Sjogren’s Syndrome Causes/Sjogren’s syndrome (SS) is an autoimmune disorder caused by the lymphocytic infiltration of exocrine glands resulting in glandular dysfunction, preferentially of the salivary and lacrimal glands [rx]. It can be classified into two types, namely primary Sjogren’s syndrome, and secondary Sjogren’s syndrome. Primary Sjogren’s syndrome (pSS) occurs in the absence of other autoimmune diseases and is characterized by keratoconjunctiva sicca (dry eyes) and xerostomia (dry mouth), collectively called the sicca syndrome. In contrast, secondary Sjogren’s syndrome presents along with other autoimmune diseases such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) [rx].
Sjögren’s syndrome is a chronic inflammatory autoimmune disease of unknown origin, attacking, in particular, the tear and salivary glands. Sicca symptoms are the hallmarks of the disease which may also present with various organ manifestations. Due to the wide variety of signs and symptoms, patients with Sjögren’s syndrome may see a diverse range of healthcare practitioners, including family physicians, ophthalmologists, ENT specialists, and dentists, at the first consultation. Thus, it is crucial for physicians of various specialties to be informed about current aspects of clinical manifestations of the disease, the revised classification criteria, and current treatment options.
Pathophysiology
The characteristic lesion of Sjogren syndrome is focal lymphocytic sialadenitis (FLS). FLS is a lesion of exocrine glands. Foci of lymphocyte-rich mononuclear cells infiltrate exocrine glandular tissue adjacent to blood vessels and excretory ducts. The foci are comprised predominantly of T lymphocytes. However, B lymphocytes, plasma cells, and other cell types are seen. With more severe diseases the foci may become confluent. The infiltrating mononuclear cells, humoral factors such as antibodies and cytokines, or both are hypothesized to cause exocrine gland dysfunction resulting in diminished tear production by the lacrimal glands and diminished saliva production by salivary glands. Also, exocrine glands outside the head and neck may be involved resulting in skin, tracheobronchial and vaginal dryness as well as lung and kidney dysfunction. Rarely, malignant transformation of B lymphocytes can result in non-Hodgkin lymphoma. Immune complexes may deposit in skin, joints and other organs resulting in systemic vasculitis.[rx]
Types of Sjogren’s Syndrome
Classification criteria for Sjögren syndrome
American/European classification criteria[rx]
Ocular symptoms (at least one)
- Persistent, troublesome dry eyes every day for longer than three months
- The recurrent sensation of sand or gravel in the eyes
- Use of a tear substitute more than three times per day
Oral symptoms (at least one)
- Feeling of dry mouth every day for at least three months
- The recurrent feeling of swollen salivary glands as an adult
- Need to drink liquids to aid in swallowing dry foods
Objective evidence of dry eyes (at least one)
- Schirmer test ≤ 5 mm/5min
- Van Bijsterveld score ≥ 4 (after lissamine test)
Objective evidence of salivary-gland involvement (at least one)
- Salivary-gland scintigraphy
- Parotid sialography
- Unstimulated salivary flow (≤ 1.5 mL/15 min, ≤ 0.1 mL/min)
Histological features
- A positive biopsy sample of a minor salivary gland (focus score > 1; refers to a cluster of ≥ 50 lymphocytes per lobule when at least four lobules are assessed)
Autoantibodies
-
Presence of antibodies to SSA (Ro/SSA) or to SSB (La/SSB)
Classification
- Primary Sjögren syndrome requires the presence of four of six criteria, including a positive biopsy sample of a minor salivary gland or antibodies against SSA or SSB, or three of the four objective criteria
- Secondary Sjögren syndrome requires an established connective-tissue disease and one sicca symptom plus any three of the four objective criteria
- Exclusions – previous radiotherapy to the head and neck, lymphoma, sarcoidosis, graft-versus-host disease, infection with hepatitis C virus or HIV, or the use of anticholinergic drugs
American College of Rheumatology criteria[rx]
- Antibodies against SSA (Ro/SSA) or SSB (La/SSB), or positive rheumatoid factor and antinuclear antibody levels of 1:320 or greater
- Labial salivary gland biopsy showing focal lymphocytic sialadenitis with a focus score ≥ 1 focus/4 mm2
- Keratoconjunctivitis sicca with ocular staining score ≥ 3 (assumes that the patient is not currently using daily eye drops for glaucoma and has not had corneal surgery or cosmetic eyelid surgery in the last five yr)
- Classification of Sjögren syndrome, which applies to patients with signs or symptoms suggestive of Sjögren syndrome, requires the presence of at least two of the three aforementioned objective features.
- Exclusions history of head and neck radiation treatment, infection with hepatitis C virus, AIDS, sarcoidosis, amyloidosis, graft-versus-host disease or IgG4-related disease
Causes of Sjogren’s Syndrome
The cause of SS is unknown, but it may be the influence of a combination of genetic, environmental, and other factors—as is the case with many other autoimmune disorders.[rx]
- Genetic factors – The observation of high rates of autoimmune disorders in families of SS is linked with a genetic predisposition to the syndrome.[rx] Studies on the polymorphisms of human leukocyte antigen (HLA)-DR and HLA-DQ gene regions in SS patients show differential susceptibility to the syndrome due to different types of the resulting autoantibody production.[rx]
- Hormonal factors – Since SS is associated with a high prevalence in women, sex hormones, especially estrogen, are believed to affect humoral and cell-mediated immune responses affecting susceptibility to the syndrome.[rx] Androgens are generally considered to prevent autoimmunity.[rx] Studies on mice models suggest estrogen deficiency stimulates the presentation of autoantigens, inducing SS-like symptoms.[rx]
- Microchimerism factors – Microchimerism of fetal cells (offspring lymphoid cells in maternal circulation) may generate autoimmunity in women who have been previously pregnant.[rx][rx] Generation of an autoimmune potential via microchimerism may lead to a switch from a silent form of autoimmunity with an age-dependent decrease in self-tolerance.[rx]
- Environmental factors – Viral proteins, engulfed molecules, or degraded self-structures may initiate autoimmunity by molecular mimicry and increase the chances of SS development.[rx] Epstein-Barr virus, hepatitis C, and human T-cell leukemia virus-1 are among the most studied infectious agents in SS.[rx] Damaged self-structures targeted for apoptosis may be mistakenly exposed to the immune system, triggering autoimmunity in exocrine glands, which are often prone to autoimmune responses.[rx]
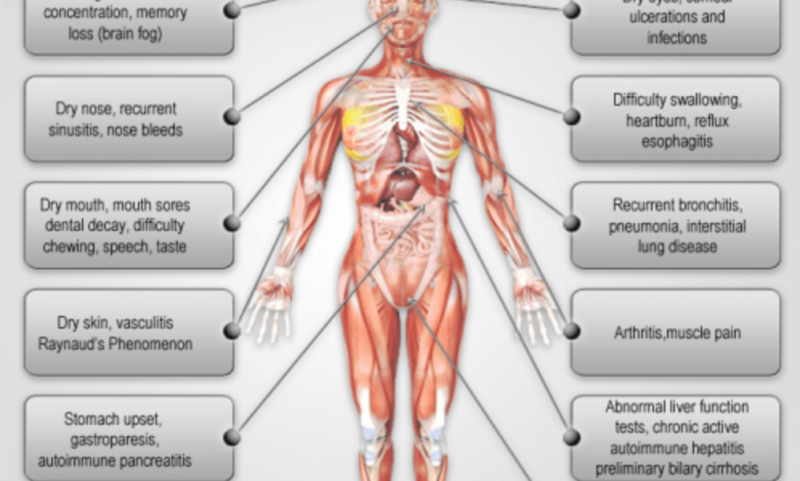
Symptoms of Sjogren’s Syndrome
Revised international classification criteria for Sjögren’s syndrome (American–European Consensus Group, 2002)
I. Ocular symptoms: a positive response to at least one of the following questions:
- Have you had daily, persistent, troublesome dry eyes for more than 3 months?
- Do you have a recurrent sensation of sand or gravel in the eyes?
- Do you use tear substitutes more than three times a day?
II. Oral symptoms: a positive response to at least one of the following questions:
- Have you had a daily feeling of dry mouth for more than 3 months?
- Have you had recurrently or persistently swollen salivary glands as an adult?
- Do you frequently drink liquids to aid in swallowing dry food?
III. Ocular signs – that is, objective evidence of ocular involvement defined as a positive result for at least one of the following two tests:
- Schirmer’s I test, performed without anesthesia (<5 mm in 5 minutes)
- Rose Bengal score or another ocular dye score (>4 according to van Bijsterveld’s scoring system)
IV. Histopathology:
- In minor salivary glands (obtained through normal-appearing mucosa) focal lymphocytic sialoadenitis, evaluated by an expert histopathologist, with a focus score ≥1, defined as a number of lymphocytic foci (which are adjacent to normal-appearing mucous acini and contain more than 50 lymphocytes) per 4 mm2 of glandular tissue.
V. Salivary gland involvement: objective evidence of salivary gland involvement defined by a positive result for at least one of the following diagnostic tests:
- Unstimulated whole salivary flow (≤1.5 mL in 15 minutes)2. Parotid sialography showing the presence of diffuse sialectasias (punctate, cavitary or destructive pattern), without evidence of obstruction in the major ducts3. Salivary scintigraphy showing delayed uptake reduced concentration and/or delayed the excretion of tracer
- Antibodies to SS-A/Ro or SS-B/La antigens, or both
Others
Inflammation of the salivary glands can lead to the following symptoms and signs:
- Mouth dryness,
- Swallowing difficulties,
- Dental decay,
- Cavities,
- Gum disease,
- Mouth sores and swelling,
- Hoarseness or impaired voice,
- Abnormality of taste or loss of taste,
- Dry cough, and
- Stones and/or infection of the parotid gland inside of the cheeks.
- Dry lips often accompany mouth dryness. Dry mouth is a condition medically referred to as xerostomia.
- Other glands that can become inflamed, though less commonly, in Sjögren’s syndrome include those of the lining of the breathing passages (leading to lung infections) and the vagina (sometimes causing a woman pain during intercourse or recurrent vaginal infections).
The signs and symptoms associated with dry eyes include:
- A sensation in one or both eyes similar to the irritation caused by foreign material, such as sand or gravel
- Tired-looking and heavy eyes
- An itchy sensation
- Discharge of mucus from the eyes
- Photophobia, or sensitivity to light
- Stinging or burning eyes
- Swollen and irritated eyelids
- blurred vision
- Smoking, air travel, overhead fans, and air-conditioned or windy environments can exacerbate symptoms.
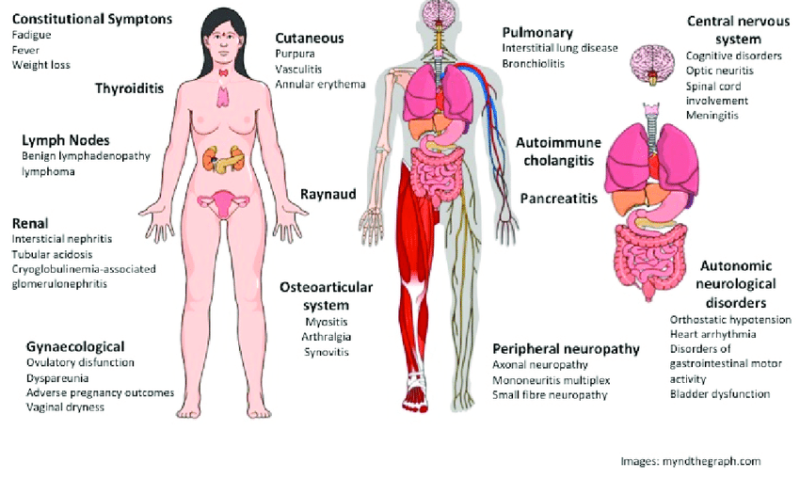
In some cases, the patient’s immune system attacks other parts of the body, causing the following signs and symptoms
- General tiredness
- Brain fog
- Aching muscles
- Inflammation of joints, as well as stiffness and pain
- Peripheral neuropathy, or numbness and occasional pain in the arms or legs
- Lung disease
- Raynaud’s phenomenon, in which the hands feel painful, cold, and numb
- Vasculitis, where the blood vessels become inflamed
Diagnosis of Sjogren’s Syndrome
SS is usually classified as either ‘primary’ or ‘secondary’. Primary Sjögren syndrome occurs by itself and secondary Sjögren syndrome occurs when another connective tissue disease is present.
- Blood tests – can be done to determine if a patient has high levels of antibodies that are indicative of the condition, such as an antinuclear antibody(ANA) and rheumatoid factor (because SS frequently occurs secondary to rheumatoid arthritis), which are associated with autoimmune diseases.
- A spit test – you spit as much saliva as you can into a cup over a five-minute period and the amount is then measured or weighed
- Eye tests – Your doctor can measure the dryness of your eyes with a test called a Schirmer tear test. A small piece of filter paper is placed under your lower eyelid to measure your tear production. A doctor specializing in the treatment of eye disorders (ophthalmologist) might also examine the surface of your eyes with a magnifying device called a slit lamp. He or she may place drops in your eye that make it easier to see damage to your cornea.
- Measuring how many tears you produce – small strips of paper are placed in your lower eyelid for five minutes to see how much of the paper is soaked with tears
- Typical SS ANA patterns – are SSA/Ro and SSB/La of which Anti-SSB/La is far more specific; Anti-SSA/Ro is associated with numerous other autoimmune conditions but is often present in SS. However, Anti-SSA and Anti-SSB tests are frequently not positive in SS.
- The rose bengal test – uses a stain that measures the state and function of the lacrimal glands. This test involves placing the non-toxic dye rose bengal on the eyes. The dye’s distinctive color helps in determining the state and functioning of the tear film and the rate of tear evaporation. Any distinctive color change can indicate SS, but confirming the condition requires many related diagnostic tools.[rx]
- Schirmer’s test measures – the production of tears: a strip of filter paper is held inside the lower eyelid for five minutes, and its wetness is then measured with a ruler. Producing less than 5 mm (0.20 in) of liquid is usually indicative of SS. This measurement analysis varies among people depending on other eye-related conditions and medications in use when the test is taken.[rx] A slit-lamp examination can reveal dryness on the surface of the eye.
- A lip/salivary gland biopsy – takes a tissue sample that can reveal lymphocytes clustered around salivary glands, and damage to these glands due to inflammation. This test involves removing a sample of tissue from a person’s inner lip/salivary gland and examining it under a microscope. In addition, a sialogram, a special X-ray test, is performed to see if any blockage is present in the salivary gland ducts (i.e. parotid duct) and the amount of saliva that flows into the mouth.[rx]
- Radiological procedure – is available as a reliable and accurate test for SS. A contrast agent is injected into the parotid duct, which opens from the cheek into the vestibule of the mouth opposite the neck of the upper second molar tooth.
- Histopathology studies – should show focal lymphocytic sialadenitis. Objective evidence of salivary gland involvement is tested through ultrasound examinations, the level of unstimulated whole salivary flow, a parotid sialography or salivary scintigraphy, and autoantibodies against Ro (SSA) and/or La (SSB) antigens.
Traditional biomarkers[rx]
- Anti-SS-A/Ro, anti-SS-B/La – Not specific for SS; occurs in other autoimmune disorders, particularly SLE.
- Antinuclear antibody (ANA) -Titer ≥1:40 present in approximately two-thirds of SS patients[rx]
- Rheumatoid factor (RF) – Found in many rheumatic conditions but is not unique to SS
Novel biomarkers/autoantibodies[rx]
- Salivary protein-1 (SP-1) – Greatest sensitivity and specificity for early SS
- Carbonic anhydrase VI (CA-6) – Expressed very early in the course of SS; observed rarely in RA or normal controls
- Parotid secretory protein (PSP) – Expressed early in SS; observed rarely in RA or normal controls
Treatment of Sjogren’s Syndrome
Treatment of sicca symptoms involves:
-
Dry eyes – usually respond to artificial tears applied regularly during the day or to gels applied at night. We usually have patients use a preservative-free drop during the day and a preservative-free gel or ointment at night.
-
Punctal occlusion – with plugs or cauterization is frequently needed in more severe cases. Cauterization should only be performed after a trial of plugs to ensure the patient is not left with excessive tearing.
-
Eye drops – that reduce inflammation in the glands around the eyes, such as cyclosporine (Restasis) are used to increase tear production. Many patients are helped by serum tears which are derived from their own blood. Most eye centers now have the capability of making these for the patient.
-
Drinking water – chewing gum, or using saliva substitutes may relieve dry mouth. Some patients benefit from using prescription medications that stimulate saliva flow, such as pilocarpine (Salagen) or cevimeline (Evoxac).
-
If patients develop yeast infections – anti-fungal therapies may be used. Humidifiers and nasal saline irrigation may improve nasal dryness.
-
Medications that reduce gastric acid – (such as proton-pump inhibitors and H2 blockers) may lessen symptoms of acid reflux. Treatments may help relieve some of the dryness, but usually, some dryness persists. The first approach to extra-glandular (systemic) major organ-system disease is oral/parenteral corticosteroids.
-
DMARDs (methotrexate, azathioprine) – have been successfully employed as steroid-sparing agents although none is specifically approved for Sjogren.
-
Hydroxychloroquine – is recommended to treat inflammatory polyarthritis. B cell depletion may have a role in certain severe extra-glandular manifestations (vasculitis). TNF-alpha inhibitors have not proved effective for Sjogren. [rx][rx][rx]
Medications
Depending on your symptoms, your doctor might suggest medications that:
- Decrease eye inflammation – Prescription eye drops such as cyclosporine (Restasis) or lifitegrast (Xiidra) may be recommended by your eye doctor if you have moderate to severe dry eyes.
- Increase production of saliva – Drugs such as pilocarpine (Salagen) and cevimeline (Evoxac) can increase the production of saliva, and sometimes tears. Side effects can include sweating, abdominal pain, flushing, and increased urination.
- Address specific complications – If you develop arthritis symptoms, you might benefit from nonsteroidal anti-inflammatory drugs (NSAIDs) or other arthritis medications. Yeast infections in the mouth should be treated with antifungal medications.
- Treat systemwide symptoms – Hydroxychloroquine (Plaquenil), a drug designed to treat malaria, is often helpful in treating Sjogren’s syndrome. Drugs that suppress the immune system, such as methotrexate (Trexall), also might be prescribed.
Overview of treatment options in primary Sjögren Syndrome.
Some recommended systemic traditional treatment in patients with primary Sjögren’s syndrome.
| Parotid swelling | Short-term oral corticosteroids (D) Antibiotic treatment, if required (D) |
| Arthritis | Hydroxychloroquine (C) NSAIDs Short-term oral/intraarticular corticosteroids (C) Other DMARDs as with rheumatoid arthritis (C) |
| Interstitial lung disease | Corticosteroids, oral or intravenous (C) Cyclophosphamide for active alveolitis (C) Pirfenidone, nintedanib (C) |
| Tubulointerstitial nephritis | Potassium and bicarbonate replacement (D) |
| Glomerulonephritis | Corticosteroids, oral or intravenous (C) Cyclophosphamide Mycophenolate mofetil (according to specific neurologic guidelines) |
| Peripheral neuropathy | Gabapentinoids (D) Corticosteroids IVIg (D) |
| Cryoglobulinemic vasculitis | Corticosteroids, plasmapheresis (C) |
[/dropshadowbox]
- Medications to stimulate saliva flow – These include pilocarpine and cevimeline. They have a short-term impact, limited to a few hours only, so several doses a day are usually required.
- Artificial saliva – Saliva substitutes and mouth-coating gels can relieve dryness of the mouth. They are available as sprays, pre-treated swabs, and liquids. These can be important at night, as the mouth becomes dryer during sleep.
- Artificial tears – Artificial tears can help to lubricate the eyes and are available over-the-counter (OTC). Prescription options are available that reduce the need for artificial tears, such as cyclosporine ophthalmic emulsion and hydroxypropyl cellulose pellets.
- Prescription eye drops – These include cyclosporine and lifitegrast.
- Moisture chamber spectacles – These are special glasses that keep out irritants and retain moisture.
- Prescription expectorants and throat medications – In cases of respiratory dryness, drugs such as those used to stimulate saliva flow, as well as linseed extract, sorbitol, xylitol, or malic acid, can moisturize the area.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – Anti-inflammatory drugs such as aspirin, naproxen, and ibuprofen can provide relief for people with Sjogren’s who are experiencing joint pain.
- Disease-modifying antirheumatic drugs (DMARDs) – In cases where the joint pain is accompanied by fatigue and rashes, DMARDs may relieve symptoms. Examples include hydroxychloroquine or methotrexate. If Sjogren’s seems to be affecting the muscles, nerves, lungs, or kidneys, stronger DMARDs or corticosteroids may be prescribed.
- Antifungal medication – If oral yeast infections are occurring, medication may be prescribed to combat the fungus.
- Vaginal lubricants – For vaginal dryness, water-based vaginal lubricants can provide a solution, especially during sexual intercourse.
- Punctual occlusion – When all conservative treatment options have been exhausted, this surgical option seals the tear ducts with small plugs to reduce the drainage of tears from the eye. This keeps the eye moist for longer. Temporary silicone plugs are likely to be used until the procedure is confirmed successfully.
- Autologous eye serum – In severe cases of eye dryness, eye drops can be made from the person’s blood serum.
Here are some easy ways to keep the mouth lubricated.
- Consuming more liquids.
- Sucking on ice cubes
- Rinsing the mouth regularly to prevent infection and soothe the area
- Maintaining excellent oral and dental hygiene
- Quitting smoking, as smoke irritates the mouth and speeds up the evaporation of saliva
- Chewing sugar-free gum, which stimulates the production of saliva
- Applying coconut oil to the dry areas, as it is both moisturizing and anti-microbial
[dropshadowbox align=”none” effect=”lifted-both” width=”auto” height=”” background_color=”#ffffff” border_width=”1″ border_color=”#dddddd” ]
Selected pathways, biological processes, and molecular functions are represented by differential-expressed genes of the lacrimal and salivary glands during the development and onset of SjS-like disease in C57BL/6.NOD-Aec1Aec2 mice
| Lacrimal Glands | Salivary Glands |
|---|---|
| A. Enriched Pathways | |
| B cell activation | Muscarinic AchR signaling pathway |
| T cell activation | Cell cycle |
| Fas/apoptosis signaling pathway | Angiogenesis |
| Interferon-γ signaling pathway | FGF signaling pathway |
| Integrin signaling pathway | Integrin signaling pathway |
| B. Biological Processes | |
| Apoptosis | Apoptosis |
| Lipid, fatty acid and steroid metabolism | Homeostasis |
| Protein metabolism/targeting/localization | Protein/carbohydrate metabolism |
| Cell cycle | VEGF signaling pathway |
| C. Molecular Functions | |
| Oxidoreductase | Oxidoreductase |
| Membrane traffic protein | Extracellular matrix |
| Kinase | Kinase |
| Transferase | Transferase |
[/dropshadowbox]
References