in chronic low back pain is, however, still have controversial [rx, rx]. Other nonpharmacological complementary therapies, such as acupuncture, manual therapy, functional restoration, and cognitive behavioral therapy, may also be utilized, although the level and supporting team most of these therapies in the management of chronic back pain is moderate at best [rx, rx].
- High-frequency spinal cord stimulation – This technique has been shown to be of particular value in patients with FBSS with a predominant lower back pain component.[rx]A frequency of about 5000–10,000 Hz is used. A major advantage is that patients do not have to rely on the perception of paraesthesia, itching in the affected area. There are no efficacy, cost-effectiveness, or safety data from a randomized controlled trial or comparison with conventional SCS in relation to the long-term use of this technology.
- Dorsal root ganglion stimulation – A specially designed lead is placed around the dorsal root ganglion, via the epidural space, and this produces pleasant paraesthesia in a dermatome or part of it. The major advantages seem to be that there is no change in perception of paraesthesia with posture, and it is possible to target dermatomes that would otherwise be difficult to target with conventional SCS (foot, groin, etc.) without overspill of paraesthesia into other dermatomes. There are minimal long-term data regarding efficacy, safety, and cost-effectiveness.[,rx]
- Peripheral nerve field stimulation – Specially designed leads have been approved for this use, especially for treating the neuropathic back pain component of FBSS. The use of this technique, in combination with conventional SCS or alone, has been published with impressive results in case series.[rx] However, cost-effectiveness and long-term efficacy are not established.
- Radiofrequency ablation – RFA of nerves are often used to provide sustained relief that a diagnostic block or therapeutic injection cannot provide. Successfully targeting the intended nerve is achieved, maximizing the size of the lesion. This can be done by performing multiple RFA in different locations, increasing the temperature and time of the ablation, using bipolar RF or cooled RF.[rx,rx]
- Neuromodulation – Spinal cord stimulation (SCS) is a treatment modality that has shown tremendous potential in the management of FBSS. The advent of SCS came just 2 years after Melzak and Wall’s 1965 groundbreaking paper on Gate Theory with Shealy and Mortimer’s case study on the complete elimination of pain in a 70-year-old male with metastatic bronchogenic carcinoma by means of electrical stimulation of the dorsal columns.[rx,rx]
- Chiropractic – The results of several studies showed significant improvement for patients with failed back surgery who were managed with chiropractic care
Medications
Oral pharmacological treatment of FBSS is multimodal and increasingly controversial.
- Anticonvulsant drugs – have gained popularity for neuropathic pain, with gabapentin (Neurontin) and pregabalin (Lyrica) being the most commonly used preparations. Gabapentin has been shown to be superior to naproxen in alleviating back and leg pain after spinal surgery [rx]. Pregabalin plays a role in the prevention of pain before and after surgery, with its effect apparently increasing with time [rx].
- Antidepressants – (amitriptyline and duloxetine) [rx]. Two-drug combinations for the treatment of neuropathic pain in adults have been shown to improve analgesic efficacy [rx].
- Chemical neuromodulation – by continuous intrathecal drug delivery (IDD) based on morphine or ziconotide administration may be considered for patients preferentially with neuropathic pain who have responded to strong oral opioids in the presence of severe adverse events [rx–rx]
- Epidural injections – Epidural steroid injections (ESIs) are the most commonly performed procedure in pain clinics around the world.[rx] These can be administered primarily by three approaches: transforaminal, interlaminar, or caudally, and are indicated for symptoms of radiculopathy.
- Intrathecal drug delivery – Similar to a spinal cord stimulator, spinal drug delivery (or intrathecal drug delivery) involves implanting a small pump in the stomach and running a catheter to the spine to deliver pain medication. It is used for people with chronic back pain who need large doses of narcotics to deal with the pain. Compared to oral medication, this “pain pump” requires a smaller dose of narcotics because the medication goes directly to the area of pain.
- Long-term Oxycodone – Naloxone is given to counteract the long-term effects of narcotic use. In one case study, Spanish research Dr. Borja Mugabure Bujedo recorded that a combination of Oxycodone – naloxone can be a good alternative for the management of Failed Back Surgery Syndrome when other interventional or pharmacologic strategies have failed in a case report in the journal Anesthesiology and pain medicine. In this case report, higher doses than those recommended as a maximum daily ceiling (80/40 mg) were used in one selected patient with severe pain.[rx]
- Platelet Rich Plasma Therapy in combination with Prolotherapy – Some doctors may recommend the use of Platelet Rich Plasma to help patients with failed back surgery syndrome. Platelet Rich Plasma is an injection of your concentrated blood platelets into the area of pain. The concentrated blood platelets bring healing and regenerating growth factors to the areas possibly damaged or affected by surgery. Recent research says that
- Platelet-rich plasma (PRP) represents an additional approach – as it has shown some promise in bone regeneration, and should be explored for its potential role in limiting spinal fusion surgery failures.[rx]
Why Does Failed Back Syndrome Happen?
One of the most common situations in which we see failed back syndrome is after spinal fusion surgery. The spine is not immediately, fully fused after spinal fusion; rather, surgeons have created an environment that encourages fusion, through the use of a tissue graft between two (or more) vertebrae.
For the vertebrae to fully fuse, the spine must be stabilized and immobilized to a degree. If the environment for growing new bone tissue is not quite right, the spinal fusion may prove ineffective. This is one of the main causes of the failed back syndrome.
Another common scenario happens after a discectomy or laminectomy to relieve symptoms of a herniated disc when the patient has degenerative disc disease (DDD). The surgery may have been performed flawlessly, but DDD can affect multiple locations in the spinal column.
Sometimes patients have one disc herniation repaired only to find that another herniation has occurred after recovery from the surgery, or a more minor existing herniation was being masked by stronger symptoms, which the surgery addressed.
The risk of failed back syndrome rises with each surgery. According to a 2018 review in Asian Spine Journal, about half of initial surgeries are successful. That percentage, however, drops to 30 percent, then 15 percent, then 5 percent after the second, third, and fourth surgeries.
Aside from the choice of surgery, the number of surgeries, and the presence of other spinal conditions, the risk of the failed back syndrome can be increased by a number of factors after surgery. In the short-term, some of these include:
- Infection
- Nerve injury
- Hematoma formation
In later stages, changes to the spinal column can affect the way a patient moves, which can cause further spinal problems after time.
What exercises help reduce Failed Back Syndrome pain?
There are 4 exercises your spine specialist may recommend helping you reduce failed back pain nerve pain caused by degenerative disc disease: pelvic tilt, knee to chest, lower trunk rotations, and all fours opposite arm and leg extensions. Each low-impact exercise is demonstrated in narrated videos and written instructions are provided to help you fine-tune your sciatica home exercise program.
Pelvic Tilt
Purpose: To strengthen the lower abdominal muscles and stretch the low back.
How to perform a pelvic tilt
- Lie on your back.
- Exhale and tighten your abdominal muscles while pushing your belly button toward the floor and flatten your lower back.
- Hold the position for 5 seconds.
- Repeat the pelvic tilt 10 times holding the position for 5 seconds each time.
How can I tell if I’m doing the pelvic tilt right?
- Place your pinky finger on your hip bone and thumb on your lowest rib (same side of your body).
- As you tighten your abdominal muscles, the amount of space between your pinky finger and thumb should get smaller.
Knee to Chest
Purpose: To help reduce nerve compression in your low back, which may help alleviate lower back pain.
- Lie on your back.
- Starting with either your left or right knee and use your hands to gently pull the bent knee toward your chest.
- Hold for 10 seconds.
- Repeat the movement with the opposite knee.
- Perform the movement 3 to 5 times holding the position for 10 seconds each time.
- Next, use your hands to gently pull both knees toward your chest.
- Hold for 10 seconds.
- Repeat the movement with both knees 3 to 5 times holding the position for 10 seconds each time.
Lower Trunk Rotations
Purpose: To increase your spine’s mobility and flexibility.
- Lie on your back with both knees bent upright and both feet flat on the floor (called the hook lying position).
- While holding both knees together, rotate your knees to one side and hold for 3 to 5 seconds. You will feel a gentle stretching sensation on the opposite side of your lower back and hip area.
- Next, contact your abdominal muscles and rotate both knees to the opposite side and hold for 3 to 5 seconds.
- Repeat up to 10 times on each side.
All Fours Opposite Arm and Leg Extensions
Purpose: To strengthen your abdominal muscles, low back, and stabilize those areas.
- Begin by positioning yourself on all fours.
- Contract your abdominal muscles to help keep your back flat and straight.
- Raise one leg upward behind you and straighten in outward.
- Hold for 3 to 5 seconds.
- Repeat the movement on your opposite side.
When you can perform this exercise 10 times with tolerable pain, you can add arm movement with each leg extension:
- Extend the arm (opposite side from the leg) upward and outward in front of your body.
- Hold for 3 to 5 seconds.
- Repeat on the opposite side.
- Perform this exercise up to 10 times.
How can these exercises work to reduce sciatic pain?
The abdominal and spinal muscles are essential components of the spine’s support system, which—anatomically, can be likened to your internal spinal brace. These 4 low-impact exercises, when performed correctly and under your spine specialist’s guidance, can help strengthen your spine and increase its flexibility and range of motion. While you cannot halt the effects of degenerative disc disease (eg, cause of bulging or herniated disc), exercise can help fortify the spine’s structural components that may reduce pain and speed healing.
Furthermore, exercise causes your body to release endorphins—hormones that interact with pain receptors in the brain that can reduce the perception of pain.
References