Osteoarthritis (OA), which is also known as osteoarthrosis or degenerative joint disease (DJD), is a progressive disorder of the joints caused by gradual loss of cartilage and resulting in the development of bony spurs and cysts at the margins of the joints. The name osteoarthritis comes from three Greek words meaning bone, joint, and inflammation.
Osteoarthritis is a multifactorial process in which mechanical factors have a central role and is characterized by changes in the structure and function of the whole joint. Rx There is no cure, and current therapeutic strategies are primarily aimed at reducing pain and improving joint function. We searched Medline for relevant articles (1966 to January 2006) and the Cochrane library (to the first quarter of 2006) and consulted experts in rheumatology to produce a narrative review with an update on management for primary care doctors. We concentrated on osteoarthritis of the knee as this is associated with the greatest public health burden.
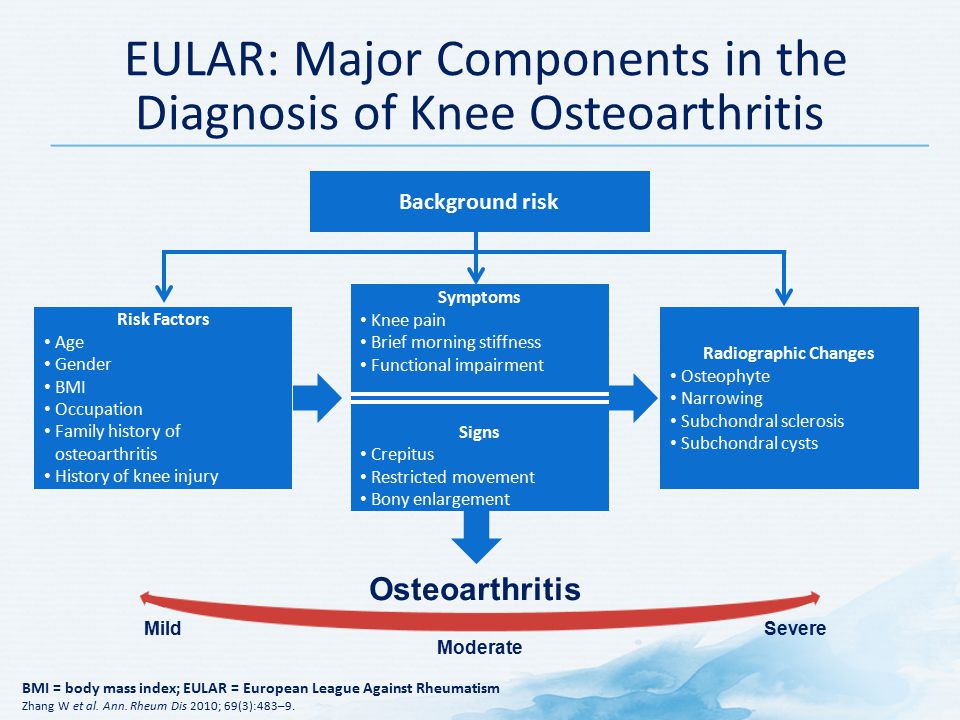
Osteoarthritis (OA) is a common disease of an aged population and one of the leading causes of disability. The incidence of knee OA is rising by increasing the average age of the general population. Age, weight, and trauma to joints due to repetitive movements, in particular, squatting and kneeling are common risk factors for knee OA. Several factors including cytokines, leptin, and mechanical forces are pathogenic factors of knee OA. In patients with knee pain attribution of pain to knee OA should be considered with caution. Since a proportion of knee OA is asymptomatic and in a number of patients identification of knee OA is not possible due to the low sensitivity of radiographic examination.
Pathophysiology
Cartilage
- Type II collagen most important structural protein
- Chondrocytes regulate cartilage architecture, biomechanical composition
- When activated, chondrocytes release multiple inflammatory cytokines including TNF-alpha, IL-6, IL-1, metalloproteinases, a disintegrin
- In osteoarthritis, the immune system is activated by damage-associated molecules including glycosaminoglycans, hyaluronan
- Calcium pyrophosphate and sodium urate crystals also bind to chondrocytes
- It is unclear if chondrocytes are primarily activated from cartilage degradation or secondarily from other joint structures
Subchondral Bone
- Forms anchor between articular cartilage and trabecular bone
- Osteoblasts respond to mechanical stimulation similar to chondrocytes
- Pronounced changes occur in subchondral bone in osteoarthritis
- Radiographs evidence includes osteophytes, subchondral cysts, subchondral sclerosis
- MRI can also demonstrate microfractures at different stages of healing
- One study suggested that subchondral degeneration may precede cartilage degeneration
- Subchondral bone is highly innervated and contributes to pain generation
Synovium
- Inflammation of the synovium, termed synovitis, is a commonly seen in osteoarthritis
- Synoviocytes are noted to proliferate under arthritic stress, producing hyaluronic acid and lubricin
- In physiologically normal patients, these proteins provide lubrication and reduce stress load
- In patients with osteoarthritis, they demonstrate reduced lubrication and stress reduction
- Synoviocytes also release inflammatory markers similar to osteoblasts and chondroblasts
Systemic Inflammation
- In general, osteoarthritis is considered a localized pathologic state and not a systemic illness
- 2013 systematic review: C-reactive associated with symptoms but not radiographic findings
Osteoarthritis formation
When your knee has osteoarthritis its surfaces become damaged and it doesn’t move as well as it should do. The following happens:
- The cartilage becomes rough and thin – this can happen over the main surface of your knee joint and in the cartilage underneath your kneecap.
- The bone underneath the cartilage reacts by growing thicker and becoming broader.
- All the tissues in your joint become more active than normal as if your body is trying to repair the damage.
- The bone at the edge of your joint grows outwards, forming bony spurs called osteophytes.
- The synovium may swell and produce extra fluid, causing the joint to swell – this is called an effusion or sometimes water on the knee.
- The capsule and ligaments slowly thicken and contract.
These changes in and around your joint are partly the result of the inflammatory process and partly an attempt by your body to repair the damage. In many cases, your body’s repairs are quite successful and the changes inside your joint won’t cause much pain or, if there is the pain, it’ll be mild and may come and go.
However, in other cases, the repair doesn’t work as well and your knee is damaged. This leads to instability and more weight being put onto other parts of the joint. This can cause symptoms to become gradually worse and more persistent over time.
How does a normal knee work?
- Your knee joint is where your thigh bone (femur) and your shin bone (tibia) meet. It allows the bones to move freely but within limits.
- Your knee is the largest joint in the body and also one of the most complicated. It needs to be strong enough to take our weight and must lock into position so we can stand upright. But it also has to act as a hinge so we can walk, and it must withstand extreme stresses, twists, and turns, such as when we run or play sports.
Causes of Osteoarthritis (OA) of Knee
Articular cartilage increased the water content
- Alterations in proteoglycans eventual decrease in the number of proteoglycans
- Collagen abnormalities organization and orientation are lost
- Binding of proteoglycans to hyaluronic acid
Synovium and capsule
An early phase of OA
- Mild inflammatory changes in the synovium
The middle phase of OA
- Moderate inflammatory changes of the synovium
- Synovium becomes hypervascular
Late phases of OA
- The synovium becomes increasingly thick and vascular
Bones
- Subchondral bone attempts to remodel by forming lytic lesions with sclerotic edges (different than bone cysts in RA) bone cysts form in late stages
Cell biology
- Proteolytic enzymes matrix metalloproteases (MMPs)
Responsible for cartilage matrix digestion
- Examples
- Stromelysin
- Plasmin
- Aggrecanase-1 (ADAM-TS-4)
Tissue inhibitors of MMPS (TIMPs)
- Control MMP activity preventing excessive degradation
- The imbalance between MMPs and TIMPs has been demonstrated in OA tissues
Inflammatory cytokines
Secreted by synoviocytes and increase MMP synthesis, examples
- IL-1
- IL-6
- TNF-alpha
Genetics >Inheritance
- in-mendelian
Genes potentially linked to OA
- vitamin D receptor
- estrogen receptor 1
- inflammatory cytokines
- IL-1
- leads to the catabolic effect
- IL-4
- matriline-3
- BMP-2, BMP-5
Possible Causes of Secondary Knee OA
-
Posttraumatic
-
Postsurgical
-
Congenital or malformation of the limb
-
Malposition (Varus/Valgus)
-
Scoliosis
-
Rickets
-
Hemochromatosis
-
Chondrocalcinosis
-
Ochronosis
-
Wilson disease
-
Gout
-
Pseudogout
-
Acromegaly
-
Avascular necrosis
-
Rheumatoid arthritis
-
Infectious arthritis
-
Psoriatic arthritis
-
Hemophilia
-
Paget disease
-
Sickle cell disease
Diet & Nutrition
- Vitamin D Overall – mixed results. Low vitamin D is associated with an increased risk of progression of knee OA compared to individuals with higher vitamin D. Serum vitamin D levels were not associated with the risk of hip OA. 2 cohort studies failed to confirm any protective effect of vitamin D supplementation on the structural worsening of knee OA
- Vitamin C – Low vitamin C dietary intake was associated with an increased risk of progression, but not incidence, of both radiographic and symptomatic knee OA
- Vitamin E – Supplementation with vitamin E failed to ameliorate symptoms in patients who had symptomatic knee OA or prevent knee OA progression
- Selenium – Animal studies: low selenium associated with irregular bone formation, decreased bone strength, and abnormalities in type I and II collagen in cartilage. Low selenium is associated with an increased risk of Kashin-beck disease, a form of arthritis, and the risk was reduced with selenium supplementation. Another study found high selenium intake was significantly associated with an increased risk of both hip and knee OA
- Vitamin K – Neogi et al: Low vitamin K associated with osteoarthritis of the hand and knee[44]
Risk Factor
Age is not the only factor that plays a role in the evolution of OA. Other risk factors are
- Obesity
- Joint hypermobility or instability
- Sports stress with high impact loading
- Repetitive knee bending or heavy weight lifting
- Specific occupations
- Peripheral neuropathy
- Injury to the joint
- History of immobilization
- Family history
Modifiable
-
Articular trauma
-
Occupation – prolonged standing and repetitive knee bending
-
Muscle weakness or imbalance
-
Weight
-
Health – metabolic syndrome
Non-modifiable
-
Gender – females more common than males
-
Age
-
Genetics
-
Race

Risk Factors can be Classified into Primary & secondary
Primary
- A number of studies have shown that there is a greater prevalence of the disease among siblings and especially identical twins, indicating a hereditary basis. Although a single factor is not generally sufficient to cause the disease, about half of the variation in susceptibility has been assigned to genetic factors
- As early human ancestors evolved into bipeds, changes occurred in the pelvis, hip joint, and spine which increased the risk of osteoarthritis. Additionally, genetic variations that increase the risk were likely not selected against because usually problems only occur after reproductive success.
- The development of osteoarthritis is correlated with a history of previous joint injury and with obesity, especially with respect to knees. Since the correlation with obesity has been observed not only for knees but also for non-weight bearing joints and the loss of body fat is more closely related to symptom relief than the loss of body weight, it has been suggested that there may be a metabolic link to body fat as opposed to just mechanical loading.
- Changes in sex hormone levels may play a role in the development of osteoarthritis as it is more prevalent among post-menopausal women than among men of the same age. A study of mice found natural female hormones to be protective while injections of the male hormone dihydrotestosterone reduced protection.
Secondary
This type of osteoarthritis is caused by other factors but the resulting pathology is the same as for primary osteoarthritis:
- Older age – The risk of osteoarthritis increases with age.
- Sex – Women are more likely to develop osteoarthritis, though it isn’t clear why.
- Obesity – Carrying extra body weight contributes to osteoarthritis in several ways, and the more you weigh, the greater your risk. Increased weight puts added stress on weight-bearing joints, such as your hips and knees. In addition, fat tissue produces proteins that may cause harmful inflammation in and around your joints.
- Joint injuries – Injuries, such as those that occur when playing sports or from an accident, may increase the risk of osteoarthritis. Even injuries that occurred many years ago and seemingly healed can increase your risk of osteoarthritis.
- Certain occupations – If your job includes tasks that place repetitive stress on a particular joint, that joint may eventually develop osteoarthritis.
- Genetics – Some people inherit a tendency to develop osteoarthritis.
- Bone deformities – Some people are born with malformed joints or defective cartilage, which can increase the risk of osteoarthritis.
- Inflammatory diseases – (such as Perthes’ disease), (Lyme disease), and all chronic forms of arthritis (e.g., costochondritis, gout, and rheumatoid arthritis). In gout, uric acid crystals cause the cartilage to degenerate at a faster pace.
- Diabetes doubles – the risk of having a joint replacement due to osteoarthritis and people with diabetes have joint replacements at a younger age than those without diabetes.
- Alkaptonuria
- Congenital disorders of joints
- Ehlers-Danlos Syndrome
- Hemochromatosis and Wilson’s disease
- Injury to joints or ligaments (such as the ACL), as a result of an accident or orthopedic operations.
- Ligamentous deterioration or instability may be a factor.
- Marfan syndrome
- Joint infection
The symptom of Osteoarthritis (OA) of the Knee
- Pain (particularly when you’re moving your knee or at the end of the day – this usually gets better when you rest)
- Stiffness (especially after rest – this usually eases after a minute or so as you get moving)
- Crepitus, a creaking, crunching, grinding sensation when you move the joint
- Hard swellings (caused by osteophytes)
- Soft swellings (caused by extra fluid in the joint).
- Loss of flexibility – You may not be able to move your joint through its full range of motion.
- Grating sensation – You may hear or feel a grating sensation when you use the joint.
- Bone spurs – These extra bits of bone, which feel like hard lumps, may form around the affected joint.
Other symptoms can include
- your knee giving way because your muscles have become weak or the joint structure is less stable
- your knee not moving as freely or as far as normal
- your knees becoming bent and bowed
- the muscles around your joint looking thin or wasted.
It’s unusual, but some people have pain in their knees that wakes them up at night. This generally only happens with severe osteoarthritis.
- You’ll probably find that your pain will vary and that you have good days and bad days, sometimes depending on how active you’ve been but sometimes for no clear reason.
- Some people find that changes in the weather (especially damp weather and low pressure) make their pain and stiffness worse. This may be because nerve fibers in the capsule of their knee are sensitive to changes in atmospheric pressure.
Diagnosis of Osteoarthritis (OA) of Knee
Physical Examination
During the physical examination, your doctor will look for:
- Joint swelling, warmth, or redness
- Tenderness in the knee
- The range of passive (assisted) and active (self-directed) motion
- Instability of the joint
- Crepitus (a grating sensation inside the joint) with movement
- Pain when weight is placed on the knee
- Problems with your gait (the way you walk)
- Any signs of injury to the muscles, tendons, and ligaments surrounding the knee
- Involvement of other joints (an indication of rheumatoid arthritis
Physical Exam
Skin
- Scars
- Trauma
- Erythema
- Swelling
- Muscle atrophy
- Normal quadriceps circumference >10 cm (VMO), 15 cm (quadriceps)
- Asymmetry
Gait
- Antalya
- Stride length
- Muscle weakness
Standing limb alignment
- Neutral, varus, valgus
- Joint line tenderness
Tenderness over soft tissue structures
- Pes anserine bursae
- Patellar tendon
- Iliotibial band
Point of maximal tenderness
- Effusion
- Patella balloting
- Milking
Active and passive
Flexion/extension normal range
- 10° extension (recurvatum) to 130° flexion
Rotation varies with flexion
- In full extension, there is ma animal rotation
- At 90° flexion, 45° ER, and 30° IR
Abduction/adduction
- In full extension, essentially 0°
- At 30° flexion, a few degrees of passive motion are possible
Sensation
- Medial thigh – obturator
- Anterior thigh – femoral
- Posterolateral calf – sciatic
- Dorsal foot – peroneal
- Plantar foot – tibial
Motor
- Thigh adduction – obturator
- Knee extension – femoral
- Knee flexion – sciatic
- Toe extension – peroneal
- Toe flexion – tibial
Vascular
Pulses
- Popliteal
- Dorsalis pedis
- Posterior tibial
Ankle-brachial index
- ABI < 0.9 is abnormal
- Large hemarthrosis
- Quadriceps avoidance gait (does not actively extend knee)
Pivot shift
- Extension to flexion: reduces at 20-30° of flexion
- The patient must be completely relaxed (easier to elicit under anesthesia)
- Mimics the actual giving way event
KT-1000
- Useful to quantify anterior laxity
- Measured with the knee in slight flexion and 10-30° externally rotation
PCL Injury
- Posterior sag sign – The patient lies supine with hips and knees flexed to 90°, examiner supports the ankles and observes for a posterior shift of the tibia as compared to the uninvolved knee
- Posterior drawer (at 90° flexion) – With the knee at 90° of flexion, a posteriorly directed force is applied to the proximal tibia and posterior tibial translation is quantified & the medial tibial plateau of a normal knee at rest is ~1 cm anterior to the medial femoral condyle
- Most accurate maneuver for diagnosing PCL injury Quadriceps active test– attempt to extend a knee flexed at 90° to elicit quadriceps contraction positive if the anterior reduction of the tibia occurs relative to the femur
MCL Injury
Valgus instability = medial opening
- 30° only – isolated MCL
- 0° and 30° – combined MCL and ACL and/or PCL
Classification
- Grade I: 0-5 mm opening
- Grade II: 6-10 mm opening
- Grade III: 11-15 mm opening
Anterior Drawer with the tibia in external rotation
- grade III MCL tears are often associated with ACL and posteromedial corner tears
- the positive test will indicate associated ligamentous injury
LCL Injury
Varus instability = lateral opening
- 30° only – isolated LCL
- 0° and 30° – combined LCL and ACL and/or PCL
- Varus opening and increased external tibial rotatory instability at 30° – combined LCL and posterolateral corner
PLC Injury
Gait
Varus thrust or hyperextension thrust
Varus stress test
- Varus laxity at 0° indicates both LCL & cruciate (ACL or PCL) injury
- Varus laxity at 30° indicates LCL injury.
Dial test
- > 10° ER asymmetry at 30° only consistent with isolated PLC injury
- > 10° ER asymmetry at 30° & 90° consistent with PLC and PCL injury
Reversed pivot shift test
- With the knee positioned at 90°, ER and valgus forces are applied to the tibia as the knee is extended, the tibia reduces with a palpable clunk tibia reduces from a posterior subluxed position at ~20° of flexion to a reduced position in full extension (reduction force from IT band transitioning from a flexor to an extensor of the knee)
External rotation recurvatum test
- positive when the leg falls into ER and recurvatum when the lower extremity is suspended by the toes in a supine patient
- Peroneal nerve assessment injury present with altered sensation to foot dorsum and weak ankle dorsiflexion
Meniscus Injury
- Joint line tenderness
- Effusion
McMurray’s test
- Flex the knee and place a hand on the medial side of the knee externally rotate the leg and bring the knee into extension
- A palpable pop or click is a positive test and can correlate with a medial meniscus tear
Patella Pathology
Large hemarthrosis
- The absence of swelling supports ligamentous laxity and habitual dislocation mechanism
- Medial-sided tenderness (over MPFL)
- Increase in passive patellar translation
- Measured in quadrants of translation (midline of the patella is considered “0”) and should be compared to the contralateral side
- Normal motion is <2 quadrants of patellar translation
- Lateral translation of the medial border of the patella to the lateral edge of the trochlear groove is considered “2” quadrants and is an abnormal amount of translation
- Patellar apprehension
- Increased Q angle
J sign
- Excessive lateral translation in extension which “pops” into the groove as the patella engages the trochlea early inflection
- Associated with patella alta
Grading Knee
For the grading of osteoarthritis in the knee, the most reliable systems are the International Knee Documentation Committee (IKDC) system and the Ahlbäck system, which have been found to be superior to for example systems by Kellgren-Lawrence, Fairbank, Brandt, and Jäger-Wirth. These findings refer to posteroanterior weight-bearing projection radiographs made with the knee in 45° of flexion.
[stextbox id=’info’]
| Grade | Findings |
|---|---|
| I | Joint space narrowing, with or without subchondral sclerosis. Joint space narrowing is defined by this system as a joint space less than 3 mm, or less than half of the space in the other compartment, or less than half of the space of the homologous compartment of the other knee. |
| II | Obliteration of the joint space |
| III | Bone defect/loss <5 mm |
| IV | Bone defect/loss between 5 and 10 mm |
| V | Bone defect/loss >10 mm, often with subluxation and arthritis of the other compartment |
For the patellofemoral joint, a classification by Merchant 1974 uses a 45° “skyline” view of the patella
| Stage | Description |
|---|---|
| 1 (mild) | Patellofemoral joint space > 3mm |
| 2 (moderate | Joint space < 3 mm but no bony contact |
| 3 (severe) | Bony surfaces in contact over less than one-quarter of the joint surface |
| 4 (very severe) | Bony contact throughout the entire joint surface |
[/stextbox]
Goldberg RJ recommends the following as a common approach to the examination of all joints
-
Make sure the area is well exposed—no clothing covering either side. Patient gowns come in handy
-
Carefully inspect the joint or joints in question – Are there signs of inflammation or injury (swelling, redness, warmth)? Deformity? Because many joints are symmetrical, compare it with the opposite side
-
Understand normal functional anatomy – What does this joint normally do?
-
Observe the joint – while the patient attempts to perform the normal activity. What can’t the patient do? What specifically limits him/her? Was there a discrete event (eg, trauma) that caused this? If so, what was the mechanism of injury?
-
Palpate the joint in question – Is there warmth? Point tenderness? If so, over what anatomic structures?
-
Assess the range of motion – both active (patient moves it) and passive (you move it). If the active range of motion is limited, determine the causes of pain
-
Perform strength and neurovascular assessments
-
Perform specific provocative maneuvers related to pathology occurring in that joint (Goldberg[Rx])presents some for each joint)
-
In the setting of acute injury and pain, it is often very difficult to assess a joint because the patient “protects” the affected area, limiting movement and thus your examination. It helps to examine the unaffected side first. This will help to set the patient at ease and will help the physician gain a sense of the patient’s normal range of motion.
Histopathology
Cartilage Changes in Aging
-
Water content – decreased
-
Collagen – same
-
Proteoglycan content – decreased
-
Proteoglycan synthesis – same
-
Chondrocyte size – increased
-
Chondrocyte number – decreased
-
Modulus of elasticity – increased
Cartilage Changes in OA
-
Water content – increased
-
Collagen – disorganized
-
Proteoglycan content – decreased
-
Proteoglycan synthesis – increased
-
Chondrocyte size – same
-
Chondrocyte number – same
-
Modulus of elasticity – decreased
Matrix Metalloproteases
Responsible for cartilage matrix degradation
-
Stromelysin
-
Plasmin
-
Aggrecanase-1 (ADAMTS-4)
-
Collagenase
-
Gelatinase
Tissue inhibitors of MMPs & Control MMP activity preventing excess degradation
-
TIMP-1
-
TIMP-2
-
Alpha-2-macroglobulin
Areas of focus for the medial aspect of the knee
-
Vastus medialis obliquus
-
Superomedial pole patella
-
A medial facet of the patella
-
Origin of the medial collateral ligament (MCL)
-
Midsubstance of the MCL
-
Broad insertion of the MCL
-
Medial joint line
-
Medial meniscus
-
Pes anserine tendons and bursa
Areas of focus for the midline of the knee
-
Quadricep tendon
-
Suprapatellar pouch
-
Superior pole patella
-
Patellar mobility
-
Prepatellar bursa
-
Patellar tendon
-
Tibial tubercle
Areas of focus for the lateral aspect of the knee
-
Iliotibial band
-
Lateral facet patella
-
Lateral collateral ligament (LCL)
-
Lateral joint line
-
Lateral meniscus
-
Gerdy’s tubercle
A thorough neurovascular exam should be performed and documented. It is important to assess the strength of the quadriceps and hamstring muscles as these often times will become atrophied in the presence of knee pain. A sensory exam of the femoral, peroneal, and tibial nerve should be assessed as there may be concomitant neurogenic symptoms associated. Palpation of a popliteal, dorsal pedis, and posterior tibial pulse is important as any abnormalities may raise the concern for vascular problems. Other knee tests may be performed, depending on clinical suspicion based on history.
Lab Diagnostic
Laboratory tests and x-rays are often used in addition to these criteria.
- Osteoarthritis of the hand can often be diagnosed on the basis of these criteria alone, and laboratory tests and x-rays may be unnecessary. But in some cases, it is needed.
- A normal erythrocyte sedimentation rate (ESR)
- The presence of bony outgrowths (osteophytes) on x-rays
- The presence of joint space narrowing on x-rays indicates a loss of cartilage
www.rxharun.com
The number of characteristics associated with knee pain varies depending on whether a diagnosis is being made using clinical criteria only, using clinical and radiographic criteria, or using clinical and laboratory criteria, as follows
-
Crepitus on active joint motion
-
Morning stiffness less than 30 minutes duration
-
age older than 50 years
-
Bony enlargement of the knee on examination
-
Bony tenderness of the knee on examination
-
No palpable warmth.
-
Crepitus on active motion
-
Morning stiffness less than 30 minutes duration
-
Age older than 50 years.
-
Crepitus on active joint motion
-
Morning stiffness less than 30 minutes duration
-
Age older than 50 years
-
Bony tenderness to palpation
-
Bony enlargement
-
No palpable warmth
-
Erythrocyte sedimentation rate below 40 mm/h
-
A rheumatoid factor less than 1:40
-
Synovial fluid is consistent with OA (white blood cell count < 2000/μL).
Laboratory tests may be recommended to help diagnose OA by ruling out conditions with similar symptoms.
Imaging tests
- X-rays are often helpful for tracking the status of OA over time, but x-rays may appear normal during the early stages.
- Other types of imaging tests, such as ultrasound and magnetic resonance imaging (MRI), may be used to detect damage to cartilage, ligaments, and tendons, which cannot be known by the following an investigation
[stextbox id=’info’]
American College of Rheumatology criteria for the diagnosis of knee osteoarthritis
| Using history and clinical examination* |
| Pain in the knee and three of the following |
| 1-Age >50 years |
| 2- Morning stiffness <30 minutes |
| 3-Crepitus on active motions |
| 4-Bony tenderness |
| 5-Bony enlargement |
| 6-No palpable warmth of synovium |
| Using history and clinical examination and radiographic findings |
| Pain in the knee and one of the following |
| 1-Age >50 years |
| 2- Morning stiffness < 30 minutes |
| 3-Crepitus on active motions and osteophyte |
| Using history and clinical examination and laboratory findings |
| Pain in the knee and 5 of the following |
| 1- Age >50 years |
| 2- Morning stiffness <30 minutes |
| 3-Crepitus on active motions |
| 4-Bony enlargement |
| 5-No palpable warmth of synovium |
| 6-ESR <40 mm/h |
| 7-Rheumatoid Factor <1/40 |
| 8-Synovial fluid signs of osteoarthritis |
*Reference: Altman, R, et al.: Arthritis Rheum 29:1039, 1986.
[/stextbox]
Special knee tests
-
Patella apprehension – patellar instability
-
J-sign – patellar maltracking
-
Patella compression/grind – chondromalacia or patellofemoral arthritis
-
Medial McMurray – a medial meniscus tear
-
Lateral McMurray – lateral meniscus tear
-
Thessaly test – a meniscus tear
-
Lachman – anterior cruciate ligament (ACL) injury
-
Anterior drawer – ACL injury
-
Pivot shift – ACL injury
-
Posterior drawer – posterior cruciate ligament (PCL) injury
-
Posterior sag – PCL injury
-
Quadriceps active test – PCL injury
-
Valgus stress test – MCL injury
-
Varus stress test – LCL injury
Treatment of Osteoarthritis (OA) of the Knee
Treatment for knee osteoarthritis can be broken down into non-surgical and surgical management. Initial treatment begins with non-surgical modalities and moves to surgical treatment once the non-surgical methods are no longer effective. A wide range of non-surgical modalities is available for the treatment of knee osteoarthritis. These interventions do not alter the underlying disease process, but they may substantially diminish pain and disability.
The non-pharmacological approach includes
- Education –Encourage patients to participate in self-management programs (such as those conducted by the Arthritis Foundation in the United States and Arthritis Care in the United Kingdom), and provide resources for social support and instruction on coping skills.
- Weight loss – Encourage overweight patients with osteoarthritis of the hip and knee to lose weight through a combination of diet and exercise.[Rx]
- Exercise – increases aerobic capacity, muscle strength, and endurance and also facilitates weight loss. All people capable of exercise should be encouraged to take part in a low-impact aerobic exercise program (walking, cycling, swimming or another aquatic exercise). Exercises to strengthen the quadriceps lead to reductions in pain and improvements in function.
- Physical therapy – consists of several strategies to facilitate the resolution of symptoms and improve functional deficits, including a range of motion exercise, muscle strengthening, muscle stretching, and soft tissue mobilization.
- Knee braces and orthotics – For those with the instability of the knee and varus misalignment, valgus bracing and orthotics shift the load away from the medial compartment and, in doing so, may provide relief of pain and improvement in function.[Rx] Though some research has shown that heel wedges can reduce medial compartment loads, there is no evidence that used alone, they improve knee symptoms.[Rx] Appropriate supportive footwear should be worn by people who have osteoarthritis of the knee and hip.
- Shoe inserts – Consider trying splints, braces, shoe inserts, or other medical devices that can help reduce your pain. These devices can immobilize or support your joint to help you keep pressure off it.
The first-line treatment for all patients with symptomatic knee osteoarthritis includes patient education and physical therapy. A combination of supervised exercises and a home exercise program have been shown to have the best results. These benefits are lost after 6 months if the exercises are stopped. The American Academy of Orthopedic Surgeons (AAOS) recommends this treatment.
The Medication of Osteoarthritis (OA) of the Knee
The goal of treatment is to decrease pain and increase mobility.
- Analgesics – Paracetamol (up to 4 g/day) is the oral analgesic of choice for mild to moderate pain in osteoarthritis. NSAIDs should be added or substituted in patients who respond inadequately and are sometimes the first choice because of greater efficacy and patients’ preference.[rx] There are, however, certain disadvantages of routinely using NSAIDs—for example, all NSAIDs (non-selective and COX 2 selective) are associated with potential toxicity, particularly in elderly people. COX 2 selective inhibitors have also been associated with an increased risk for cardiovascular disease. Rofecoxib, a COX 2 selective inhibitor, was recently withdrawn because of such concerns. In people with an increased gastrointestinal risk, nonselective NSAIDs plus a gastroprotective agent or a selective COX 2 inhibitor should be used. Opioid analgesics are useful alternatives in patients in whom NSAIDs are contraindicated, ineffective, or poorly tolerated. Topical formulations of NSAIDs and capsaicin may be helpful.
- Antidepressants – Drugs that block pain messages from your brain and boost the effects of endorphins (your body’s natural painkillers).
- Nonsteroidal anti-inflammatory drugs (NSAIDs) Common pain remedies such as aspirin, acetaminophen, ibuprofen, and naproxen can offer short-term relief. All are available in low doses without a prescription. Other medications, including muscle relaxants and anti-seizure medications, treat aspects such as muscle spasms and damaged nerves.
- Corticosteroid injections – Your doctor will inject a steroid such as prednisone into your thumb joints. Steroids make the inflammation go down. However, because of side effects, they are used sparingly
- Anesthetics – Used with precision, an injection of a “nerve block” can stop the pain for a time.
- Muscle Relaxants – These medications provide relief from spinal muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications: These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – to improve bone health and heal fractures.
- Glucosamine & diacerein– can be used to tighten the loose tension and regenerate cartilage or inhabit the further degeneration of cartilage. Possibly as a function of this publicity, osteoarthritis is the leading medical condition for which people use alternative therapies. Glucosamine and chondroitin seem to have the same benefit as a placebo,[Rx]and there is controversy over whether they also have structure modifying benefits.
- Muscle relaxants – such as cyclobenzaprine might be prescribed to relieve the discomfort associated with muscle spasms. However, these medicines might cause confusion in older people. Depending on the level of pain, prescription pain medicines might be used in the initial period of treatment.
- Over-the-counter – non-narcotic pain relievers and anti-inflammatory medications are usually the first choices of therapy for arthritis of the knee. Acetaminophen is a simple, over-the-counter pain reliever that can be effective in reducing arthritis pain that is following
Intra-Articular Knee Injection Treatments
-
Viscosupplementation with hyaluronic acid (HA) – Injection into the knee with HA (similar to the main component in cartilage) has been reported to provide temporary pain relief for up to three months. Evidence to date on the use of HA has been contradictory, and recommendations regarding its use remain inconclusive[,Rx ]Currently, the American Academy of Orthopaedic Surgeons does not recommend using hyaluronic acid for patients with symptomatic end-stage osteoarthritis (OA) of the knee.
-
There are no existing data that any of the HA injections – will cause regression of osteophytes, subchondral bone remodeling, or regeneration of cartilage and meniscus in patients with substantial, irreversible bone and cartilage damage. Further investigations are required to determine whether high-molecular-weight and cross-linked preparations of HA have superior efficacy compared with other HA preparations or other currently available treatments. Because of the paucity of data supporting the effectiveness of HA injections to justify their cost, careful patient selection and decreasing the use of HA among patients with end-stage knee OA may represent a substantial cost reduction without negatively affecting the quality of health care.Rx
-
Intra-articular corticosteroids – Intra-articular injections of corticosteroids have long been used to try to relieve symptoms of knee OA, but studies addressing their efficacy have been contradictory. The American Academy of Orthopaedic Surgeons guidelines for nonoperative treatment options for patients with OA of the knee does not recommend for or against the use of intra-articular corticosteroids in the knee. Rx Furthermore, a recent Cochrane systematic review concluded that clinically important benefits of one to six weeks remain unclear because of the overall quality of the studies, the heterogeneity between trials, and the presence of small-study effects. Rx
- Cortisone shots – Injections of corticosteroid medications may relieve pain in your joint. During this procedure, your doctor numbs the area around your joint, then places a needle into the space within your joint and injects the medication. The number of cortisone shots you can receive each year is limited because the medication can worsen joint damage over time.
- Lubrication injections – Injections of hyaluronic acid derivatives (Hyalgan, Synvisc) may offer pain relief by providing some cushioning in your knee. These agents are similar to a component normally found in your joint fluid.
- Realigning bones – During a surgical procedure called an osteotomy, the surgeon cuts across the bone either above or below the knee to realign the leg. Osteotomy can reduce knee pain by shifting your body weight away from the worn-out part of your knee.
Biologics
-
Cell-based therapies – Cell-based therapies for knee OA are in the development stages. A recent systematic review suggested that intra-articular cellular injections for OA and focal cartilage defects in the human knee had positive results and seemed safe. However, improvement in patient symptoms was modest and a placebo effect could not be disregarded. The overall quality of the literature was poor; therefore, accurate assessment and optimization of these therapies will require further research. Rx Most of the studies analyzed reported on the use of autologous cellular therapies. Bone marrow-derived cells were the source chosen more often, followed by adipose-derived cells and blood stem cells.
-
Platelet-rich plasma – Multiple studies and systematic reviews have reported on the use of intra-articular PRP for the treatment of knee OA.Rx Initial observations support an inference that PRP appears to be safe. Although some transient pain or swelling has been reported after its use, these symptoms typically resolve within two to three days, and no long-term side effects have been reported.
-
Use of PRP – especially a lower leukocyte concentration known as leukocyte-poor PRP, showed improved results compared with HA and placebo, showing beneficial effects of amelioration in pain and improvement in function about two months after application and lasting up to a year. Rx–Rx On the basis of the current evidence, although PRP injections have been demonstrated to more effectively reduce pain and improve overall physical function compared with control studies, the quality of evidence is lacking, and further research is required to establish the efficacy of using PRP as a treatment option.
-
Hyaluronic acid injections – Hyaluronic acid is meant to supplement a natural substance that gives joint fluid its viscosity. Most of the studies conducted have been in patients with knee OA. Although the study outcomes differ, some do find the treatment relieves pain. Hyaluronic acid injections seem to reach their peak benefit 8 weeks after the shot is given, and the effect lasts for about 24 weeks. Side effects were minimal, including temporary pain and swelling at the injection site. Because of inconsistent study results, hyaluronic acid injections are “not appropriate” for people with OA in the hip and other joints, and “uncertain” for those with knee-only OA.
-
Risedronate (Actonel) – This bisphosphonate drug is better known for treating osteoporosis, but it may also reduce cartilage degeneration. More studies are needed to determine whether risedronate helps with symptoms, function, or OA disease progression. For now, the drug is deemed “not appropriate.”
-
Disease-modifying anti-rheumatic drugs (DMARDs) – are used to slow the progression of rheumatoid arthritis. Drugs like methotrexate, sulfasalazine, and hydroxychloroquine are commonly prescribed. In addition, biologic DMARDs like etanercept and adalimumab may reduce the body’s overactive immune response. Because there are many different drugs today for rheumatoid arthritis, a rheumatology specialist is often required to effectively manage medications.
Bisphosphonates
- Inhibition of osteoclast activity may reverse subchondral bone changes
- In a small study, risedronate significantly reduced markers of cartilage degradation and bone resorption at 1-year follow-up. In a much larger study, risedronate (compared with placebo) did not improve signs or symptoms of OA, nor did it alter the progression of OA, a reduction in the level of a marker of cartilage degradation was observed. In a small study, zoledronic acid reduced knee pain, the size of bone marrow lesions over 6 months
Strontium Ranelate
- Used for osteoporosis, stimulates calcium receptors and increases bone formation. Poorly researched for use in osteoarthritis. Treatment with strontium ranelate 1 and 2 g/day is associated with a significant effect on structure in patients with knee osteoarthritis, and a beneficial effect on symptoms for strontium ranelate 2 g/day
AMG 108
- Is a monoclonal antibody against the interleukin 1 receptor. Demonstrated statistically insignificant but numerically greater improvements in pain; however, minimal, if any, clinical benefit was observed.
Adalimumab
- A trade name is Humira. Is a monoclonal antibody to TNFα. No difference in disease progression between adalimumab and placebo at 12 months of follow-up. This small, non-blinded study showed improvement in pain, stiffness, function, and joint swelling at 12 weeks
Topical Medications
Capsaicin
- Safe, well-tolerated, no systemic toxicity. Application site burning pain peaks at one weak and resolves over time. Administered four times daily, capsaicin is moderately effective in reducing pain intensity up to 20 weeks regardless of site of application and dose in patients with at least moderate pain and clinical or radiologically defined OA, and is well tolerated.
Topical NSAIDs
- Recommended by governing bodies for hand and knee OA. Topical and oral NSAIDs demonstrate an equivalent effect on knee pain over 1 year of treatment, with fewer adverse events due to lower systemic absorption of topical NSAIDs compared with oral NSAIDs
Supplements
Fish Oil
- Used for a variety of ailments in addition to OA. Contains omega-3 polyunsaturated fatty acids. Anti-inflammatory and chondroprotective in animal studies. In a double-blinded RCT, No benefit when added to glucosamine compared to placebo[75]
S-adenosylmethionine (SAMe)
- Soeken et al meta-analysis: similar effect to NSAIDs in reducing pain, improving function with fewer adverse events. Not limited to only 2 studies
Methylsulfonylmethane (MSM)
- When combined with glucosamine compared to glucosamine alone, there was increased efficacy in reducing pain and swelling and in improving the functional ability of joints than the individual agents. Kim et al: randomized, double-blinded RCT MSM twice a day improved symptoms of pain and physical function over the 12 week study period
Collagen Hydrolysate
- Collagen hydrolysate ingestion stimulates a statistically significant increase in the synthesis of extracellular matrix macromolecules by chondrocytes. Two small studies suggest that it helps with pain from knee OA
Passion Fruit Peel Extract
- In a small, randomized, double-blinded placebo-controlled study, there was a statistically significant reduction in pain, stiffness, physical function, and WOMAC score compared to a placebo
Curcuma Longa Extract
- In this small, randomized, single-blind, placebo-controlled trial of patients with primary knee OA, Curcuma longa extract showed a significant decrease in knee pain. Additionally shown to reduce serum levels of inflammatory markers IL-1, malondialdehyde[84]
Boswellia Serrata Extract (BSE)
- A randomized double-blind placebo-controlled crossover study had a statistically significant decrease in knee pain and swelling, increased flexion, and walking. BSE showed a slower onset of action but the effect persisted even after stopping therapy compared to valdecoxib
Curcumin
- In patients with undefined arthritis, a brand-name formulation successfully improved WOMAC score, walking distance, and decreased CRP
Pine Bark Extract
- Brand name Pycnogenol. Exerts antioxidative, anti-inflammatory, and chondroprotective effects in vitro and in vivo. Provides long-lasting positive effects such as enhanced physical mobility and pain relief for patients with mild OA. In 100 patients with knee OA randomized to pine bark extract or placebo, patients reported improved WOMAC score and alleviation of pain compared to placebo[89]
L-Carnitine
- In a randomized double-blind placebo-controlled trial of women with knee OA, Kolahij et al found 750 mg/day was superior to placebo for pain reduction, stiffness, physical function, and WOMAC score
Intra-Articular Injections
Dextrose Prolotherapy
- Injection of dextrose into pathologic joint in order to generate an inflammatory process. Note: injectant can be substance other than dextrose, however dextrose most common
- Rahimzadeh et al found that prolotherapy decreased WOMAC scores. Note they also found PRP to be superior to prolotherapy. 3 Arm study: Dextrose prolotherapy resulted in clinically meaningful sustained improvement of pain, function, and stiffness scores for knee osteoarthritis compared with blinded saline injections and at-home exercises[98]
Lubricin
- A glycoprotein that acts synergistically with Hyaluronic acid. Minimal research at this time, however, offers therapeutic potential. Supplementation restores normal joint lubrication and might be chondroprotective[100][101]
Anakinra
- The recombinant antagonist of interleukin-1 receptor
- Anakinra was well-tolerated as a single 50‐mg or 150‐mg intraarticular injection in patients with OA of the knee. However, anakinra was not associated with improvements in OA symptoms compared with placebo.
Sprifermin
- Also known as recombinant human fibroblast growth factor 18 (rhFGF18). Intra-articular administration of 100 μg of sprifermin every 6 or 12 months vs placebo resulted in an improvement in total femorotibial joint cartilage thickness after 2 years that was statistically significant, but of uncertain clinical importance[103]
Regenerative Medicine
Stem Cell Therapy
- General Poorly understood and studied
Dextrose Prolotherapy
- General, Injection of dextrose into pathologic joint in order to generate an inflammatory process. Note: injectant can be substance other than dextrose, however dextrose most common
- Rahimzadeh et al found that prolotherapy decreased WOMAC scores. Note they also found PRP to be superior to prolotherapy. 3 Arm study: Dextrose prolotherapy resulted in clinically meaningful sustained improvement of pain, function, and stiffness scores for knee osteoarthritis compared with blinded saline injections and at-home exercises[106]
Surgical Treatment
Your doctor may recommend surgery if your pain from arthritis causes disability and is not relieved with nonsurgical treatment. As with all surgeries, there are some risks and possible complications with different knee procedures. Your doctor will discuss the possible complications with you before your operation.
- Arthroscopy – During arthroscopy, doctors use small incisions and thin instruments to diagnose and treat joint problems. Arthroscopic surgery is not often used to treat arthritis of the knee. In cases where osteoarthritis is accompanied by a degenerative meniscal tear, arthroscopic surgery may be recommended to treat the torn meniscus.
- Cartilage grafting – Normal, healthy cartilage tissue may be taken from another part of the knee or from a tissue bank to fill a hole in the articular cartilage. This procedure is typically considered only for younger patients who have small areas of cartilage damage.
- Synovectomy – The joint lining damaged by rheumatoid arthritis is removed to reduce pain and swelling.
- Osteotomy – In a knee osteotomy, either the tibia (shinbone) or femur (thighbone) is cut and then reshaped to relieve pressure on the knee joint. Knee osteotomy is used when you have early-stage osteoarthritis that has damaged just one side of the knee joint. By shifting your weight off the damaged side of the joint, an osteotomy can relieve pain and significantly improve function in your arthritic knee.
- Total or partial knee replacement (arthroplasty) – Your doctor will remove the damaged cartilage and bone, and then position new metal or plastic joint surfaces to restore the function of your knee. (Left) A partial knee replacement is an option when damage is limited to just one part of the knee. (Right) A total knee replacement prosthesis.
Surgical Treatment Options
-
Osteotomy
-
Unicompartmental knee arthroplasty (UKA)
-
Total knee arthroplasty (TKA)
A high tibial osteotomy (HTO) may be indicated for unicompartmental knee osteoarthritis associated with malalignment. Typically an HTO is done for varus deformities where the medial compartment of the knee is worn and arthritis. The ideal patient for an HTO would be a young, active patient in whom arthroplasty would fail due to excessive component wear. An HTO preserves the actual knee joint, including the cruciate ligaments, and allows the patient to return to high-impact activities once healed. It does require additional healing time compared to an arthroplasty, is more prone to complications, depends on bone and fracture healing, is less reliable for pain relief, and ultimately does not replace cartilage that is already lost or repaired any remaining cartilage. An osteotomy will delay the need for arthroplasty for up to 10 years.
Indications for HTO
-
Young (less than 50 years old), active patient
-
Healthy patient with good vascular status
-
Non-obese patients
-
Pain and disability interfering with daily life
-
Only one knee compartment is affected
-
A compliant patient who will be able to follow the postoperative protocol
Contraindications for HTO
-
Inflammatory arthritis
-
Obese patients
-
Knee flexion contracture greater than 15 degrees
-
Knee flexion less than 90 degrees
-
If the procedure will need greater than 20 degrees of deformity correction
-
Patellofemoral arthritis
-
Ligamentous instability
A UKA also is indicated in unicompartmental knee osteoarthritis. It is an alternative to an HTO and a TKA. It is indicated for older patients, typically 60 years or older, and relatively thin patients; although, with newer surgical techniques the indications are being pushed.
Indications for UKA
-
Older (60 years or older), lower demand patients
-
Relatively thin patients
Contraindications for UKA
-
Inflammatory arthritis
-
ACL deficiency
-
Fixed varus deformity greater than 10 degrees
-
Fixed valgus deformity greater than 5 degrees
-
Arc of motion less than 90 degrees
-
Flexion contracture greater than 10 degrees
-
Arthritis in more than one compartment
-
Younger, higher activity patients or heavy laborers
-
Patellofemoral arthritis
A TKA is the surgical treatment option for patients failing conservative management and those with osteoarthritis in more than one compartment. It is regarded as a valuable intervention for patients who have severe daily pain along with radiographic evidence of knee osteoarthritis.
Indications for TKA
-
Symptomatic knee OA in more than one compartment
-
Failed non-surgical treatment options
Contraindications for TKA
Absolute
-
Active or latent knee infection
-
Presence of active infection elsewhere in the body
-
Incompetent quadriceps muscle or extensor mechanism
Relative
-
Neuropathic arthropathy
-
Poor soft-tissue coverage
-
Morbid obesity
-
Noncompliance due to major psychiatric disorder or alcohol or drug abuse
-
Insufficient bone stock for reconstruction
-
Poor health or the presence of comorbidities that make the patient an unsuitable candidate for major surgery and anesthesia
-
Patient’s poor motivation or unrealistic expectations
-
Severe peripheral vascular disease
Advantages of UKA vs TKA
-
Faster rehabilitation and quicker recovery
-
Less blood loss
-
Less morbidity
-
Less expensive
-
Preservation of normal kinematics
-
Smaller incision
-
Less post-surgical pain and shorter hospital stay
Advantages of UKA vs HTO
-
Faster rehabilitation and quicker recovery
-
Improved cosmesis
-
The higher initial success rate
-
Fewer short-term complications
-
Lasts longer
-
Easier to convert to TKA
Physiotherapy Treatment
Strengthening Exercises
Knee extension
Straightening the knee against resistance will strengthen the quadriceps muscles at the front of the thigh. This can be achieved in a number of ways, including using ankle weights and resistance machines. One of the easiest ways involves using a resistance band
- The patient sits on a chair with one end of the band tied around their ankle and the other end around one of the chair legs.
- The band should be taut when the knee is bent at 90 degrees. The patient straightens the knee before slowly bending it and returning the foot back to the floor.
- Perform 10-15 repetitions and repeat this 2-3 times.
Knee flexion
Still using the resistance band
- The patient lies on the floor with the band tied around one ankle and the other end attached to something sturdy, close to the floor. The band should be taught when the knee is straight
- The patient bends the knee to bring the heel towards the buttock as far as possible, and then slowly straightens the knee back again.
- Perform 10-15 repetitions and repeat this 2-3 times.
Calf raise
Calf raises are good for strengthening the Gastrocnemius muscle which is one of the two main calf muscles, but the only one which crosses the knee joint.
- The patient stands with the feet should width apart and close to a wall or chair which can be held for balance if required.
- The patient rises up onto the toes, keeping the knees straight, before slowly lowering the heels back to the floor.
- Perform 10-15 repetitions and repeat this 2-3 times.
- This exercise can be progressed by performing on one leg only.
Squats
Squats are really good exercises for strengthening all the main muscle groups of the legs and buttocks. They can start off as very shallow movements and progress until the knees reach a 90-degree angle at which point weights can be added.
- The patient stands with the feet shoulder-width apart and backs straight.
- The knees are then bent as if trying to sit on a chair.
- The back should remain straight and the knees should not move forward past the toes.
- Perform 10-15 repetitions and repeat this 2-3 times.
Acupuncture
- It uses fine needles to stimulate specific body areas to relieve pain or temporarily numb an area. Although it is used in many parts of the world and evidence suggests that it can help ease the pain of arthritis, there are few scientific studies of its effectiveness. Be sure your acupuncturist is certified, and do not hesitate to ask about his or her sterilization practices.
- Magnetic pulse therapy – is painless and works by applying a pulsed signal to the knee, which is placed in an electromagnetic field. Like many alternative therapies, magnetic pulse therapy has yet to be proven.
As with other arthritic conditions, the initial treatment of arthritis of the knee is nonsurgical. Your doctor may recommend a range of treatment options.
Lifestyle modifications
Some changes in your daily life can protect your knee joint and slow the progress of arthritis.
- Minimize activities that aggravate the condition, such as climbing stairs.
- Switching from high-impact activities (like jogging or tennis) to lower-impact activities (like swimming or cycling) will put less stress on your knee.
- Losing weight can reduce stress on the knee joint, resulting in less pain and increased function.
- Physical therapy – Specific exercises can help increase the range of motion and flexibility, as well as help strengthen the muscles in your leg. Your doctor or a physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
- Assistive devices – Using devices such as a cane, wearing shock-absorbing shoes or inserts, or wearing a brace or knee sleeve can be helpful. A brace assists with stability and function and may be especially helpful if the arthritis is centered on one side of the knee. There are two types of braces that are often used for knee arthritis: An “unloader” brace shifts weight away from the affected portion of the knee, while a “support” brace helps support the entire knee load.
- Occupational therapy – An occupational therapist can help you discover ways to do everyday tasks or do your job without putting extra stress on your already painful joint. For instance, a toothbrush with a large grip could make brushing your teeth easier if you have finger osteoarthritis. A bench in your shower could help relieve the pain of standing if you have knee osteoarthritis.
- Other remedies – Applying heat or ice, using pain-relieving ointments or creams, or wearing elastic bandages to provide support to the knee may provide some relief from pain.
- Aerobic exercise – programs may make OA patients feel better, help reduces joint pain, and make it easier for them to perform daily tasks. Exercise programs under medical supervision should be balanced with rest and joint care.[Rx] Aerobic programs truly border both clinical (rehabilitation) and home programs. Regardless of the setting, this program type was found to be effective in reducing pain in the hip and knee.[Rx] Patients are typically recommended to exercise between 50% and 70% target heart rate for a minimum of 30 min, 3 times a week, for overall weight management, health benefits, and a reduction in pain which was noted after a 6-month program.[Rx]
- Hydrotherapy (balneotherapy) – involves the use of water in any form or at any temperature (steam, liquid, ice) for the purpose of healing. In aquatic physical therapy or hydrotherapy, exercise activities are carried out in heated pools by a variety of providers.[Rx] Hydrotherapy/balneotherapy and aquatic therapy displayed positive results when conducted for testing a subject’s strength and flexibility. The results emphasized the role of these therapies in aiding normal walking and relieving joint pain.[Rx] The sessions typically run from 6 to 48 weeks for the duration of 60 min and are conducted in a shallow pool with water temperatures ranging from 29°C to 34°C.[Rx]
Natural Relief From Arthritis Pain
Arthritis Pain

- Arthritis is a painful and degenerative condition marked by inflammation in the joints that causes stiffness and pain. Osteoarthritis, the most common type of arthritis, gets worse with age and is caused by wear and tear over the years.
- Doctors traditionally treat arthritis with anti-inflammatory medications and painkillers. However, some medications cause side effects, and a natural approach to pain relief is becoming more popular. Remember to consult your doctor before trying these natural remedies.
- Your weight can make a big impact on the amount of pain you experience from arthritis.
- Extra weight puts more pressure on your joints—, especially your knees, hips, and feet. Reducing the stress on your joints by losing weight will improve your mobility, decrease pain, and prevent future damage to your joints.
Get More Exercise
- There are more benefits to exercise than just weight loss. Regular movement helps to maintain flexibility in your joints. Weight-bearing exercises like running and walking can be damaging. Instead, try low-impact exercises like water aerobics or swimming to flex your joints without adding further stress.
Use Hot and Cold Therapy
- Simple hot and cold treatments can make a world of difference when it comes to arthritis pain. Long, warm showers or baths—especially in the morning—help ease stiffness in your joints. Use an electric blanket or heating pad at night to keep your joints loose and use moist heating pads.
- Cold treatments are best for relieving joint pain. Wrap a gel ice pack or a bag of frozen vegetables in a towel and apply it to painful joints for quick relief
Use Meditation to Cope With Pain
- Meditation and relaxation techniques may be able to help you reduce pain from arthritis by reducing stress and enabling you to cope with it better. According to the National Institutes of Health (NIH), studies have found that the practice of mindfulness meditation is helpful for some people with painful joints. Researchers also found that those with depression and arthritis benefitted the most from meditation.
Include the Right Fatty Acids in Your Diet
- Everyone needs omega-3 fatty acids in their diets for optimum health. However, these fats may also help your arthritis. Fish oil supplements, which are high in omega-3s, may help reduce joint stiffness and pain.
- Another fatty acid that can help is gamma-linolenic acid or GLA. It’s found in the seeds of certain plants like evening primrose, borage, hemp, and black currants. You can also buy the oils of the seeds as a supplement. However, be sure to check with your doctor before taking them.
Turmeric to Dishes
- Turmeric, the yellow spice common in Indian dishes, contains a chemical called curcumin that may be able to reduce arthritis pain. The secret is its anti-inflammatory properties.
- The NIH reports that turmeric given to lab rats reduced inflammation in their joints. Research on humans is scarce, but it can’t hurt to add this tasty spice to your dinners.
Massage
- According to the Arthritis Foundation, regular massaging of arthritic joints can help reduce pain and stiffness and improve your range of motion. Work with a physical therapist to learn self-massage, or schedule appointments with a massage therapist regularly
- Your massage therapist should be experienced with working on people who have arthritis. Check with your doctor for a recommendation.
Consider Herbal Supplements
- There are many kinds of herbal supplements on the market that claim to be able to reduce joint pain. Some of the herbs touted for arthritis pain include Boswellia, bromelain, devil’s claw, ginkgo, stinging nettle, and thunder god vine.
- Always talk to your doctor before trying a new supplement to avoid side effects and dangerous drug interactions.
Homeopathic medicines for Osteoarthritis
- Bryonia Alba – The excellent remedy which is useful in the treatment of osteoarthritis, pain with inflammation that is aggravated by movement and relieved by moderate pressure and rest. There is inflammation of joints which are hot and swollen.
- RhusToxm – Recurring attacks due to getting chilled. Rheumatism is caused by damp weather and worse in damp climate; there is restlessness and the pains are worse on first motion, better by continued motion
- Kali Carb – pains stitching, stabbing, and burning character relieved temporarily by cold application and not by rest or motion. The patient shrieks on account of pain. Backache accompanied by great weakness
- Arnica – Chronic arthritis with a feeling of bruised soreness can indicate a need for this remedy. Pain is worse from touch and may occur in joints that were injured in the past.
- Ruta graveolens – Arthritis with a feeling of great stiffness and lameness, worse from cold and damp, and worse from exertion often is relieved by this remedy. Tendons and the capsules of the joints may be affected. Arthritis may have developed after overuse, from repeated wear and tear.
- Kalmia latiflora – Intense arthritic pain that appears quite suddenly may indicate this medicine—especially when the problems start in higher joints and extend to lower ones. Pain and inflammation often start in the shoulder, moving to the elbow, wrist, and hand. The knees are also frequently affected. Discomfort is worse from motion and often worse at night.
- Apismellifica – This remedy can be helpful in acute conditions with redness, tenderness, and swelling. Joints feel hot and have stinging pain. The hands and knees are often affected. Warmth can aggravate the symptoms and cool applications bring relief.
- Calcarea fluorica – This medicine is often indicated for arthritic pains that are improved by heat and motion. Joints become enlarged and hard, and nodosities or bone spurs may develop. Arthritis after a chronic injury to joints often responds to Calcarea fluorica.
- Calcarea carbonica – This remedy is often useful for arthritis in a person who is flabby or overweight, and easily tired by exertion. Inflammation and soreness are worse from cold and dampness, and weakness or cramping in the extremities are often seen. Problems often focus on the knees when Calcarea is needed.
- Sticta Pulmonaria – Rheumatism of right shoulder blade or joint, wrist joint, ankle joint and knee joint. It also reduces fluid in the joints.
Complications
Complications associated with non-surgical treatment are largely associated with NSAID use.
Common Adverse Effects of NSAID Use
-
Stomach pain and heartburn
-
Stomach ulcers
-
A tendency to bleed, especially while taking aspirin
-
Kidney problems
Common Adverse Effects of Intra-Articular Corticosteroid Injection
-
Pain and swelling (cortisone flare)
-
Skin discoloration at the site of injection
-
Elevated blood sugar
-
Infection
-
Allergic reaction
Common Adverse Effects of Intra-Articular HA Injection
-
Injection site pain
-
Muscle pain
-
Trouble walking
-
Fever
-
Chills
-
Headache
Complications Associated with HTO
-
Recurrence of deformity
-
Loss of posterior tibial slope
-
Patella baja
-
Compartment syndrome
-
Peroneal nerve palsy
-
Malunion or nonunion
-
Infection
-
Persistent pain
-
Blood clot
Complications Associated with UKA
-
Stress fracture of the tibia
-
Tibial component collapse
-
Infection
-
Osteolysis
-
Persistent pain
-
Neurovascular injury
-
Blood clot
Complications Associated with TKA
-
Infection
-
Instability
-
Osteolysis
-
Neurovascular injury
-
Fracture
-
Extensor mechanism rupture
-
Patellar maltracking
-
Patellar clunk syndrome
-
Stiffness
-
Peroneal nerve palsy
-
Wound complications
-
Heterotopic ossification
-
Blood clot
References











