Calcaneus fractures are rare but potentially debilitating injuries. The calcaneus is one of seven tarsal bones and is part of the hind-foot which includes the calcaneus and the talus. The hindfoot articulates with the tibia and fibula creating the ankle joint. The subtalar or calcaneotalar joint accounts for at least some foot and ankle dorsal/plantar flexion. Calcaneal anatomy is demonstrated in Figure 1. Historically a burst fracture of the calcaneus was coined a “Lovers Fracture” as the injury would occur as a suitor would jump off a lover’s balcony to avoid detection. [rx][rx][rx]
Causes of Calcaneus Fractures
Calcaneal fractures are often attributed to shearing stress adjoined with compressive forces combined with a rotary direction (Soeur, 1975[rx]). These forces are typically linked to injuries in which an individual falls from a height, involvement in an automobile accident, or muscular stress where the resulting forces can lead to the trauma of fracture. Overlooked aspects of what can lead to a calcaneal fracture are the roles of osteoporosis and diabetes.
Unfortunately, the prevention of falls and automobile accidents is limited and applies to unique circumstances that should be avoided. The risk of muscular stress fractures can be reduced through stretching and weight-bearing exercise, such as strength training. In addition, footwear can influence forces that may cause a calcaneal fracture and can prevent them as well. A 2012 study conducted by Salzler[rx] showed that the increasing trend toward minimalist footwear or running barefoot can lead to a variety of stress fractures including that of the calcaneus.
Symptoms of Calcaneus Fractures
The most common symptom is pain over the heel area, especially when the heel is palpated or squeezed. Patients usually have a history of recent trauma to the area or fall from a height. Other symptoms include: inability to bear weight over the involved foot, limited mobility of the foot, and limping. Upon inspection, the examiner may notice swelling, redness, and hematomas. A hematoma extending to the sole of the foot is called “Mondor Sign”, and is pathognomonic for calcaneal fracture.[rx][rx] The heel may also become widened with associated edema due to the displacement of lateral calcaneal border. Soft tissue involvement should be evaluated because of the association with serious complications (see below).[rx][rxrx]
Diagnosis ofCalcaneus Fractures
History
Your doctor in the emergency department may ask the following questions
-
How – How was the fracture created, and, if chronic, why is it still open? (underlying etiology)
-
When – How long has this fracture been present? (e.g., chronic less than 1 month or acute, more than 6 months)
- Where – Where on the body parts is it located? Is it in an area that is difficult to offload, complicated, or keep clean? Is it in an area of high skin tension? Is it near any vital organ and structures such as a major artery?
- What is your Past – Has your previous medical history of fracture? Are you suffering from any chronic disease, such as hypertension, blood pressure, diabetes mellitus, previous major surgery? What kind of medicine did you take? What is your food habits, geographic location, Alcohol, tea, coffee consumption habit, anabolic steroid uses for athletes, etc?
Physical
Physical examination is done by your doctor, consisting of palpation of the fracture site, eliciting boney tenderness, edema, swelling. If the fracture is in the dept of a joint, the joint motion, normal movement will aggravate the pain.
- Inspection – Your doctor also check superficial tissue, skin color, involving or not only the epidermal layer or Partial-thickness affects the epidermis and extend into the dermis, but full-thickness also extends through the dermis and into the adipose tissues or full-thickness extends through the dermis, and adipose exposes muscle, bone, evaluate and measure the depth, length, and width of the fracture. Access surrounding skin tissue, fracture margins for tunneling, rolled, undermining fibrotic changes, and if unattached and evaluate for signs and symptoms of infect warm, pain, delayed healing.
- Palpation – Physical examination may reveal tenderness to palpation, swelling, edema, tenderness, worm, temperature, open fracture, closed fracture, microtrauma, and ecchymosis at the site of fracture.
- Motor function – Your doctor may ask the patient to move the injured area to assist in assessing muscle, ligament, and tendon function. The ability to move the joint means only that the muscles and tendons work properly, and does not guarantee bone integrity or stability. The concept that “it can’t be fractured because you can move it” is not correct. The jerk test and manual test are also performed to investigate the motor function.
- Sensory examination – assesses sensations such as light touch, worm, paresthesia, itching, numbness, and pinprick sensations, in its fracture side.
- Range of motion – A range of motion examination of the fracture associate joint and it’s surrounding joint may be helpful in assessing the muscle, tendon, ligament, cartilage stability. Active assisted, actively resisted exercises are performed around the injured area joint.
- Blood pressure and pulse check – Blood pressure is the term used to describe the strength of blood with which your blood pushes on the sides of your arteries as it’s pumped around your body. An examination of the circulatory system, feeling for pulses, blood pressure, and assessing how quickly blood returns to the tip of a toe to heart and it is pressed the toe turns white (capillary refill).
Lab Test
Laboratory tests should be done as an adjunct in overall medical status for surgical treatment.
- CBC, ESR test
- Random blood sugar, glucose, and routine diabetes test if the patient has diabetes mellitus.
- Microscopic urine examination test, and stool test.
- ECG, EKG test for heart abnormality is present
- Ultrasonography test in some cases.
- Normalized hemoglobin, hematocrit test
- Coagulation profile with bleeding time and coagulation time test, prothrombin time (PT) test for surgery if needed,
- Partial thromboplastin time (PTT), and platelet counts will be needed for operative intervention.
- Serum creatinine test,
- Serum lipid profile
- Serum uric acid test
Evaluation of a potential calcaneus fracture should include the following:
-
Complete neurovascular examination as well as evaluation of all lower extremity tendon function. Loss of ipsilateral dorsalis pedis or posterior tibial pulse compared to contralateral limb should raise suspicion of arterial injury and prompt further investigation with angiography or Doppler scanning.
-
Initial bony evaluation with AP, lateral, and oblique plain films of the foot and ankle is needed. A Harris View may be obtained which demonstrates the calcaneus in an axial orientation.
-
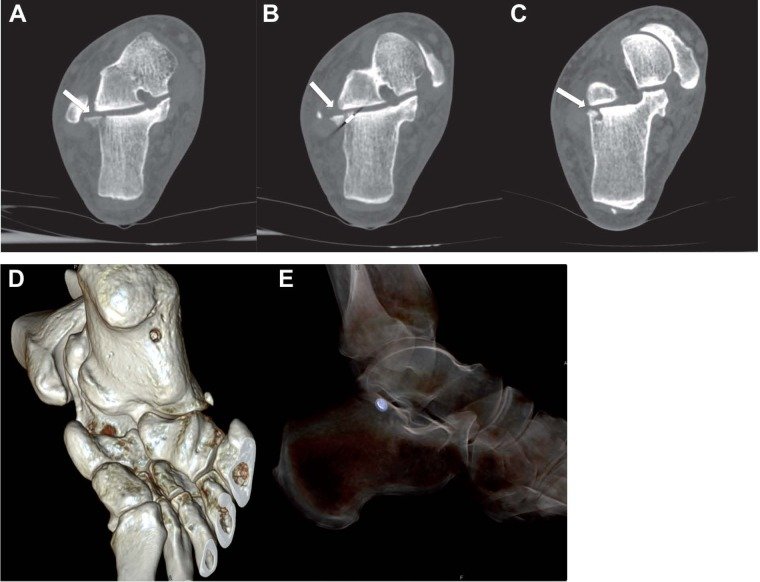
Noncontrast computed tomography remains the gold standard for traumatic calcaneal injuries. CT scan is used for preoperative planning, classification of fracture severity, and in instances where the index of suspicion for a calcaneal fracture is high despite negative initial plain radiographs.
-
Mondor’s Sign is a hematoma identified on CT that extends along the sole and is considered pathognomic for calcaneal fracture.
-
Stress fractures such as those seen in runners would be best evaluated with a bone scan or MRI.
-
Bohler’s Angle may be depressed on plain radiographs. Defined as the angle between two lines drawn on plain film. The first line is between the highest point on the tuberosity and the highest point of the posterior facet and the second is the highest point on the anterior process and the highest point on the posterior facet. The normal angle is between 20-40 degrees.
-
The Critical Angle of Gissane may be increased. Defined as the angle between two lines drawn on plain film. The first along the anterior downward slope of the calcaneus and the second along the superior upward slope. A normal angle is 130-145 degrees.
-
Normal Bohlers and Gissane angles do not rule out a fracture.
-
Abnormalities of either of these findings should prompt a CT scan for further classification and evaluation of the fracture.
Calcaneal fractures can be classified into two general categories.[rx][rx]
-
Extraarticular fractures account for 25 % of calcaneal fractures. These typically are avulsion injuries of either the calcaneal tuberosity from the Achilles tendon, the anterior process from the bifurcate ligament, or the sustenaculum tali.
-
Intraarticular Fractures account for the remaining 75%. The talus acts as a hammer or wedge compressing the calcaneus at the angle of Gissane causing the fracture.
There are two main classification systems of extraarticular fractures.
Essex-Lopresti:
-
Joint depression type with a single verticle fracture line through the angle of Gissane separating the anterior and posterior portions of the calcaneus.
-
Tongue type which has the same verticle fracture line as a depression type with another horizontal fracture line running posteriorly, creating a superior posterior fragment.
Sanders Classification: Based on reconstituted CT findings.
-
Type I fractures: 1 nondisplaced or minimally displaced bony fragment
-
Type II fractures: 2 bony fragments involving the posterior facet. Subdivided into types A, B, and C depending on the medial or lateral location of the fracture line.
-
Type III fractures: 3 bony fragments including an additional depressed middle fragment. Subdivided into types AB, AC, and BC, depending on the position and location of the fracture lines.
-
Type IV fractures: 4 comminuted bony fragments.
Treatment of Calcaneus Fractures
Do no HARM for 72 hours after injury
- Heat—hot baths, electric heat, saunas, heat packs, etc has the opposite effect on the blood flow. Heat may cause more fluid accumulation in the fracture joints by encouraging blood flow. Heat should be avoided when inflammation is developing in the acute stage. However, after about 72 hours, no further inflammation is likely to develop and heat can be soothing.
- Alcohol stimulates the central nervous system that can increase bleeding and swelling and decrease healing.
- Running, and walking may cause further damage, and causes healing delay.
- Massage also may increase bleeding and swelling. However, after 72 hours of your fracture, you can take a simple message, and applying heat may be soothing the pain.
Medication
The following medications may be considered by your doctor to relieve acute and immediate pain, long term treatment
- Antibiotic – Cefuroxime or Azithromycin, or Flucloxacillin or any other cephalosporin/quinolone, meropenem antibiotic must be used to prevent infection or clotted blood removal to prevent further swelling, inflammation, and edema.
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include first choice NSAIDs is Ketorolac, then Etoricoxib, then Aceclofenac, naproxen.
- Muscle Relaxants – These medications provide relief from spinal muscle spasms, spasticity. Muscle relaxants, such as baclofen, tolperisone, eperisone, methocarbamol, carisoprodol, and cyclobenzaprine, may be prescribed to control postoperative muscle spasms, spasticity, stiffness, contracture.
- Calcium & vitamin D3 – To improve bone health, blood clotting, helping muscles to contract, regulating heart rhythms, nerve functions, and healing fractures. As a general rule, too absorbed more minerals for men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day to heal back pain, fractures, osteoarthritis.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, tingling sensation, and paresthesia.
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tighten the loose tendon, cartilage, ligament, and cartilage, ligament regenerates cartilage or inhabits the further degeneration of cartilage, ligament. The dosage of glucosamine is 15oo mg per day in divided dosage and chondroitin sulfate approximately 500mg per day in different dosages, and diacerein minimum of 50 mg per day may be taken if the patient suffers from osteoarthritis, rheumatoid arthritis, and any degenerative joint disease.[rx]
- Topical Medications and essential oil – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation in acute trauma, pain, swelling, tenderness through the skin. If the fracture is closed and not open fracture then you can use this item.
- Antidepressants – A drug that blocks pain messages from your brain and boosts the effects of endorphins in your body’s natural painkillers. It also helps in neuropathic pain, anxiety, tension, and proper sleep.
- Corticosteroids – Also known as oral steroids, these medications reduce inflammation. To heal the nerve inflammation and clotted blood in the joints.
- Dietary supplement – To eradicate the healing process from fracture your body needs a huge amount of vitamin C, and vitamin E. From your dietary supplement, you can get it, and also need to remove general weaknesses & improved health.
- Cough Syrup – If your doctor finds any chest congestion or fracture-related injury in your chest, dyspnoea, post-surgical breathing problem, then advice you to take bronchodilator cough syrup.
What To Eat and What to avoid
Eat Nutritiously During Your Recovery
All bones and tissues in the body need certain micronutrients in order to heal properly and in a timely manner. Eating a nutritious and balanced diet that includes lots of minerals and vitamins is proven to help heal broken bones and all types of fractures. Therefore, focus on eating lots of fresh food produce (fruits and veggies), whole grains, cereal, beans, lean meats, seafood, and fish to give your body the building blocks needed to properly repair your fracture. In addition, drink plenty of purified mineral water, milk, and other dairy-based beverages to augment what you eat.
- Broken bones or fractures bones need ample minerals (calcium, phosphorus, magnesium, boron, selenium, omega-3) and protein to become strong and healthy again.
- Excellent sources of minerals/protein include dairy products, tofu, beans, broccoli, nuts and seeds, sardines, sea fish, and salmon.
- Important vitamins that are needed for bone healing include vitamin C (needed to make collagen that your body essential element), vitamin D (crucial for mineral absorption, or machine for mineral absorber from your food), and vitamin K (binds calcium to bones and triggers more quickly collagen formation).
- Conversely, don’t consume food or drink that is known to impair bone/tissue healing, such as alcoholic beverages, sodas, fried fast food, most fast food items, and foods made with lots of refined sugars and preservatives.
Open fractures require more urgent surgical treatment and wound care.
Closed fracture reduction can be delayed.
-
All surgical treatment is aimed at restoration of heel height and width (i.e., reconstructing the anatomy to reapproximate Bohler and Gissane angles), repair and realignment of the subtalar joint, and returning the mechanical axis of the hindfoot to functionality.
-
Most extraarticular fractures are treated conservatively with 10-12 weeks of casting.
-
Calcaneal tuberosity avulsion, displaced sustenaculum tali, and large substantial calcaneal body fractures may require operative management.
-
Some intraarticular injuries may be treated in a closed fashion depending upon severity. Many are treated with either open surgical reduction and internal fixation, percutaneous pinning, or sometimes arthrodesis.
-
Nondisplaced Sanders type I fractures may be treated in a conservative, closed fashion.







