Ankylosing Spondylitis (Bechterew’s disease or Marie Struempell disease as it is also known) is a form of chronic, degenerative arthritis that affects the spine and sacroiliac joints and often other joints of the body.
Ankylosing spondylitis is a chronic inflammatory rheumatic disorder that primarily affects the axial skeleton. Sacroiliitis is its hallmark, accompanied by inflammation of the entheses (points of union between tendon, ligament, or capsule and bone) and formation of syndesmophytes, leading to spinal ankylosis in later stages. The pathogenesis of AS is poorly understood. [Rx]However, immune-mediated mechanisms involving human leucocyte antigen (HLA)-B27, inflammatory cellular infiltrates, cytokines (for example, tumor necrosis factor α and interleukin 10), and genetic and environmental factors are thought to have key roles. The detection of sacroiliitis by radiography, magnetic resonance imaging, or computed tomography in the presence of clinical manifestations is diagnostic for AS, although the presence of inflammatory back pain plus at least two other typical features of spondyloarthropathy (for example, enthesitis and uveitis) is highly predictive of early AS. Non-steroidal anti-inflammatory drugs (NSAIDs) effectively relieve inflammatory symptoms and are presently first-line drug treatment.[Rx]

What is Ankylosing Spondylitis?
Ankylosing Spondylitis (Bechterew’s disease or Marie Struempell disease as it is also known) is a form of chronic, degenerative arthritis that affects the spine and sacroiliac joints and often other joints of the body. The cause is currently unknown although there is a hereditary factor.

No two cases of AS are exactly the same. Variations occur in the distribution of pain, stiffness, inflammation, and in the length of flare-ups and course of the disease. In some cases, the disease becomes less active and pain may cease altogether.
Anatomy of Ankylosing Spondylitis
Ankylosing spondylitis is a systemic disease, meaning it can affect the entire body in some people. It can cause fever, loss of appetite, and fatigue, and it can damage other organs besides the joints, such as the lungs, heart, and eyes. Most often though, only the low back is involved.
The eye is the most common organ affected by ankylosing spondylitis. Eye inflammation (iritis) occurs from time to time in one-fourth of people with ankylosing spondylitis. Iritis results in a red, painful eye that also leads to photophobia, increased pain when looking at a bright light. It is a potentially serious condition requiring medical attention from an ophthalmologist. Luckily, it rarely causes blindness but it can affect vision while the inflammation is present.

Less frequently, ankylosing spondylitis may be associated with a scaly skin condition called psoriasis. In rare cases, typically when the ankylosing spondylitis has been present for many years, ankylosing spondylitis may cause problems with the heart or lungs. It can affect the large vessel called the aorta that moves blood from the heart into the body. Ankylosing spondylitis can cause inflammation where the heart and aorta connect leading to possible enlargement of the aorta.
Symptoms similar to that seen in ankylosing spondylitis may also occur along with such conditions as psoriasis, inflammatory bowel disease, or Reiter’s syndrome. It is thought that bowel inflammation is somehow tied to the development of ankylosing spondylitis and this is the reason that people with inflammatory bowel disease, i.e. Crohn’s disease or ulcerative colitis are at an increased risk of the illness. Ankylosing Spondylitis has distinct pathological changes at the enthesis, i.e. the area in which a ligament or joint capsule attaches to the bone.
The inflammatory component of this disease causes bony erosions at the enthesis. The body seeks to repair these erosions, and this repair activity results in ossification at these sites. It is this inflammation-repair process that is the basis for many of the findings in Ankylosing Spondylitis.
Ankylosing Spondylitis is usually diagnosed during the second to fourth decade of life. It is more common in first-degree relatives of those with Ankylosing Spondylitis. While a strong affiliation with the HLA-B27 antigen supports a genetic predisposition, the evidence suggests that other factors also play a role in susceptibility to Ankylosing Spondylitis. The HLA-B27 antigen is a generic maker found in 8% of North Americans of European (white) heritage. Of those who are HLA-B27 positive, the actual risk of developing Ankylosing Spondylitis is estimated to be 1 to 2 %. Only 20% of HLA-B27 positive first-degree relatives of individuals with Ankylosing Spondylitis and who are positive for HLA-B27 will develop the disease.
Causes of Ankylosing Spondylitis

www.rxharun.com
The exact cause of ankylosing spondylitis is unclear. It is thought to be an autoimmune disease – where the body’s own immune system attacks the body’s tissues causing inflammation and tissue damage.
Genetic (inherited) factors appear to influence development of AS. Approximately 90% of people diagnosed with AS have a gene called HLA-B27. However only about 10 – 15% of people with the gene will go on to develop AS. Approximately one in five individuals with AS also has a relative with the condition.
The information cited below is not binding. Each case should be adjudicated on the evidence provided and its own merits.
- Idiopathic – The precise etiology is unclear.
- Genetic – Although the precise cause of Ankylosing Spondylitis is unknown, there is a strong genetic component, i.e. HLA-B27. Significant physical traum – aggravation only Significant physical trauma will produce aggravation only in the site that is affected by significant physical trauma. For significant physical trauma to produce aggravation of Ankylosing Spondylitis, the following should be evident: Significant physical trauma must occur to an area of the body where Ankylosing Spondylitis is active; Increased signs/symptoms of Ankylosing Spondylitis must be present on a continuous or recurrent basis for at least 6 months. Significant physical trauma is a discrete injury that causes, within 24 hours of the injury being sustained, the development of acute symptoms and signs for which medical attention would normally or reasonably be sought.
- The cause of ankylosing spondylitis (AS) is unknown – It’s likely that genes (passed from parents to children) and the environment both play a role. The main gene associated with the risk for AS is called HLA-B27. Having the gene doesn’t mean you will get AS. Fewer than 1 of 20 people with HLA-B27 gets AS. Scientists recently discovered two more genes (IL23R and ERAP1) that, along with HLA-B27, make it more likely you will get AS.
Inability to obtain appropriate clinical management. Medical Conditions Which Are To Be Included In Entitlement / Assessment
- Chronic Mechanical Lumbar/Thoracic (Dorsal)/Cervical Pain
- Peripheral arthritis due to ankylosing spondylitis
- Enthesitis
Common Medical Conditions Which May Result In Whole Or In Part From Ankylosing Spondylitis
- Restrictive lung disease
- Cauda equina syndrome
- Post-traumatic intervertebral fractures (the C5-C6 or C6-C7 level is the most commonly involved site)
- Osteoporosis
- Uveitis
- Aortic regurgitation
- Cardiac conduction abnormalities
- Atlantoaxial subluxation
- IgA nephropathy
Researchers do not know the cause of ankylosing spondylitis. However, studies show that both genes and environment may lead to the development of the disease. Researchers know that the HLA-B27 gene increases the risk of developing ankylosing spondylitis, but this does not mean you will get the disease if you have the gene. Many people have the gene and never develop ankylosing spondylitis, which tells researchers that environmental factors also play a role.
Researchers continue to discover many other gene variations that may cause the disease; however, HLA-B27 is the primary gene that increases your risk for developing ankylosing spondylitis.
Symptoms of Ankylosing Spondylitis
General symptoms-
- Pain, stiffness, and inflammation in other joints, such as the ribs, shoulders, knees, or feet.
- Difficulty taking deep breaths if the joints connecting the ribs are affected.
- Vision changes and eye pain due to uveitis, which is inflammation of the eye.
- Difficulty bending the spine
- Pain in the hips and difficulty walking- dull diffuse type of pain
- Pain in the heels and soles of the feet- pain is worse in morning and night and better after a warm shower
- Bent-over posture
- Straightening of the normal curvature of the spine
- Fever- In the early stages of the disease, there may be a mild fever, loss of appetite, and general discomfort
- Loss of appetite, weight loss
- Fatigue decreased energy
- Eye swelling, redness, and pain
- Sensitivity to light
- Difficulty taking a deep breath (because expanding the chest is difficult and painful)
- Heart failure
- Pain and stiffness. Constant pain and stiffness in the low back, buttocks, and hips continue for more than three months. Back pain from ankylosing spondylitis is inflammatory in nature
- The stiffness is often worst in the morning and after you have been inactive for a while
- Bone fusion results in a rigid spine. These changes may be mild or severe and may lead to a stooped-over posture
- Pain in ligaments and tendons.

- Stiffness and pain in the morning affect the sacroiliac joint area and spine.
- Aching in the lower back can disrupt sleep.
- Pain radiating down the legs and into the groin.
- Pain is worse during and after rest e.g. in the mornings.
- Exercise eases pain and stiffness.
- Aches and pains in the buttocks, neck, shoulders, hips, and upper back.
- Symptoms may flare up and then disappear.
- Severe cases may cause feelings of illness, weight loss, and fatigue.
- Back pain relieved by movement and exercise
- Difficulty bending the spine
- Pain in the hips and difficulty walking
- Pain in the heels and soles of the feet
- Bent-over posture
- Straightening of the normal curvature of the spine
- Fever
- Loss of appetite, weight loss
- Fatigue decreased energy
- Eye swelling, redness, and pain
- Sensitivity to light
- Difficulty taking a deep breath (because expanding the chest is difficult and painful)
Diagnosis of Ankylosing Spondylitis
To diagnose ankylosing spondylitis, your doctor will ask you about your medical history and perform a physical exam. Your doctor may order imaging studies and lab tests to help confirm a diagnosis.
Medical and Family History
Your doctor may ask about your medical and family history, including questions such as:
- How long have you had pain?
- Where is your pain?
- What makes the pain better or worse?
- Does anyone in your family have a history of back pain, joint pain, or arthritis?
Physical Exam
A physical exam may include:
- Examine your joints, including your spine, pelvis, heels, and chest.
- Watching how you move and bend in different directions, checking for flexibility.
- Asking you to breathe deeply to check for rib stiffness and inflammation.

Early diagnosis of AS is important if the fusion of the joints and permanent stiffening of the spine is to be avoided. It can be difficult to diagnose in the early stages as symptoms may be attributed to more common causes of back pain. A doctor will evaluate the following when diagnosing the condition:
These diagnostic criteria include:
- Inflammatory back pain
Chronic, inflammatory back pain is defined when at least four out of five of the following parameters are present: (1) Age of onset below 40 years old, (2) insidious onset, (3) improvement with exercise, (4) no improvement with rest, and (5) pain at night (with improvement upon getting up) - A full medical history, including any family history of AS
- Discussion of current symptoms including a history of back pain
- The age of the patient when the pain started
- Physical assessment
- Past history of inflammation in the joints, heels, or tendon-bone attachments
- Family history for axial spondyloarthritis
- Positive for the biomarker HLA-B27
- Good response to treatment with nonsteroidal anti-inflammatory drugs (NSAIDs)
- Signs of elevated inflammation (C-reactive protein and erythrocyte sedimentation rate)
- Manifestation of psoriasis, inflammatory bowel disease, or inflammation of the eye (uveitis)
If these criteria still do not give a compelling diagnosis magnetic resonance imaging (MRI) may be useful. MRI can show inflammation of the sacroiliac joint.
Radiographic features
- The earliest changes in the sacroiliac joints demonstrable by plain x-ray show erosions and sclerosis.
- Progression of the erosions leads to pseudo-widening of the joint space and bony ankylosis.
- X-ray spine can reveal squaring of vertebrae with spine ossification with fibrous band run longitudinally called syndesmophyte while producing bamboo spine appearance.
- A drawback of X-ray diagnosis is the signs and symptoms of AS have usually been established as long as 8–10 years prior to X-ray-evident changes occurring on a plain film X-ray, which means a delay of as long as 10 years before adequate therapies can be introduced. Options for earlier diagnosis are tomography and MRI of the sacroiliac joints, but the reliability of these tests is still unclear.
- MRI (magnetic resonance imaging)
- Blood tests – which may show the presence of the HLA-B27gene, a raised ESR (erythrocyte sedimentation rate), and a reactive protein which indicates inflammation
- Bamboo spine-Bamboo spine is a radiographic feature seen in ankylosing spondylitis that occurs as a result of vertebral body fusion. It is often accompanied by fusion of the posterior vertebral elements as well and resembles a bamboo stem…therefore the term bamboo spine.
In order for a diagnosis of AS to be made, a referral to a rheumatologist – who specializes in treating arthritis – may be recommended.
Treatment of Ankylosing Spondylitis
Non-Surgical Treatment
- Bed rest for first 24 hours. Additional bed rest will be determined by the severity of the problem. Recent medical studies indicate that staying more active is better for back disorders than prolonged bed rest.
- Use a firm mattress (place a bed board under the mattress if needed).
- Massage may help. Be sure the person is well-trained or massage could cause more harm than help.
- Wear a special back support device.
- Other options are available depending on the degree of injury, such as surgery (if disk damaged), electrical nerve stimulation, acupuncture, special shoes, etc.
- Stress reduction techniques, if needed.
- Non-Prescription Pain Relievers – Naproxen, acetaminophen, and ibuprofen each reduce inflammation and pain. Though these drugs are available over-the-counter, they are potent and taking more than the recommended dose can harm health. A doctor can help with advice about the right kind of non-prescription pain reliever to take.
- Cold and Heat – Applying a cold pack to the painful part of the back contracts inflamed muscle and relieves pain. This treatment helps a great deal when the disk has recently ruptured and swelling is at its greatest. A heating pad or warm pack helps with residual pain.
- Continued Physical Activity – Though pain or weakness seem like good reasons to rest the back, excessive bedrest worsens the symptoms of a slipped disc. Moving around too little allows muscles to grow weaker and prevents the body from healing. Periods of rest interspersed with periods of normal activity throughout the day keep the back muscles in shape.
- Prescription Remedies – If over-the-counter drugs fail to ease slipped disc pain, the doctor will turn to prescription medications. These can include narcotics, such as hydrocodone or codeine. While they can do away with pain, narcotics are very addictive and induce a mental fogginess that can itself be dangerous. More narrowly-focused medicines designed to target damaged nerves that create chronic pain may be a better choice, as they have fewer undesirable side effects. Gabapentin and Cymbalta are two drugs that act in different ways to minimize nerve pain. These drugs are less addictive than narcotics.
- Nutrition – In order to restore the disc we also are going to need to include different substances in our diet. There are a lot of supplements on the market, of course. If you wish to try them, that’s fine. I personally don’t like them. I have tried one with glucosamine and chondroitin, but I didn’t feel any different. So, if you have the opportunity to take these with the food or from more natural sources, it will be great. You can find these substances in seafood and animal cartilages and by digesting them we ensure the building blocks for the connecting tissue for our joints and spine. Also, we will need more Omega 3 fatty acids, which can be supplied from cold-pressed oils, fatty fish, flax seeds, chia, and many more. Vitamins from the B group are very beneficial for people with herniated discs and all kinds of issues with the peripheral nervous system. Vitamins B1, B6, and B12 nourish the nerves and help them recover from the disk accident. Usually, doctors prescribe them as a part of the treatment, but it is worth mentioning anyway.
- A good massage – A massage is one of the natural methods of relieving pain. Individuals who get a massage weekly for several months stand a better chance of alleviating back pain. A good massage provides a person with many health benefits that lessen back pain. A massage triggers the release of endorphins. Endorphins aid in decreasing anxiety and relieving pain. They offer a relaxation effect by softening muscles that are injured preventing cramping.
- Undertaking yoga – Yoga is an applicable strategy for keeping the level of back pain at minimal levels. Taking yoga sessions often is very effective method of dealing with back pain. With yoga, there is a high likelihood of proper body functions. The use of pain prescriptions is also diminished. Patients suffering from back pain related issues do not have to rely on these prescriptions to manage pain. Incorporating laughter in yoga is a good way of exercising. Yoga incorporates simple yet appropriate exercises that enhance the stretching of muscles. Laughter with yoga stimulates relieving of pain. It facilitates increased uptake of oxygen, little anxiety, and production of endorphins. All these variables play an essential role in diminishing back pain.
- Adjusting sleeping position – A simple sleeping mistake can immensely contribute to back pain. A poor sleeping position can cause stress and tension on the muscles contributing to back pain. Altering one’s sleeping position and adopting a style that does not exert a lot of stress on the back is a recommended tactic. Nurturing sleeping habits such as assuming a reclining position, using wedge-shaped cushions and getting adjustable beds from reputable medical institutions are easy techniques to endorse. If a reclining position does not suit an individual, the other two techniques can be embraced.
- Heat therapy – Several considerations should be observed when using heat therapy. The right temperature ought to be set so as to ensure a patient does not face risks associated with too much exposure to heat. The key objective should be to ensure enough access to heat to the muscles to yield benefits for the patient. The adoption of heat therapy for easing back pain is determined by the magnitude of pain a person is experiencing. In cases where relatively low back pain is encountered, short heat therapy sessions are recommended. On the other hand, if an individual is experiencing prolonged back pain, long heat therapy sessions are the most applicable.
- Taking hot baths – This is a form of heat therapy that aims at relieving back pain. It guarantees permeation of heat into the muscles leading to reduced pain. Many individuals opt for this method since they believe it achieves competent results. Hot baths initiate a fast process of blood supply to stiff neck and back muscles. When this happens, the muscles relax and stretch leading to decreased back pain. To avoid interference with one’s sleeping patterns, a hot bath should be taken several hours before retiring to bed.
- Aquatic therapy – This natural technique involves physical therapy in a pool. Individuals get the best out of this therapy by relying on the resistance of water. Consistency in undertaking this therapy is what ascertains getting back pain relief. Integrating aquatic therapy in an individual’s life for the better part of the week enhances the reduction of back pain quickly.
- Enlighten others – Individuals have the power to devise their own natural strategies that aid them in coping with back pain. The strategies can also be a good remedy for others going through similar circumstances. An individual can use social media platforms to equip others with important tips on how to keep back pain at bay. Further, becoming a member of associations that address back pain issues enables better communication of the knowledge gained from personal experience.
Medication
The major types of medications used to treat ankylosing spondylitis are pain-relievers and drugs aimed at stopping or slowing the progression of the disease. All of these have potentially serious side effects. Pain-relieving drugs come in two major classes:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – These drugs relieve pain and swelling. Aspirin, ibuprofen, and naproxen are examples of NSAIDs. NSAIDs including the Coxib class are the first-line drugs for ankylosing spondylitis. A recent study reported that ankylosing spondylitis is associated with the prostaglandin E receptor 4 (PTGER4) gene. This receptor is associated with bone absorption; NSAIDs inhibit prostaglandin production, thus reducing the absorption[rx]. The mainstay of therapy in all seronegative spondyloarthropathies are anti-inflammatory drugs, which include NSAIDs such as ibuprofen, phenylbutazone, diclofenac, indomethacin, naproxen and COX-2 inhibitors, which reduce inflammation and pain. Indomethacin is a drug of choice. 2012 research showed that those with AS and elevated levels of acute phase reactants seem to benefit most from continuous treatment with NSAIDs.
- Corticosteroids – These strong drugs are similar to the cortisone made by your body. They fight pain and swelling.
- Analgesics – Acetaminophen and opioid-(like) agents are often used 1) for patients who complain of pain even after administration of NSAIDs and TNF-α inhibitors or 2) when other therapeutic options are not available.
- Glucocorticoids – Although local glucocorticoid injection can be considered for skeletal muscle inflammation such as enthesitis, systematic administration of steroids is not generally recommended6)
- Antidepressants – such as tricyclics and serotonin and norepinephrine reuptake inhibitors have been commonly prescribed for chronic low back pain, but their benefit for nonspecific low back pain is unproven, according to a review of studies assessing their benefit.
- Calcium & vitamin D3 – to improve bones health and healing fracture.
- Glucosamine & Diacerein – can be used to tightening the loose tension and regenerate cartilage or inhabit the further degeneration of cartilage.
- Corticosteroid- to healing the nerve inflammation and clotted blood in the joints.
- Dietary supplement -to remove the general weakness & improved the health.
- Vitamin D – You must correct the vitamin D deficiency in your body if you are suffering from ankylosis. Bones need Vitamin D in greater amounts when they are affected by a disease.
- Muscle Relaxants – If the muscles around the slipped disc experience painful spasms, a muscle relaxant such as Valium may be useful. The drawback to drugs like these is that they do not limit their power to the affected nerve. Instead, they have a generally relaxing effect and will interfere with daily activities. Such as cyclobenzaprine (Flexeril), might be prescribed to relieve the discomfort associated with muscle spasms. However, these medicines might cause confusion in older people. Depending on the level of pain, prescription pain medicines might be used in the initial period of treatment.
- Steroids – If inflammation is severe, a doctor may also prescribe a steroid. Steroids, such as cortisone, reduce swelling quickly. A cortisone shot directly in the affected area will have an immediate effect on the displaced disc.
- Counter-irritants – such as creams or sprays applied topically stimulate the nerves in the skin to provide feelings of warmth or cold in order to dull the sensation of pain. Topical analgesics reduce inflammation and stimulate blood flow.
- Nerve Relaxant — Pregabalin or gabapentin and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include aspirin, ibuprofen, and naproxen.
- Disease-modifying antirheumatic drugs (DMARDs) – These drugs work in different ways to reduce pain and swelling in AS. Although the administration of DMARDs (e.g., sulfasalazine and methotrexate) is not recommended for axial diseases such as back pain, sulfasalazine is worth considering for treatment of peripheral arthritis [Rx]. Disease-modifying antirheumatic drugs (DMARDs) such as sulfasalazine can be used in people with peripheral arthritis. For axial involvement, the evidence does not support sulfasalazine. Other DMARDs, such as methotrexate, did not have enough evidence to prove their effectiveness. Generally, systemic corticosteroids were not used due to lack of evidence. Local injection with a corticosteroid can be used for certain people with peripheral arthritis.
- TNF-α inhibitors – In 1995, Braun and coworkers[rx] isolated TNF-α from ankylosing spondylitis patients via sacroiliac arthrocentesis. Thus, it was recognized that TNF-α is an important inflammatory mediator in this disease, which dramatically facilitated the development of biological agents.
- Infliximab (Remicade) – Infliximab is a chimeric monoclonal antibody against TNF-α and is the first developed biological agent, consisting of 75% of human and 25% of mouse sequences[ rx]. This antibody directly binds to TNF-α and neutralizes it. It is administered by intravenous injections at 5 mg/kg body weight. For the first administration, the same dose of infliximab is injected twice with an interval of 2 weeks and then the drug is administered every 6 weeks. Baraliakos et al.[Rx] reported a drug survival rate (patients who completed 8 years of treatment) of 48% and 88% of partial remission or low disease activity after 8-year follow-up. It was also reported that the potency was similar when the treatment was interrupted for 3 years and then resumed.
- Etanercept (Enbrel) – Etanercept is a soluble blocker of TNF-α. This fusion protein binds TNF-α, which hinders interactions between TNF-α and TNF-α receptor located on other cells. Etanercept is generally administered by subcutaneous injection of 25 mg twice a week [Rx]. Martĺn-Mola et al.[Rx]reported that 63% of the enrolled patients completed 5 years of etanercept administration without any serious complications, while Baraliakos reported a drug survival rate of 62%, partial remission in 31% of patients, and complete remission in 44% of patients in a 7-year follow-up study. Similar to infliximab, etanercept was effective when the medication was interrupted and then resumed; the drug survival rate was slightly higher in the etanercept group than in the infliximab group.
- Adalimumab (Humira) – Like infliximab, adalimumab is a monoclonal antibody against TNF-α but its sequence is 100% human. Adalimumab is administered by subcutaneous injections of 40 mg once per 2 weeks. Sieper et al.[Rx] reported a drug survival rate of 65%, partial remission according to Ankylosing Spondylitis Disease Activity Score (ASDAS) in 51% of patients, and ASDAS inactive disease in 61% of patients in a 5-years follow-up study. Similar to the long-term follow-up results for infliximab, favorable outcomes of long-term follow-up were demonstrated with remission achieved after 12 weeks of administration.
- Anti-tumor necrosis factor therapy —A group of medicines known as anti-tumor necrosis factor agents (anti-TNF agents or TNF inhibitors) are often effective in the treatment of AS. Examples of anti-TNF medications include infliximab, etanercept, adalimumab, certolizumab pegol, and golimumab. People who do not respond to one anti-TNF treatment may respond to another. Improvement in symptoms is common and may occur within a few weeks of starting the drugs.
- Who should use anti-TNF therapy? – Not every patient with AS needs anti-TNF therapy. In general, people with the active disease in the spine who have not responded fully to NSAIDs may be candidates (see ‘How do I know how active my ankylosing spondylitis is?’ above). Your clinician may also recommend a glucocorticoid (cortisone-like drug) injection into painful or swollen joints before starting an anti-TNF drug if these areas continue to bother you despite using NSAIDs (see ‘Glucocorticoids (steroids)’ below). The decision to use anti-TNF therapy depends upon several factors that should be discussed with your clinician.
- Secukinumab — Secukinumab (brand name: Cosentyx) may be an alternative treatment option for some people who do not respond adequately to anti-TNF therapy.
- Glucocorticoids (steroids) — Some clinicians may also recommend a glucocorticoid injection into particularly painful or swollen joints, especially if only one or two areas are causing the most pain. In some cases, a glucocorticoid injection into the sacroiliac joint may help provide relief in patients who have sacroiliac pain that has not responded to other therapies.
- Bisphosphonates – Oral bisphosphonates are commonly used for fracture prevention in ankylosing spondylitis. Bisphosphonates also have an anti-inflammatory action and may have an effect on disease activity. Intravenous pulses of the bisphosphonate pamidronate have been investigated in several studies and have produced significant clinical improvements in some but not all studies.[rx]
- Omega-3 fats and inflammation – Foods that contain omega-3 fats have been found to help reduce the inflammation associated with some forms of arthritis. These effects are modest compared with medication. Omega-3 fats have few side effects and may have other health benefits, such as reduced heart disease. Foods rich in omega-3 fats include
- fish – the oily fish such as salmon and sardines have greater amounts of omega-3 fats
- linseeds and linseed (flaxseed) oil
- canola (rapeseed) oil
- walnuts
- foods fortified with omega-3, such as margarine and eggs
- some fish oil supplements.
- Potassium Rich Foods
Potassium is known to decrease inflammation if it is present in the body in adequate amounts. Foods that contain potassium in high amounts are bananas, almonds, apricots, and broccoli.
Other Medications to Stop Inflammation and Save Your Joints: Biological Drugs
If NSAIDs or DMARDs do not control your AS, your doctor may prescribe drugs called biologics. These drugs aim to address the problems with your immune system. They target your body’s production of specific proteins that cause inflammation.
Biologic drugs slow your immune system to help ease AS symptoms (pain, swelling, tenderness, and stiffness) as well as inflammation. These drugs may also help protect your joints from damage.
Dietary & Molecular Supplements
-
Omega-3 Fish Oil
-
Dosage: 2–3 g/day EPA/DHA
-
Function: Anti-inflammatory by shifting eicosanoid balance
-
Mechanism: Reduces pro-inflammatory cytokine synthesis [rx].
-
-
Vitamin D₃
-
Dosage: 1,000–2,000 IU/day
-
Function: Bone health and immune modulation
-
Mechanism: Regulates T-cell responses and promotes calcium absorption [rx].
-
-
Calcium Citrate
-
Dosage: 500–1,000 mg/day
-
Function: Prevents osteoporosis from chronic inflammation/steroids
-
Mechanism: Provides substrate for bone mineralization [rx].
-
-
Curcumin (Turmeric Extract)
-
Dosage: 500 mg BID standardized to 95% curcuminoids
-
Function: Natural anti-inflammatory and antioxidant
-
Mechanism: Inhibits NF-κB and COX-2 pathways [rx].
-
-
Boswellia Serrata
-
Dosage: 300 mg three times daily
-
Function: Reduces joint inflammation
-
Mechanism: Inhibits 5-lipoxygenase and leukotriene synthesis [rx].
-
-
Probiotic Blend
-
Dosage: ≥10⁹ CFU/day multispecies
-
Function: Supports gut barrier and immune balance
-
Mechanism: Modulates gut microbiota and reduces systemic inflammation [rx].
-
-
Resveratrol
-
Dosage: 150–500 mg/day
-
Function: Antioxidant and anti-inflammatory
-
Mechanism: Activates SIRT1 and inhibits TNF-α production [rx].
-
-
Vitamin K₂
-
Dosage: 90–120 mcg/day
-
Function: Improves bone mineralization
-
Mechanism: Activates osteocalcin, aiding calcium deposition in bone [rx].
-
-
Magnesium Citrate
-
Dosage: 200–400 mg/day
-
Function: Muscle relaxation, bone health
-
Mechanism: Cofactor for collagen synthesis and neuromuscular function [rx].
-
-
Green Tea Extract (EGCG)
-
Dosage: 300–500 mg/day
-
Function: Anti-oxidative, may reduce inflammation
-
Mechanism: Inhibits pro-inflammatory cytokines and MMPs [rx].
-
Advanced & Regenerative Drug Therapies
-
Alendronate (Bisphosphonate)
-
Dosage: 70 mg once weekly
-
Function: Prevents bone loss
-
Mechanism: Inhibits osteoclast-mediated bone resorption [rx].
-
-
Zoledronic Acid (Bisphosphonate)
-
Dosage: 5 mg IV once yearly
-
Function: Strong anti-resorptive for severe osteoporosis
-
Mechanism: Binds hydroxyapatite, induces osteoclast apoptosis [rx].
-
-
Hyaluronic Acid Injection (Viscosupplementation)
-
Dosage: 20 mg intra-articular per injection, weekly×3
-
Function: Improves joint lubrication (primarily peripheral joints)
-
Mechanism: Restores synovial fluid viscosity and cushions load [rx].
-
-
Platelet-Rich Plasma (PRP) (Regenerative)
-
Dosage: 3–5 mL intra-enthesis injection monthly×2–3
-
Function: Enhances tissue repair at entheses
-
Mechanism: Delivers concentrated growth factors to stimulate healing [rx].
-
-
Mesenchymal Stem Cell Therapy
-
Dosage: 1–10 × 10⁶ cells/kg IV or local injection
-
Function: Potentially regenerates damaged tissues
-
Mechanism: Differentiates into musculoskeletal cells and modulates immune response [rx].
-
-
Denosumab (RANKL inhibitor)
-
Dosage: 60 mg subcutaneously every 6 months
-
Function: Reduces bone resorption
-
Mechanism: Monoclonal antibody binds RANKL, preventing osteoclast activation [rx].
-
-
Teriparatide (PTH analog)
-
Dosage: 20 mcg subcutaneously daily
-
Function: Anabolic bone formation
-
Mechanism: Stimulates osteoblast activity and bone matrix synthesis [rx].
-
-
IL-17 Inhibitors (e.g., Secukinumab)
-
Dosage: 150 mg SC weekly×5 then monthly
-
Function: Reduces spinal inflammation
-
Mechanism: Neutralizes IL-17A cytokine, blocking inflammatory cascade [rx].
-
-
TNF Inhibitors (e.g., Adalimumab)
-
Dosage: 40 mg SC every other week
-
Function: Controls systemic inflammation
-
Mechanism: Binds TNF-α, preventing receptor activation [rx].
-
-
Platelet-Derived Growth Factor (PDGF)
-
Dosage: Experimental – dose varies by protocol
-
Function: Stimulates tissue regeneration
-
Mechanism: Promotes cell proliferation and angiogenesis [rx].
-
Biologic drugs used to treat AS include:
- Adalimumab
- Certolizumab
- Etanercept
- Etanercept
- Golimumab
- Infliximab
- Infliximab
- Secukinimab
Biologic drugs used to treat AS include:
- Adalimumab
- Certolizumab
- Etanercept
- Etanercept
- Golimumab
- Infliximab
- Infliximab
- Secukinimab
Surgical Options
-
Total Hip Arthroplasty
-
Procedure: Replacement of acetabulum and femoral head
-
Benefits: Relieves severe hip pain and restores mobility [rx].
-
-
Corrective Spinal Osteotomy
-
Procedure: Wedge resection of vertebra to correct kyphosis
-
Benefits: Improves upright posture and horizontal gaze [rx].
-
-
Spinal Fusion
-
Procedure: Instrumented fusion of mobile vertebral segments
-
Benefits: Stabilizes spine, prevents deformity progression [rx].
-
-
Vertebroplasty/Kyphoplasty
-
Procedure: Injection of bone cement into compressed vertebrae
-
Benefits: Reduces fracture pain and restores vertebral height [rx].
-
-
Facet Joint Replacement
-
Procedure: Prosthetic facet implantation
-
Benefits: Preserves motion while relieving pain [rx].
-
-
Enthesectomy
-
Procedure: Surgical removal of inflamed entheses
-
Benefits: Alleviates localized tendon–bone pain [rx].
-
-
Arthroscopic Synovectomy
-
Procedure: Minimally invasive removal of inflamed joint lining
-
Benefits: Decreases pain in peripheral joints [rx].
-
-
Vertebral Column Resection
-
Procedure: Removal of entire vertebral segment for severe deformity
-
Benefits: Enables correction of rigid kyphoscoliosis [rx].
-
-
Spinal Decompression (Laminectomy)
-
Procedure: Removal of lamina to relieve nerve compression
-
Benefits: Alleviates neurological symptoms from stenosis [rx].
-
-
Interspinous Process Device Insertion
-
Procedure: Implant between spinous processes to limit extension
-
Benefits: Reduces pain from facet overload while preserving some motion [rx].
-
Clinical Trials
Doctors and scientists are constantly coming up with new ways to treat diseases, and they always need patients to test the efficacy of a proposed intervention. Below, you will find a current list of trials for ankylosing spondylitis and related conditions, as well as a link to enroll. You should speak with your doctor to decide if enrolling in a clinical trial is a good option for you.
Physical therapy involves three main components: education, passive treatments, and active treatments. A physical therapist uses passive treatments to relax you and your body and to decrease acute pain or inflammation. They’re called passive because you don’t have to actively participate. If you’re experiencing acute pain, you’ll most likely start with passive treatments as your body heals and/or adjusts to the pain. However, the goal of physical therapy is to get into active treatments. These are therapeutic exercises that strengthen your body so that your spine has better support.
Passive Treatments for Ankylosing Spondylitis
Your physical therapist may give you passive treatments such as:
Deep Tissue Massage – This technique targets spasms and chronic muscle tension that perhaps builds up through daily life stress. You could also have spasms or muscle tension because of strains or sprains. The therapist uses direct pressure and friction to try to release the tension in your soft tissues (ligaments, tendons, muscles).
Hot and Cold Therapies – Your physical therapist will alternate between hot and cold therapies. By using heat, the physical therapist seeks to get more blood to the target area because an increased blood flow brings more oxygen and nutrients to that area. Blood is also needed to remove waste byproducts created by muscle spasms, and it also helps to heal. Cold therapy, also called cryotherapy, slows circulation, helping to reduce inflammation, muscle spasms, and pain. You may have a cold pack placed upon the target area, or even be given an ice massage. Another cryotherapy option is a spray called fluoromethane that cools the tissues. After cold therapy, your therapist may work with you to stretch the affected muscles.
Electrical stimulation – This can be performed within the clinic and if extremely successful, a TENS unit can be issued to a patient for home use. E-stim stimulates your muscles through variable (but safe) intensities of electrical current. It helps to reduce muscle spasms, and it may increase your body’s production of endorphins, your natural pain killers. It may also drive out inflammation, bring in healing properties, relax, and re-educate the muscles involved. The e-stim unit in the clinic is of a professional standard; the equipment is relatively large. However, a smaller machine for at “at home” use is also available. Electrical stimulation is a helpful therapy.
Yoga – Yoga is a great natural pain reliever for ankylosing spondylitis,” Ostrowski says. “You need to start with very basic poses and be patient, but if you work with an instructor who can modify the yoga positions for you, you can really benefit from this form of exercise.” A review of studies published in January 2016 in the Journal of Orthopedics & Rheumatology examined the impact of yoga on low back pain and found that it was safe and can help reduce both disability and pain.
Who Treats Ankylosing Spondylitis?
Diagnosing and treating ankylosing spondylitis may require a team of health care professionals. These may include:
- Rheumatologists, who specialize in arthritis and other diseases of the bones, joints, and muscles.
- Dermatologists, who specialize in conditions of the skin, hair, and nails.
- Gastroenterologists, who specialize in conditions of the digestive system.
- Mental health professionals, who help people cope with difficulties in the home and workplace that may result from their medical conditions.
- Nurse educators, who specialize in helping people understand their overall condition and set up their treatment plans.
- Occupational therapists, who teach ways to protect joints, minimize pain, perform activities of daily living, and conserve energy.
- Ophthalmologists, who specialize in conditions of the eye.
- Orthopaedic surgeons, who specialize in treatment and surgery for bone and joint diseases.
- Physiatrists (physical, medicine, and rehabilitation specialists), who supervise exercise programs.
- Physical therapists, who help improve joint function.
- Primary care doctors, such as a family physicians or internal medicine specialists, who coordinate care between the different health providers and treats other problems as they arise.
- Psychologists or social workers, who help with psychosocial challenges caused by medical conditions.
Home Remedies For Ankylosing Spondylitis
- Use Ginger, Black Pepper or any good digestive with your meals. It will help detoxify your body.
- 1 tablespoonful of Turmeric should be consumed once every day, after boiling it in milk for half an hour.
- Constipation must be avoided at all costs. Constipation may increase pain in Ankylosing spondylitis.
- Herbs have divine healing powers and they have the ability to cure any disease of the root. They were gifted to us by God when he created life. So believe in God if you want to get rid of your problems!
- Ayurvedic herbs are unique natural remedies for Ankylosing spondylitis. Ayurvedic principles are different in many ways From modern medicine for example – Drinking water From a copper pan after keeping it overnight is also very useful in Rheumatoid arthritis and Ankylosing spondylitis.
- Consuming castor oil at night with milk or alone is a very useful herbal remedy for arthritis, especially rheumatoid arthritis and ankylosing spondylitis.
- Improve your nutrition as the first step. It plays an important role to fight diseases. When nothing works, nutrition works a lot !
- Use herbal juices like Aloe vera juice (Kumari Saar) and Amla Juice ( Amla Saar) in routine. Amla is the richest source of natural Vitamin C. Vitamin C improves the natural immunity of the body. 100 gm of Amla juice contains 30 times more vitamin C than 100 gm of oranges.

Homeopathic treatment for Ankylosing Spondylitis
Homeopathy treats the person as a whole. A Remedy is selected after full individualizing examination and case analysis which includes a medical history of the patient, physical and mental constitution etc.
- Phosphorus – The rigidity of nape of the neck. Pressure on shoulders. Swelling of the neck. Engorgement of axillary glands and of those of nape of the neck and of the neck. Paralyzes sensation in the upper sacrum and lower lumbar vertebrae. Contusive pain in loins and back (as if the back were broken), especially after having been seated a long time Sensitiveness of spinous processes of dorsal vertebrae to pressure.
- Silicea – The stiffness of nape, with a headache. Swelling of glands of nape, in the neck, and under the axillae (with suppuration), sometimes with indurations…Stitches between the hips.Coccyx painful, as after a long carriage ride.- Stinging in os coccyx on rising, painful to pressure. -Scabby elevation on the coccyx, above fissure of nates- Inflammatory abscess in the lumbar region (on the psoas muscle).- Weakness and paralytic stiffness in back, loins, and nape.
- Aurum Metallicum – Serious or advanced rheumatism with marked stiffness. Rheumatism with stiffness or spasms of the chest wall. Severe spasm or tearing pains. Pains also described as “paralytic.” An important remedy in ankylosing spondylitis. Wandering arthritis; moving spot to spot from one week to next. Worse: Night. Morning in bed. Hip pain worse rising from a seat or from walking.
- Sulfur – The stiffness of the neck, in nape, with a paralytic, sprained pain. A child cannot hold head up neck muscles so weak. Tetters on nape. Swelling and inflammation of glands of nape and of the neck. Swelling and suppuration of axillary glands. Cracking in vertebrae of the neck, especially on bending backward.
- Maintain a healthy weight – If you are overweight or obese, the extra load on your joints may be exacerbating your symptoms, especially if your affected joints include those of the hip, knee or spine. There is also a clear link between being overweight and an increased risk of developing osteoarthritis.
Early studies of anti-tumor necrosis factor (TNF)-alpha therapy over 2 years showed no structural progression of ankylosing spondylitis (AS) on radiography. However, more recent data indicated that a strong relationship exists between disease activity and structural progression. If you have the inactive disease, it’s a relatively flat line, but if you have very high disease activity, there’s a very striking relationship between disease activity and the Ankylosing Spondylitis Disease Activity Score,” said Dr. Elewaut of the department of rheumatology at Ghent (Belgium) University Hospital. “We were missing something in the early clinical studies of an anti-TNF alpha agent, and there are a few explanations as to why.
PHYSIOTHERAPY TREATMENTS
- Regular physiotherapy is very essential in the management of a patient of AS and only a physiotherapist is the person who can help the patient to fight the disease.
Aims of physiotherapy management in ankylosing spondylitis treatment:-
- Relieve pain.
- Maintain the mobility of joints affected like the spine, hip, thorax, shoulder, etc.
- Prevent and correct the deformity.
- Increase chest expansion and vital capacity.
- Attention to posture.
- To maintain and improve physical endurance.
- Advice to patient.
General instruction to patients:-
- Make the exercise part of your daily routine.
- Try to do a complete set of exercises at least twice daily at a time convenient to you.
- Heat and cold application any precede exercise to enhance relaxation and decrease pain.
- Perform only those exercises given to you by your physiotherapist.
- Perform exercises on a firm surface.
- Exercise slowly with a smooth motion, do not rush.
- Avoid holding your breath while exercising.
- Modify the exercise regime during an acute attack and contact your physical therapist if you have any complaints or problems with the exercises.
Pain Relief:-
Pain and muscle spasms are treated by the following modalities and relaxation is advised-
- Infrared.
- Hot packs.
- Cryotherapy.
- Steambath.
- Hydrotherapy.
Exercises for mobilization of joints:-
- Maintaining the mobility of joints, by giving mobility exercises to particular joints, which are affected like, the spine, hip, shoulder, the thoracic cage is essential in Ankylosing Spondylitis Treatment.
- Maintenance of mobility is very important and the basic aim is that all the joints are moved to their maximum limit and by this, we can delay the process of ankylosis.
Prevent and correct the deformity by giving attention to posture:-
- The spondylitis patient should always be conscious of his posture while sitting, standing and walking patient should maintain an erect posture during these activities. This helps to prevent and correct deformity and thus help in Ankylosing Spondylitis Treatment.
- Sleeping should occur in the prone position or supine on a firm mattress with a thin or no pillow by this, the spine remains in the extended position and not inflected.
- The design of chairs is important particularly for those who spend most of their working hours sitting at a desk. A low armchair should be avoided, an upright chair with some cushioning to support the lower lumbar spine is better.
- Adjust the height of the working table and ensure that the patient does not stop on that.
- Avoidance of prolonged immobilization or bed rest, because of this, the spinal extensors become weak and by this, the extended position of the spine is not retained.
Increase chest expansion and vital capacity:-
To increase chest expansion and vital capacity, breathing exercises are required. Breathing exercises that are used in Ankylosing Spondylitis Treatment:
- Apical breathing exercises.
- Diaphragmatic breathing exercises.
- Lateral costal breathing exercises.
- Deep breathing exercises are encouraged. Ballooning exercise is also very useful in Ankylosing Spondylitis Treatment. They increase the vital capacity of the lung. Thoracic mobility exercises.
Group Therapy Classes:-
- The patient can give support to the other member of the class that is another patient.
- Shared problems provide a good medium for patient education and the latest information about the disease process.
- Development of competitiveness and motivational aspects.
- Improvement in physical fitness
Exercises
Forward and Backward Tilt
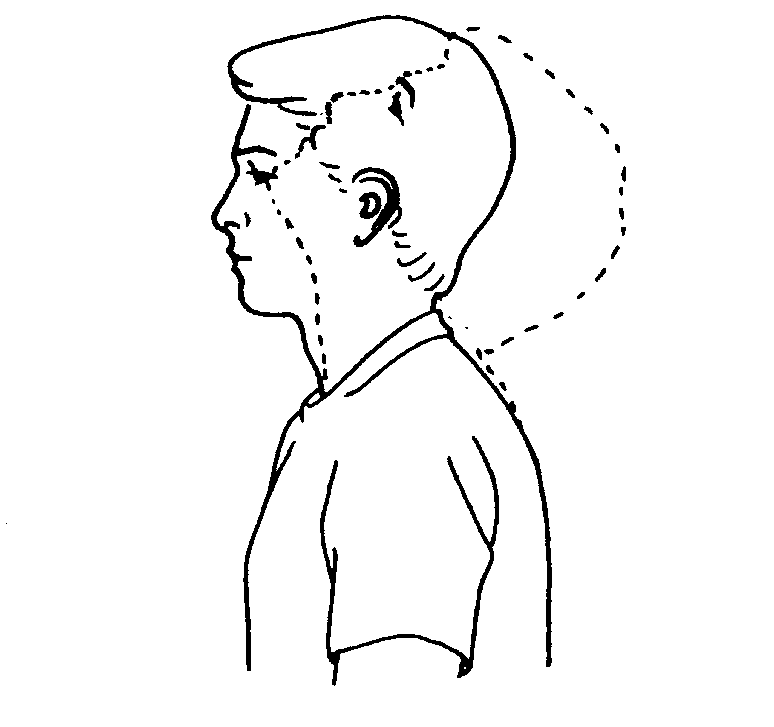
This can be done while you’re seated or on your feet. Keep your moves slow and smooth.
Start with your head squarely over your shoulders and your back straight.
Lower your chin toward your chest and hold for 15-30 seconds. Relax, and slowly lift your head back up.
Tilt your chin up toward the ceiling and bring the base of your skull toward your back. Hold for 10 seconds, then return to the start position.
Repeat the set several times. Do it every day.
Side Tilt
Do this while standing, with your feet hip-width apart and arms down by your sides.
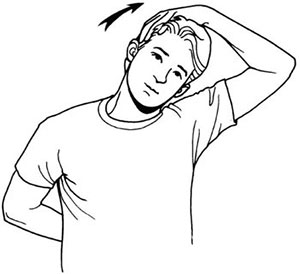
Gently tilt your head toward your right shoulder and try to touch it with your ear. Stop when you feel the stretch. Don’t raise your shoulder.
Hold the stretch for 5-10 seconds, then return to the start position.
Repeat on your left side. You can do several sets and work your way up to 10 repetitions.
For extra stretch, put the hand on the same side of your tilted head on top of your head, and press lightly with your fingertips.
Above Head Stretch :
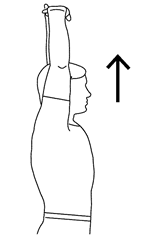
Seated or standing, interlock your fingers, bend your elbows and raise your arms above your head.
Gently squeeze your shoulder blades together and move your elbows and hands backward.
Vary the height of your hands to emphasize shoulders and/or chest (hands behind head, hands on top of head, hand a few inches above head).
Anterior deltoid stretch

You can perform the anterior deltoid stretch standing or seated — just keep your feet firmly planted and your back straight.
With your spine straight, reach your arms behind you and interlace your fingers. If you can’t interlace your fingers, grab opposite wrists or elbows or try grasping a small towel with each hand. Roll your shoulders back to sit up tall, allowing your chest to open up, and gently squeeze your shoulder blades together. Moving slowly, carefully straighten your arms. Next, gradually begin to raise your arms behind you, moving only as far as you can maintain an upright posture. Stop once you feel a stretch. Pause, breathing deeply into the stretch. Repeat 2 to 3 times, as needed.
Posterior deltoid stretch
To perform the posterior deltoid stretch, start in a standing or seated position with your spine straight.
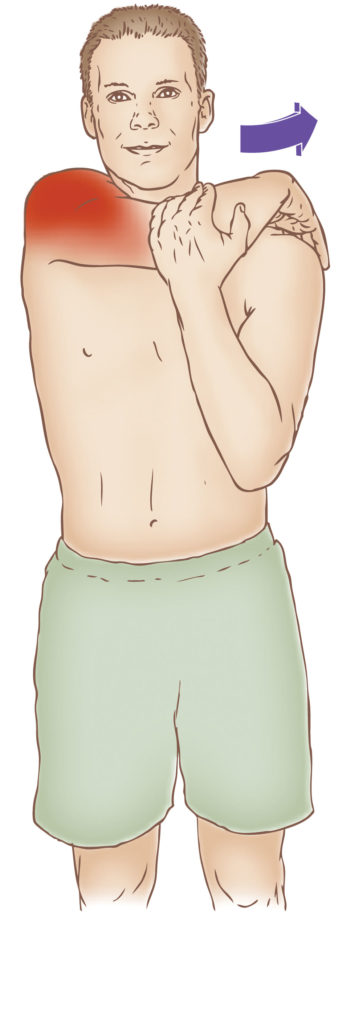
Relax your shoulders. Reach one arm across your body, using your other arm or wrist to hold it gently by your upper arm. Slowly begin to pull your arm toward your chest, as far as possible, allowing the stretch to reach deep into the back of your shoulder. Pause, breathing deeply into the stretch. Hold for at least 30 seconds. Release and repeat with the other arm.
Overhead triceps stretch
You can do the overhead triceps stretch while standing or sitting.
To do this:

Lift your shoulders up toward your ears and then draw them down and back.
Extend your right arm to the ceiling, then bend at the elbow to bring the right palm toward the center of your back, resting your middle finger along your spine. Use your left hand to gently push your elbow in toward the center and down.
Hold this stretch 30 seconds for three to four repetitions on each side.
Seated Lateral Trunk Stretch
While in a seated position, raise one arm over your head. Place your other hand on your thigh for support.
Slowly bend to the opposite side until you feel a comfortable stretch along the side of your trunk. Hold the stretch for 15-20 seconds, then repeat 3-5 times on each side.
Prayer Stretch
Tucking legs underneath, sit back on the heels and bend forward at the waist, extending arms out over the head onto the floor in front. (The goal is to get length in the lower back muscle). Hold for 30-60 seconds and sit back up. Repeat 3-5 times.

Aerobics Exercise :
Marching in Place :

Stand, holding onto a supportive railing or the back of a chair or bench. Hold on with both hands if you feel unsteady. Alternate lifting knees up and down as if marching in place. March in place for 3 to 5 minutes. Gradually try to lift knees higher and/or march faster toward the end.
Tap up and tap down :
Stand in front of a box or other stable platform. Place one foot on the top of the platform. The ball of your foot will be touching the box or ball. Your other foot will remain planted on the ground, and arms at your sides. To start the exercise, push off from the planted foot to bring it up and onto the platform while simultaneously bringing the lead foot back to the floor. This change will happen mid-air. Land with the lead foot on the ground and the edge of the planted foot on the platform. Continue alternating feet, without stopping, for the desired time. The change will be quick, and it will feel like running on stairs. Perform standing toe taps for 30 to 60 seconds. Rest for 15 to 30 seconds and repeat for 2 to 3 sets.
To make this move more challenging, increase the speed of the toe taps and pump your arms.
To decrease some of the difficulty, you can also perform toe taps on the ground doing the same movements without a raised step.
Basic :
It can be done with the R or L foot leading. Step up with one foot and then down (different instructors may use different arm movements with this move).
Example: Basic Right – step up with the R foot first followed by the L foot. Step down with the R foot first followed by the L foot.
V-Step :
The V-Step forms the letter V with the feet and can be done on the aerobic bench or on the floor. You do the movement in four counts.
HOW TO DO IT:
Stand with your feet hip-distance apart. Step forward with the right foot as wide as possible, then step forward and out with the left foot as wide as possible. Step right foot and left foot back to hip-distance, one count at a time. Repeat for the designated number of reps.
Turn-step
Do the turnstep on an aerobic bench, also in four counts. Start the move facing the step sideways.
HOW TO DO IT:
Leading with the right foot, step up on right corner of the bench sideways. Then bring the left foot up onto the bench to the left corner as you turn. Step off the bench with the right foot, bring the left foot down next to the right foot. Repeat with the left side for as many repetations as desired.
Grapevine
The Grapevine is a popular move in floor-based aerobics classes. It’s performed in an eight-count pattern as you basically criss-cross step across the floor.

HOW TO DO IT:
Start with your feet hip-distance apart. Step to the side with the right foot. Step the left foot behind and past the right foot, then step to the side with the right foot. Finally, bring the left foot next to the right foot. Then step to the side with the left foot, bring the right foot behind and past the left foot. Repeat, leading with the left foot and traveling to the left. You may see instructors add turns and bringing the knees up to make the move more challenging.
Living With Ankylosing Spondylitis
Research shows that people who take part in their own care report less pain and make fewer doctor visits. They also enjoy a better quality of life.
Self-care can help you play a role in managing your ankylosing spondylitis and improving your health. You can:
- Learn about the disease and its treatments.
- Communicate well with your health care team so you can have more control over your disease.
- Reach out for support to help cope with the physical, emotional, and mental effects of ankylosing spondylitis.
Participating in your care can help build confidence in your ability to perform day-to-day activities, allowing you to lead a full, active, and independent life.
The following lifestyle changes and activities can help improve your ability to function on your own and maintain a positive outlook.
- Exercise. Exercise is important for maintaining healthy and strong muscles, preserving joint mobility, and maintaining flexibility. In addition to an exercise program, your doctor may recommend low-impact exercises, such as water exercise programs. Talk to your health care providers before beginning any exercise program. Exercise can help:
- Improve your sleep.
- Decrease pain.
- Keep a positive attitude.
- Maintain a healthy weight.
- Posture. Another important thing you can do for yourself is to practice good posture. Your physical therapist and doctors can give you tips and exercises to help maintain and improve your posture. Practicing good posture can help you avoid some of the complications that can occur with ankylosing spondylitis.
- Support or assistive devices. Using a cane or walker can help you move around safely, provide stability, and lower pain. If you have trouble bending due to spine stiffness, try using a device to grab or pick up items.
- Monitoring of symptoms. It is important to monitor your symptoms for any changes or the development of new symptoms. Understanding your symptoms and how they may change can help you and your doctor manages your pain when you have a flare.
- Stress management. The emotions you may feel because of your disease, along with any pain, physical limitations, and the unpredictable nature of flares can increase your stress level. Although there is no evidence that stress plays a role in your disease, it can make living with ankylosing spondylitis more difficult. Ways to cope with stress can include:
- Use relaxation techniques such as deep breathing, meditating, or listening to quiet sounds or music.
- Try movement exercise programs, such as yoga and tai chi.
- Mental health management. If you feel alone, anxious, or depressed about having ankylosing spondylitis, talk to your doctor or mental health professional. Keep the lines of communication open. Talk to family and friends about your disease. You may find it helpful to join an online or community support group.
- Healthy diet. A healthy diet is good for everyone, and it may be very helpful if you have ankylosing spondylitis. There is no specific diet for people with ankylosing spondylitis, but keeping a healthy weight is important. It reduces stress on painful joints.
- Smoking. If you smoke, quit. Ankylosing spondylitis is more severe in people who smoke, and smoking blunts the effect of treatment. In addition, if you have ankylosing spondylitis in the chest or ribs, smoking can compromise your lung function even more. Smoking is also a risk factor for the progression of the disease.
References











