Foot drop is a gait abnormality in which the dropping of the forefoot happens due to weakness, irritation or damage to the common fibular nerve including the sciatic nerve, or paralysis of the muscles in the anterior portion of the lower leg. It is usually a symptom of a greater problem, not a disease in itself.
Foot drop is defined as a weakness of the anterior tibialis and is frequently accompanied by weakness of the extensor hallucis longus and extensor digitorum longus [Rx]. It is usually caused by LMN pathology, commonly disruption of conduction from the deep peroneal nerve (L4-L5). L4-L5 radiculopathy is the most common recognized cause of foot drop, usually caused by herniated nucleus pulposus or foraminal stenosis [rx]. Peripheral peroneal neuropathy is the next most common and is brought on by neurogenic and nonneurogenic causes such as nerve entrapment, diabetes mellitus, inflammatory neuropathy, trauma, masses or pressure near the fibular head, intraneural tumors, and vascular pathology [Rx]. Central or UMN causes are extremely rare but must be considered.
Foot drop is defined as a weak anterior tibialis muscle (on foot extension) and is usually caused by lower motor neuron (LMN) disease. Common causes are L4-L5 radiculopathy, caused by either a herniated nucleus pulposus or foraminal stenosis, and peroneal peripheral neuropathy. Other causes include any axonal or demyelinating damage along the whole peripheral nervous system: conus medullaris, cauda equina, nerve plexus, and peripheral mixed nerve. Central nervous system pathology can also cause foot drop. Foot drop has been reported to occur in 52% to 67% of patients with spinal upper motor neuron (UMN) pathology [rx][Rx]. Central causes tend to occur where nerve fibers are highly condensed along the UMN tracts: interhemispheric motor cortex homunculus (mass lesion, anterior cerebral artery stroke), corona radiata, internal capsule (lacune), cerebral peduncle (lacune), medulla, and spinal cord pyramidal tract (myelopathy).[rx]
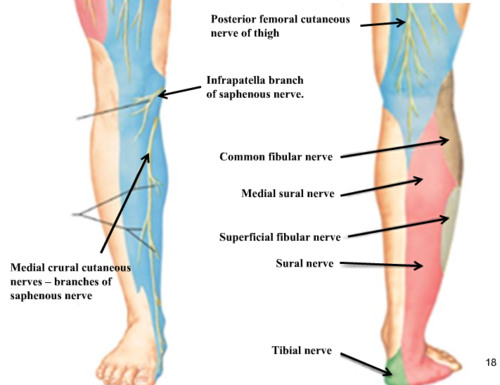
Anatomy of Foot Drop
Fibers from the dorsal branches of the ventral rami of L4-S1 are found in the peroneal nerve, which is paired with the tibial nerve to constitute the sciatic nerve. The sciatic nerve leaves the pelvic cavity at the greater sciatic foramen, just inferior to the piriformis. It bifurcates to form the peroneal and tibial nerves either in the distal third of the thigh or at the midthigh level.
The peroneal nerve crosses laterally to curve over the posterior rim of the fibular neck to the anterior compartment of the lower leg, dividing into superficial and deep branches. The superficial branch travels between the two heads of the peronei and continues down the lower leg to lie between the peroneal tendon and the lateral edge of the gastrocnemius. It then branches to the ankle anterolaterally to supply sensation to the dorsum of the foot .
The deep branch divides just after rounding the fibular neck. Its initial branch supplies the tibialis anterior, and the remaining branches supply the EDL, the EHL, and a small sensory patch at the first dorsal web space .

www.rxharun.com
The peroneal nerve is susceptible to injury all along its course. In that it is part of the sciatic nerve, its funiculi are relatively isolated from those of the tibial nerve. Therefore, trauma to the sciatic nerve may affect only one of its divisions. The funiculi of the peroneal nerve also are larger and have less protective connective tissue than those of the tibial nerve, making the peroneal nerve more susceptible to trauma. In addition, the peroneal nerve has fewer autonomic fibers; thus, in any injury, motor and sensory fibers bear the brunt of the trauma.
Causes of Foot Drop
There are gradations of weakness that can be seen with foot drop, as follows: 0=complete paralysis, 1=flicker of contraction, 2=contraction with gravity eliminated alone, 3=contraction against gravity alone, 4=contraction against gravity and some resistance, and 5=contraction against powerful resistance (normal power). Foot drop is different from foot slap, which is the audible slapping of the foot to the floor with each step that occurs when the foot first hits the floor on each step, although they often are concurrent.
- Neuromuscular disease;
- Peroneal nerve (common, i.e., frequent) —chemical, mechanical, disease;
- Sciatic nerve—direct trauma, iatrogenic;
- Lumbosacral plexus;
- L5 nerve root (common, especially in association with pain in back radiating down leg);
- Cauda equina syndrome, which is cause by impingement of the nerve roots within the spinal canal distal to the end of the spinal cord;
- Spinal cord (rarely causes isolated foot drop) —poliomyelitis, tumor;
- Brain (uncommon, but often overlooked) —stroke, TIA, tumor;
- Genetic (as in Charcot-Marie-Tooth Disease and hereditary neuropathy with liability to pressure palsies);
- Nonorganic causes.
- brain or spinal disorders
- muscle disorders
- A lower back condition
- A stroke or tumor
- Parkinson’s disease
- Diabetes
- Motor neuron disease
- Multiple sclerosis
- Adverse reactions to drugs or alcohol
- An injury to the foot or lower leg
- Motor neuron disorders, e.g. Polio.
- Following surgery (such as knee replacement). This may be due to a haematoma causing compression or irritation of the nerve which is temporary, or nerve damage during surgery.
- Habitual crossing of the legs when sitting – compresses the peroneal nerve.
If the L5 nerve root is involved, the most common cause is a herniated disc. Other causes of foot drop are diabetes (due to generalized peripheral neuropathy), trauma, motor neuron disease (MND), adverse reaction to a drug or alcohol, and multiple sclerosis.
Symptoms of peroneal nerve injury (foot drop)
Symptoms of peroneal nerve injury (foot drop) may include:
- Inability to point toes toward the body (dorsi flexion)
- Pain
- Weakness
- Numbness (on the shin or top of the foot)
- Loss of function of foot
- High-stepping walk (called steppage gait or footdrop gait)
- Pain in the foot.
- Tingling sensation in lower portion of leg.
- Tripping
- Slapping the foot while moving forward.
Diagnosis of Foot Drop
Imaging tests can help pinpoint these types of problems.
- X-rays – Plain X-rays use a low level of radiation to visualize a soft tissue mass or a bone lesion that may be causing your symptoms.
- Ultrasound – This technology uses sound waves to create images of internal structures. It may be used to check for cysts or tumors that may be pressing on the nerve.
- Computerized tomography (CT) scan – Computerized tomography combines X-ray images taken from many different angles to form cross-sectional views of structures within the body.
- Magnetic resonance imaging (MRI) – This test uses radio waves and a strong magnetic field to create detailed images. MRI is particularly useful in visualizing soft tissue lesions that may be compressing a nerve.
- Nerve tests
Electromyography (EMG) and nerve conduction studies measure electrical activity in the muscles and nerves. These tests can be uncomfortable, but they’re very useful in determining the location of the damage along the affected nerve.
Treatment of Foot Drop
In case of severe pain, medications may include:
- Analgesics-Prescription-strength drugs that relieve pain but not inflammation.
- Non-steroidal anti-inflammatory drugs – (NSAIDs – such as aspirin, ibuprofen or naproxen, COX-2 inhibitors (celecoxib)Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include aspirin, ibuprofen (Motrin, Advil), and naproxen (Naprosyn, Aleve).
- Muscle Relaxants– These medications provide relief from spinal muscle spasms, spasticity & increase muscle tone by increaseing blood flood to the cell.
- Neuropathic Agents– Drugs(pregabalin & gabapentine) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opoids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications- These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – to improve bones health and healing fracture.
- Prednisone – 20-30 mg/day with a progressive taper over 7-10 days.
Nonpharmacological treatment for foot drop may include
- Braces or splints. A brace on your ankle and foot or splint that fits into your shoe can help hold your foot in a normal position.
- Physical therapy. Exercises that strengthen your leg muscles and help you maintain the range of motion in your knee and ankle may improve gait problems associated with foot drop. Stretching exercises are particularly important to prevent the development of stiffness in the heel.
- Nerve stimulation. Sometimes stimulating the nerve that lifts the foot improves foot drop.
- Surgery. Depending upon the cause, and if your foot drop is relatively new, nerve surgery may be helpful. If foot drop is long-standing, your doctor may suggest surgery that fuses ankle or foot bones or a procedure that transfers a functioning tendon to a different position.
Exercise
- Physical therapy can help strengthen your muscles, improving your gait (your pattern of walking) and your walking ability. According to Rohrig, your physical therapist will identify whether weakness, spasticity, or both are causing the foot drop, and will then prescribe specific exercises for you. The therapist will also determine how foot drop is impacting your functioning and will investigate whether an assistive device might help you get around better.
Toe-to-Heel Rock
- Osteopathclinic.com says to stand with your hands on a table or the wall for support and rise up on your toes. Hold this position for about 5 seconds then lower your heels and rock back on them so your toes are in the air and you feel a stretch in your calf muscles. Hold this position for 6 seconds then repeat the entire sequence six times.
Toe Co-ordination Test
- Fitness magazine, says to place a few marbles on the floor and try to pick them up with your toes. This will help to improve your dexterity and the strength of the small muscles in your feet.
Strengthen and Stretch
- Sit on the floor with your legs straight out in front of you then flex your foot so your toes move towards your body and your heels lift off the ground.Hold for about 5 seconds then stretch your foot in the opposite direction and curl tour toes under as tightly as you can. Hold for another 5 seconds and repeat the full range of movement as many times as you can.
Rehabilitation Exercises for Foot Drop
- Specific exercises that strengthen the muscles in the foot, ankle and lower leg can help improve the symptoms of foot drop in some cases. Exercises are important for improving range of motion, preventing injury, improving balance and gait, and preventing muscle stiffness.
- When treating foot drop, you may work with a physical therapist who will help you get started strengthening your foot, leg and ankle muscles. Rehabilitation for foot drop can be a slow process, so your physical therapist will likely recommend that you continue to do strengthening exercises at home on your own.
- By being consistent about your exercises at home, you can maximize your chances of making a successful recovery from foot drop. Strengthening the weakened muscles will allow you to restore normal function and hopefully start walking normally again.
- Like any exercise program, please consult your healthcare professional before you begin. Please stop immediately if any of the following exercises cause pain or harm to your body. It’s best to work with a trained professional for guidance and safety.
Towel Stretch

Sit on the floor with both legs straight out in front of you. Loop a towel or exercise band around the affected foot and hold onto the ends with your hands. Pull the towel or band towards your body. Hold for 30 seconds. Then relax for 30 seconds. Repeat 3 times.
Toe to Heel Rocks

Stand in front of a table, chair, wall, or another sturdy object you can hold onto for support. Rock your weight forward and rise up onto your toes. Hold this position for 5 seconds. Next, rock your weight backward onto your heels and lift your toes off the ground. Hold for 5 seconds. Repeat the sequence 6 times.
Marble Pickup

Sit in a chair with both feet flat on the floor. Place 20 marbles and a bowl on the floor in front of you. Using the toes of your affected foot, pick up each marble and place it in the bowl. Repeat until you have picked up all the marbles.
Ankle Dorsiflexion

Sit on the floor with both legs straight out in front of you. Take a resistance band and anchor it to a stable chair or table leg. Wrap the loop of the band around the top of your affected foot. Slowly pull your toes towards you then return to your starting position. Repeat 10 times.
Plantar Flexion

Sit on the floor with both legs straight out in front of you. Take a resistance band and wrap it around the bottom of your foot. Hold both ends in your hands. Slowly point your toes then return to your starting position. Repeat 10 times.
Ball Lift

Sit in a chair with both feet flat on the floor. Place a small round object on the floor in front of you (about the size of a tennis ball). Hold the object between your feet and slowly lift it by extending your legs. Hold for 5 seconds then slowly lower. Repeat 10 times.
How can I manage foot drop myself?
There are some options you can try to help you reduce the risks of trips or falls if you have foot drop, which you can use in conjunction with one of the treatments.
Footwear
- suitable and well fitting footwear can help support your foot and lessen the dragging along the floor
- shoes with laces or with Velcro fastenings that can be adjusted, may be safer than slip-ons that can become loose with wear
- boots can be helpful as they provide ankle support
- avoid cumbersome or heavy shoes that quickly tire your muscles.
Awareness
- be aware of your surroundings when moving about, concentrate and be ALERT: Assess your Location and Environment for the Risk of Trips
- plan your movement, consider which route offers the least potential risk or fewest obstacles. If an obstacle does exist, can this be either safely moved or negotiated?
Remove hazards
- a certain degree of clutter is an inevitable part of day to day life, but try to keep your main routes around the house free from obstacles
- tape down or use non-slip mats under rugs particularly in the bathroom and bedroom, or consider removing them completely
- with electrical items, try to keep wires and cables covered or taped down in walking areas to prevent them being tripped over. An extension lead can help to reroute cables away from places where they might be a tripping hazard.
References