Amniotic band syndrome is a well-known condition potentially associated with a variety of different birth defects that comprises various congenital anomalies, which include disruption, deformation, and malformations of organs that were intended to develop normally. The abnormalities occur after the affected parts of the body have formed normally in early development. The severity of amniotic band syndrome can range from a single, isolated finding to multiple, disfiguring complications. The arms and legs are most often affected. The head and face and, in some patients, various internal organs can also be affected. The exact cause of amniotic band syndrome is unknown and controversial. Two main theories have been proposed to explain the development of the disorder. One theory attributes the disorder to causes that arise internally within the fetus (intrinsic theory); the other theory attributes the disorder to causes acting upon the fetus externally (extrinsic theory). It is likely that both internal and external factors can cause the amniotic band syndrome, and that the cause of the disorder in one infant may be different from the cause in another infant.
Amniotic band syndrome, also known as constriction ring syndrome, happens when fibrous bands of the amniotic sac (the lining inside the uterus that contains a fetus) get tangled around a developing fetus. In rare cases, the bands wrap around the fetus’ head or umbilical cord.
Synonyms of Amniotic Band Syndrome
ABS has many names amnion rupture sequence, ADAM complex (amniotic deformities/adhesions/mutilations), amniotic band disruption complex, congenital constricting bands, terminal transverse defects, and Streeter anomaly
- ABS
- amnion rupture sequence
- amniotic bands
- amniotic band sequence
- amniotic deformity, adhesions, mutilations (ADAM) complex
- congenital constriction rings
- constriction band syndrome
- limb body wall complex
- Streeter anomaly
- Streeter bands
- Streeter dysplasia
Symptoms
The symptoms associated with amniotic band syndrome vary greatly from one infant to another. Some infants develop only mild deformities; others develop severe and even life-threatening malformations. It seems likely that the features of amniotic band syndrome develop primarily in the first 12 weeks (first trimester) of pregnancy.
Several different patterns have been identified with amniotic band syndrome. The three most common patterns are amniotic band syndrome characterized by one or more limbs being affected; the limb-body-wall complex; and amniotic band syndrome characterized by abnormalities of the head and face (craniofacial abnormalities), defects of the brain, and serious malformation of the arms and legs.
Most infants with amniotic band syndrome have some form of deformity of the arms and legs or fingers and toes. One or more limbs may be affected. Upper limbs are affected more often than lower limbs. In some patients, one limb or one hand or foot may be the only symptom of the disorder. The specific physical features can include abnormally short fingers or toes with the absence of the end (distal) portion, webbing (fusion) of fingers or toes (syndactyly), constriction rings, and extra strands of tissue adhering to the fingers. The constriction rings that encircle a limb or digit can alter blood flow.
Another pattern associated with amniotic band syndrome is referred to as the limb-body wall complex, a lethal condition. Affected infants usually have protrusion of a portion of the brain and its surrounding membranes (meninges) through the skull defect (encephalocele), facial clefts, protrusion of the viscera (the soft internal organs of the body including those found in the abdominal or chest cavities) through a fissure in the abdominal wall (abdominoschisis) or the chest wall (thoracoschisis), and a variety of defects affecting the arms and legs.
A third pattern associated with amniotic band syndrome involves craniofacial abnormalities such as incomplete closure of the roof of the mouth (cleft palate), facial clefts, small, underdeveloped eyes (microphthalmia), narrowing of the nasal passages (choanal atresia), and malformations affecting the size and shape of the skull. In some infants, the head is adherent to the placenta.
Causes
The causes and underlying mechanisms that cause amniotic band syndrome are complex and controversial. Several different theories have been proposed to explain the complex mechanisms that underlie amniotic band syndrome. The two main theories are known as the extrinsic theory and the intrinsic theory. The extrinsic theory states that amniotic band syndrome occurs due to factors found outside of the fetus (externally); the intrinsic theory states that amniotic band syndrome occurs due to factors found within the fetus (internally).
MECHANISMS
Extrinsic Theory
The extrinsic theory for the development of amniotic band syndrome is that strands of tissue separate from the inner layer (amnion) of the amniotic sac. The amniotic sac is the thin membrane that surrounds an embryo or developing fetus (amniotic sac). The sac contains a liquid (amniotic fluid), which supports, cushions, and protects a developing fetus. The amniotic sac is composed of two main layers – the outer layer is called the chorion and the inner layer is called the amnion.
According to this theory, amniotic band syndrome occurs when the inner layer (amnion) of the amniotic sac ruptures or tears, exposing the fetus to strands of fibrous tissue that may float freely in the amniotic fluid or remain partially attached to the amniotic sac. These bands of tissue can disrupt the normal development of a fetus. The bands of tissue can wrap around or entangle (constrict) the fingers, toes, arms, legs, and other parts of the developing fetus as when a rubber band had been tightly wrapped around an arm or leg or another body part. The symptoms that occur due to amniotic bands depend on the specific part of the body affected by these strands of tissue and how tightly they have wrapped around a body part. If the amniotic bands are still partially attached to the amniotic sac, they may wrap around a fetal body part and tether (anchor) that body part to the amniotic sac. This can restrict the movement and proper development of the affected fetus.
Intrinsic Theory
The intrinsic theory was proposed because some researchers noted that, while the above theory explains some cases of amniotic band syndrome, it is insufficient to explain all cases. The external theory fails to explain why there is an intact amniotic sac in some infants with amniotic band syndrome; why there are a high number of malformations affecting internal organs in some patients; and why some infants have defects of parts of the body not affected by amniotic (constriction) bands.
The intrinsic theory attributes the development of amniotic band syndrome to impaired blood flow (circulation) to specific parts of the developing fetus (vascular disruption or compromise). The exact, underlying cause(s) of impaired blood flow is unknown. In areas where the blood flow is poor, injury occurs to the blood vessel walls of the fetus. This leads to bleeding (hemorrhaging) and tissue loss in the affected areas, which in turn results in the varied symptoms associated with the disorder. The intrinsic theory attributes the presence of constriction bands as a secondary effect of the impaired blood flow and subsequent damage to the fetus. In a 1987 article in the journal, Teratology, Webster, et al. demonstrated this theory of vascular disruption with an intact amnion in animal models.
Damage to the amniotic sac has been implicated as a cause of amniotic band syndrome under the extrinsic theory. The exact reason that the amniotic sac tears or ruptures is not always known and researchers believe that in some cases it may happen as a random occurrence.
In some cases, specific environmental factors have been identified. In some infants, trauma to the abdominal area during pregnancy or blunt trauma to the placenta seemed to have caused the amniotic band syndrome.
A few infants have been affected after the performance of a diagnostic technique chorionic villus sampling (CVS) when performed early during pregnancy. The prenatal test was performed to detect certain problems in a fetus such as chromosomal abnormalities or certain genetic disorders. During the procedure, tissue is removed from the placenta and certain cells called chorionic villi are studied. One estimate of the risk for this occasional risk was 1 in 2,000 CVS procedures.
It has also been reported that intense uterine contractions caused by a drug known as misoprostol (a prostaglandin E1 analog) have resulted in amniotic band syndrome. Misoprostol is approved by the Food and Drug Administration for the treatment of gastric ulcers. However, the drug has been used to induce abortion. If the pregnancy continues after the use of misoprostol at 6 to 8 weeks of pregnancy, the infant may have amniotic band syndrome.
The exact cause of impaired fetal blood flow as suggested by the intrinsic theory is unknown. It has been noted, also, that the amniotic band syndrome occurs with greater frequency in first pregnancies, problem pregnancies, or premature births. Young women and women of African descent also have higher rates of infants with amniotic band syndrome. Research is ongoing to determine why certain populations have a greater risk of developing the disorder than other populations.
Some recent genetic studies have begun to identify intrinsic, genetic factors that may predispose infants to the development of amniotic band syndrome (genetic predisposition). A genetic predisposition to developing a disorder means that a person carries a gene, or more likely gene(s), for the disorder, but that the disorder is not expressed unless it is triggered or activated under certain circumstances such as particular environmental factors (multifactorial inheritance).
For example, a genetic predisposition to vascular disruption may contribute to the development of amniotic band syndrome in some cases. Two medical journal articles (Hunter, et al. and Carmichael, et al.) have discussed the possibility that genetic factors influence the development of amniotic band syndrome in certain pregnancies.
Although genetic factors are believed to play a role in the development of infants with some cases of amniotic band syndrome, the risk of recurrence in a subsequent child is extremely low. Most cases of amniotic band syndrome occur sporadically. Current, ongoing research into the potential intrinsic factors associated with amniotic band syndrome should reveal more about the complex causes and development of the disorder.
Diagnosis
Amniotic band syndrome is typically diagnosed at or soon after birth based on characteristic physical findings. The minimal diagnostic criteria consist of the detection of certain abnormalities of the arms, legs, fingers, and/or toes, i.e., ring-like constriction or amputation defects, fusion (syndactyly) between some digits, and/or strands of tissue attached to the ends of affected fingers.
In some cases, the condition may be suspected before birth (prenatally), based upon the results of certain specialized imaging techniques, such as fetal ultrasonography, which may reveal the characteristic defects. During fetal ultrasonography, reflected high-frequency sound waves are used to create an image of the developing fetus.
Clinical presentation can classify into four major categories.
-
Constrictive rings
-
Limb defects
-
Neural or spine defects
-
Craniofacial defects
Constriction rings and limb or digital amputation are the most common findings, present in at least 80 percent of cases. The amniotic bands may be present, confined to the skin or soft tissue, and may extend deep into the tissue. If constriction results in amputation in-utero, then the amputated part is usually resorbed and not visible the following birth.
Limb defects include constriction ring of an extremity with swelling of distal part, absence of distal portions of one or more fingers and toes, especially the central digits, contractures, or fracture. Lower extremities are affected more commonly than the upper, and the thumb is usually spared due to the protection of the palm in-utero.
While atypical, craniofacial abnormalities, such as encephalocele, facial clefts, and cleft lip/cleft palate may be present. Spinal defects and scoliosis have also been known to occur with ABS.
Due to the extensive clinical presentation and heterogeneous etiology, diagnosing amniotic band syndrome could be challenging, especially prenatally. ABS can be suspected prenatally as early as the first trimester if constriction, amputation, or deformation of major anatomic structures are present. Distal limb edema can help make a diagnosis of ABS prenatally. In very few cases, a strand of amniotic fibrous tissue could be seen attached to tissues and restricting the free movement of the fetus in-utero.
Postnatally ABS should be suspected in newborns with visible constrictions, amputations, non-midline, and unusually located craniofacial or body wall defects. Investigation of the fresh fetal membranes and placenta is important in cases where amniotic bands are not visibly present in newborns.
Treatment
The treatment of infants and children with amniotic band syndrome is symptomatic and supportive. For example, in infants with incomplete development of the lungs and associated respiratory insufficiency, treatment may include oxygen support measures and other supportive therapies as required. Reconstructive surgery or other surgical techniques may be recommended to help correct or repair associated malformations, such as ring-like constrictions of the limbs, webbed fingers and toes, cleft lip, or club foot. Physical and occupational therapy may also be necessary to ensure infants can attain the optimal use of affected fingers, toes, arms, and legs.
How is amniotic band syndrome treated?
Treatment is different for every child. Some shallow bands may not interfere with function and may not require surgery. If your child has a deeper amniotic band, they may need one or more surgeries to help fix the way their hand looks and moves.
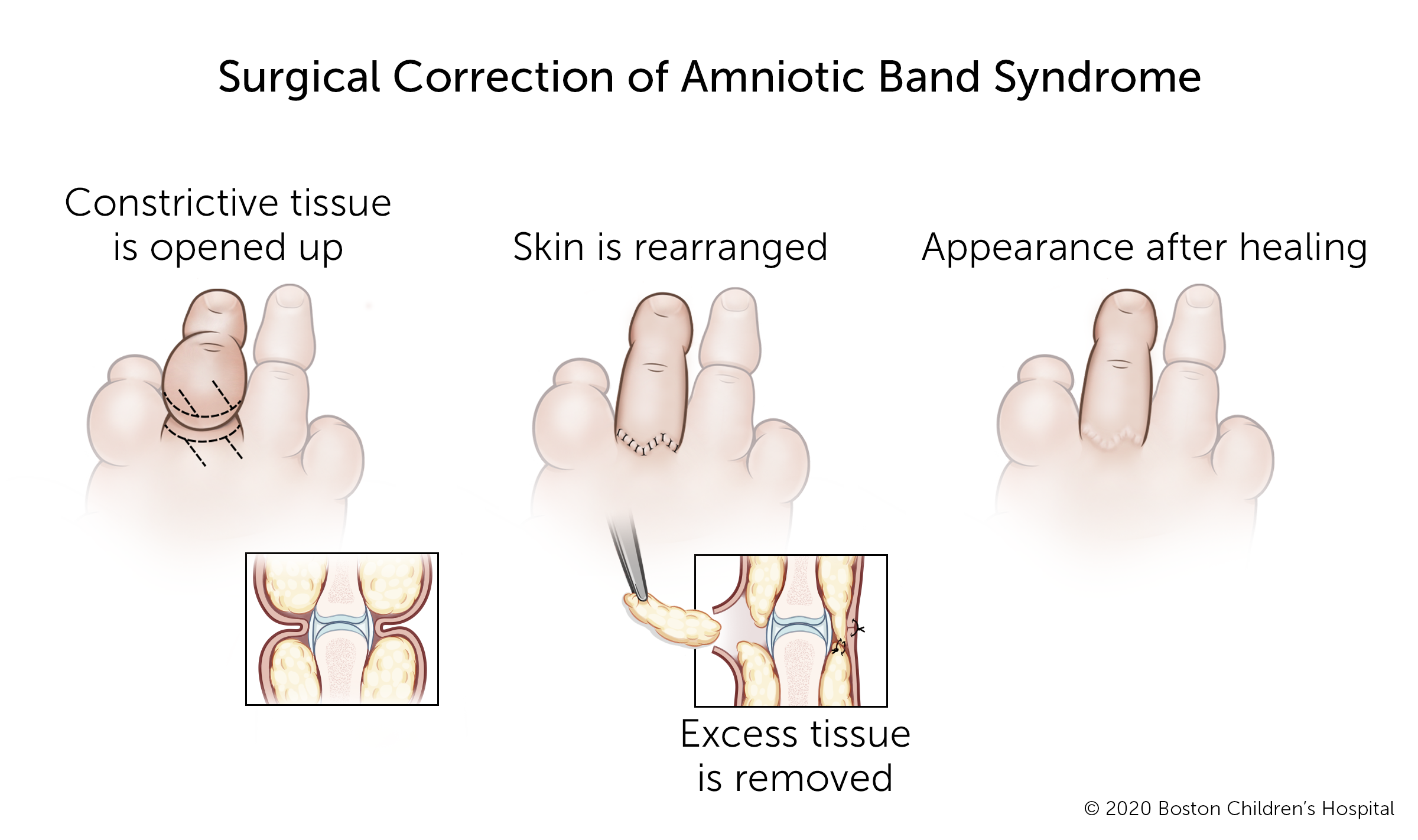
If your child needs surgery, it will probably be done when they are 1 year old or older. But if the constriction is limiting blood flow, they might need surgery right away.
How we care for amniotic band syndrome
The Orthopedic Center’s Hand and Orthopedic Upper Extremity Program and our Department of Plastic and Oral Surgery’s Hand and Reconstructive Microsurgery Program have treated thousands of babies and children with amniotic band syndrome and other hand problems. We are experienced in treating conditions that range from routine to highly complex and can provide your child with expert diagnosis, treatment, and care. We also offer the benefits of some of the most advanced clinical and scientific research in the world.
Our Orthopedic Center is nationally known as the preeminent center for the care of children and young adults with a wide range of developmental, congenital, neuromuscular, sports-related, traumatic, and post-traumatic problems of the musculoskeletal system.
Our Department of Plastic and Oral Surgery is one of the largest and most experienced pediatric plastic and oral surgery centers anywhere in the world. We provide comprehensive care and treatment for a wide variety of congenital and acquired conditions, including hand deformities.
References






