Pendred syndrome is a genetic disorder that causes early hearing loss in children. It also can affect the thyroid gland and sometimes creates problems with balance. The syndrome is named after Vaughan Pendred, the physician who first described people with the disorder.
Children who are born with Pendred syndrome may begin to lose their hearing at birth or by the time they are three years old. Usually, their hearing will worsen over time. The loss of hearing often happens suddenly, although some individuals will later regain some hearing. Eventually, some children with Pendred syndrome become deaf.
Almost all children with Pendred syndrome have bilateral hearing loss, which means a hearing loss in both ears, although one ear may have more hearing loss than the other.
Childhood hearing loss has many causes. Researchers believe that in the United States 50 to 60 percent of cases are due to genetic causes, and 40 to 50 percent of cases result from environmental causes. Healthcare professionals use different clues, such as when the hearing loss begins and whether there are anatomical differences in the ears, to help determine whether a child has Pendred syndrome or some other type of progressive deafness.
How does Pendred syndrome affect other parts of the body?
Pendred syndrome can make the thyroid gland grow larger. An enlarged thyroid gland is called a goiter. The thyroid is a small, butterfly-shaped gland in the front of the neck, just above the collarbones. The thyroid plays a major role in how the body uses energy from food. In children, the thyroid is important for normal growth and development. Children with Pendred syndrome, however, rarely have problems growing and developing properly even if their thyroid is affected. Their levels of thyroid hormones are usually normal.
People with Pendred syndrome are significantly more likely than the general population to develop a goiter in their lifetime, although not everyone who has Pendred syndrome gets a goiter. The typical age for a goiter to develop in adolescence or early adulthood. If a goiter becomes large, there may be problems with breathing and swallowing. In this case, a health professional should check the goiter and decide whether treatment is necessary. People with Pendred syndrome may need to visit an endocrinologist, who is a specially trained doctor familiar with diseases and disorders that involve the endocrine system, including the thyroid gland.
Pendred syndrome also can affect the vestibular system, which controls balance. Some people with Pendred syndrome will show vestibular weakness when their balance is tested. However, the brain is very good at making up for a weak vestibular system, and most children and adults with Pendred syndrome don’t have a problem with their balance or have difficulty doing routine tasks. Some babies with Pendred syndrome may start walking later than other babies, however.
Scientists don’t know why some people with Pendred syndrome develop goiter or have balance problems and others don’t.
What causes Pendred syndrome?
Pendred syndrome can be caused by changes, or mutations, in a gene called SLC26A4 (formerly known as the PDS gene) on chromosome 7. Because it is a recessive trait, a child needs to inherit two mutated SLC26A4 genes—one from each parent—to have Pendred syndrome. Since the child’s parents are only carriers of a mutation in the SLC26A4 gene, there are no health implications for them.
Couples who are concerned that they could pass Pendred syndrome to their children might want to seek genetic testing. A possible sign that someone might be a carrier of a mutated SLC26A4 gene is a family history of early hearing loss. Another sign is a family member who has both a goiter and hearing loss. However, often there is no family history of Pendred syndrome in the families of children who have the disorder. A mutation in the SLC26A4 gene can be determined by genetic testing of a blood sample.
The decision to have a genetic test is complicated. Most people talk with a genetic counselor trained to help them weigh the medical, emotional, and ethical considerations of testing. A genetic counselor is a health professional who provides information and support to people (and their families) who have a genetic disorder or who are at risk for a genetic disorder.
Pendred syndrome occurs due to mutation in The Pendrin Gene (PDS/SLC26A4), which encodes Pendrin/SLC26A4 Protein.[rx] SLC26A4 is on chromosome 7q22.3, and it expresses in multiple organs, including the inner ear, kidneys, thyroid, and bronchial epithelial cells.[rx][rx] It is a multifunctional anion exchanger that has an affinity to chloride, iodide, bicarbonate, and other anions.[rx]
The differential diagnosis includes other causes of sensorineural hearing loss and thyroid disease.
-
Nonsyndromic causes of congenital deafness such as congenital infections example CMV, exposure to autotoxic agents, or trauma
-
Nonsyndromic enlarged vestibular aqueduct without associated thyroid goiter[rx]
-
Congenital hypothyroidism with hearing impairment[rx]
Other causes of syndromic deafness examples:
-
Branchiootorenal (BOR) syndrome, branchial cyst, hearing impairment, and renal involvement[rx]
-
Waardenburg syndrome is associated with pigmentation of hair and skin[rx]
-
Usher syndrome is associated with retinitis pigmentosa[rx]
-
Alport syndrome with hearing impairment, with renal and ocular involvement[rx]
-
Jervell and Lange-Nielsen and its association with arrhythmia [rx]
-
Perrault syndrome is characterized by progressive sensorineural hearing loss associated with ovarian involvement in females.[rx]
How is Pendred syndrome diagnosed?
An otolaryngologist (a doctor who specializes in diseases of the ear, nose, throat, head, and neck) or a clinical geneticist will consider hearing loss, inner ear structures, and sometimes the thyroid in diagnosing Pendred syndrome. He or she will evaluate the timing, amount, and pattern of hearing loss and ask questions such as “When did the hearing loss start?”, “Has it worsened over time?”, and “Did it happen suddenly or in stages?” Early hearing loss is one of the most common characteristics of Pendred syndrome; however, this symptom alone doesn’t mean a child has the condition.
History and Physical
Hearing Impairment: Pendred syndrome patients have sensorineural hearing loss that is broad and can range from mild to profound.[rx] Hearing impairment typically is congenital or prelingual and profound. It can also develop later in infancy with progressive worsening, which may be aggravated by exposure to acoustic traumas, barotraumas, or head injury.[rx][rx] Hearing impairment is usually bilateral, although asymmetry can be present. Early signs include the absence of a reaction to sound or a delay in language acquisition.
Vestibular manifestations are usually not obvious but may be noticed during progressive hearing loss periods or in performances needing motor skills and balance.[rx] Some patients may show features of temporal bone abnormalities.[rx]
Thyroid: Euthyroid goiter is the typical presentation of Pendred syndrome.[rx] Enlargement of the thyroid gland occurs because of iodide organification defects. It may also present with multinodular goiter in late childhood or early puberty.[rx] Some may develop thyroid goiter during their adult life. Approximately 75% of patients with Pendred syndrome have a goiter on physical examination.[rx] While the majority of patients present with congenital goiter,[rx] the rest can have normal size glands, especially if they have adequate iodine intake.[rx][rx][rx]
Since Iodide organification is not solely dependent on pendrin, patients usually have partial iodide organification defects.[7] While 50 % of patients will have normal thyroid function, others have subclinical hypothyroidism, which can be congenital.[rx]
Renal System: Patients with Pendred syndrome might develop life-threatening metabolic alkalosis due to acid-base balance abnormalities.[rx]
Genetic testing:
Molecular genetic testing is a confirmatory test and should be performed to confirm the diagnosis.[rx] The SLC26A4 gene is the most affected, and 50 % of Pendred syndrome patients have a mutation in this gene. Genetic testing is done by direct sequencing of the coding region of the SLC26A4 gene [rx] By identifying the biallelic pathogenic variant in the gene or the presence of double heterozygous for one pathogenic variant.[rx] FOXII and KCNJI0 gene mutations are affected in less than 2% of patients.[rx][rx] Because of the diverse mutations in the SLC26A4 gene, researchers have identified approximately 200 sequence variants.[rx] Efforts should be made to recognize the full range of presentation of the syndrome to narrow down the suspected cases before performing the molecular studies, taking into account the more specific clinical criteria.[rx]
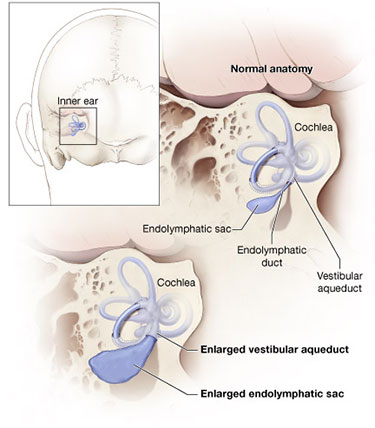
The specialist will use inner ear imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT scan) to look for two characteristics of Pendred syndrome. One characteristic might be a cochlea with too few turns. The cochlea is the spiral-shaped part of the inner ear that converts sound into electrical signals that are sent to the brain. A healthy cochlea has two-and-a-half turns, but the cochlea of a person with Pendred syndrome may have only one-and-a-half turns. Not everyone with Pendred syndrome, however, has an abnormal cochlea.
Temporal Bone Findings:
Affected individuals have temporal bone abnormalities, which can be identified by thin-cut CT with detailed cochlear anatomy.
The enlarged vestibular aqueduct is measurable by high-resolution CT of the temporal bone with coronal and axial sections. Confirmation of vestibular aqueduct enlargement is if the width of the middle portion of the descending limb of the vestibular aqueduct is over 1.5 mm.[rx][rx] Patients also can have cochlear hypoplasia when the cochlea has 1.5 turns instead of the normal 2.75 turns. If a patient has vestibular aqueduct enlargement associated with cochlear hypoplasia, it is referred to as Mondini malformation.[rx][rx]
Thyroid Findings: Euthyroid goiter is the typical thyroid abnormality in Pendred syndrome, and it is detected by volumetric studies to assess the size of the gland, thyroid ultrasound helps to evaluate the volume of the thyroid gland and characterize the size and structure of the nodules.[rx][rx] If the Pendred syndrome diagnosis is confirmed, thyroid function tests should take place regularly. Pendred syndrome can also coexist with autoimmune thyroiditis.[rx]
Perchlorate test is a screening test for iodide organification defects done by administering radioactive iodine and measuring the intrathyroidal radioactive iodine content. If it is less than 10%, it suggests an organification defect. However, a negative test does not rule out the diagnosis of Pendred syndrome because multiple factors can affect the results. One of the factors is the previous use of high-dose iodine intake, which can interfere with the testing.[rx][rx]
The second characteristic of Pendred syndrome is an enlarged vestibular aqueduct (see figure). The vestibular aqueduct is a bony canal that runs from the vestibule (a part of the inner ear between the cochlea and the semicircular canals) to the inside of the skull. Inside the vestibular aqueduct is a fluid-filled tube called the endolymphatic duct, which ends at the balloon-shaped endolymphatic sac. The endolymphatic duct and sac usually are also enlarged.
Experts don’t recommend testing thyroid hormone levels in children with Pendred syndrome, since levels are usually normal. Some children might be given a “perchlorate washout test,” a test that determines whether the thyroid is functioning properly. Although this test is probably the best test for determining thyroid function in Pendred syndrome, it isn’t used often and has largely been replaced by genetic testing. People who have developed a goiter may be referred to an endocrinologist, a doctor who specializes in glandular disorders, to determine whether the goiter is due to Pendred syndrome or another cause. Goiter is a common feature of Pendred syndrome, but many individuals who develop a goiter don’t have Pendred syndrome. Conversely, many people who have Pendred syndrome never develop a goiter.
Can Pendred syndrome be treated?
Treatment options for Pendred syndrome are available. Because the syndrome is inherited and can involve thyroid and balance problems, many specialists may be involved in treatment, including a primary care physician, an audiologist, an endocrinologist, a clinical geneticist, a genetic counselor, an otolaryngologist, and a speech-language pathologist.
-
There is no definite management for Pendred syndrome.
-
The treatment basis is from clinical manifestations. Patients with Pendred syndrome need to follow up with a multidisciplinary team, including ENT, endocrinology, genetics, and surgery.
-
Monitoring thyroid function and thyroid gland size, which might need medical or surgical intervention.[rx]
-
The importance of genetic counseling for the family and testing family members and discussion about offspring outcome.[rx]
To reduce the likelihood of hearing loss progression, children and adults with Pendred syndrome should avoid contact sports that might lead to head injury; wear head protection when engaged in activities such as bicycle riding and skiing that might lead to head injury; and avoid situations that can lead to barotrauma (extreme, rapid changes in pressure), such as scuba diving or hyperbaric oxygen treatment.
Pendred syndrome isn’t curable, but a medical team will work together to encourage informed choices about treatment options. They also can help people prepare for increased hearing loss and other possible long-term consequences of the syndrome.
Children with Pendred syndrome should start early treatment to gain communication skills, such as learning sign language or cued speech, or learning to use a hearing aid. Most people with Pendred syndrome will have hearing loss significant enough to be considered eligible for a cochlear implant. A cochlear implant is an electronic device that is surgically inserted into the cochlea. While a cochlear implant doesn’t restore or create normal hearing, it bypasses injured areas of the ear to provide a sense of hearing in the brain. Children as well as adults are eligible to receive an implant.
People with Pendred syndrome who develop a goiter need to have it checked regularly. The type of goiter found in Pendred syndrome is unusual because even though it grows in size, it continues to make normal amounts of thyroid hormone. Such a goiter often is called a euthyroid goiter.
References







