Otosclerosis is a term derived from oto, meaning “of the ear,” and sclerosis, meaning “abnormal hardening of body tissue.” The condition is caused by abnormal bone remodeling in the middle ear. Bone remodeling is a lifelong process in which bone tissue renews itself by replacing old tissue with new. In otosclerosis, abnormal remodeling disrupts the ability of sound to travel from the middle ear to the inner ear. Otosclerosis affects more than three million Americans. Many cases of otosclerosis are thought to be inherited. White, middle-aged women are most at risk.
Otosclerosis (oto, “of the ear,” and sclerosis, “abnormal hardening of body tissue”), also known as otospongiosis, is an abnormal bone remodeling in the middle ear. The normal dense endochondral layer of the bony otic capsule in the labyrinth is replaced by irregularly laid spongy bone leading to the fixation of the stapes.[rx] Otosclerosis commonly causes conductive deafness presenting with a normal tympanic membrane. Furthermore, depending upon the foci of involvement on the bony labyrinth, otosclerosis can be asymptomatic or can present as a neurosensory loss. Nevertheless, otosclerosis has an effect on the functioning of the middle and the inner ear.
How do we hear?
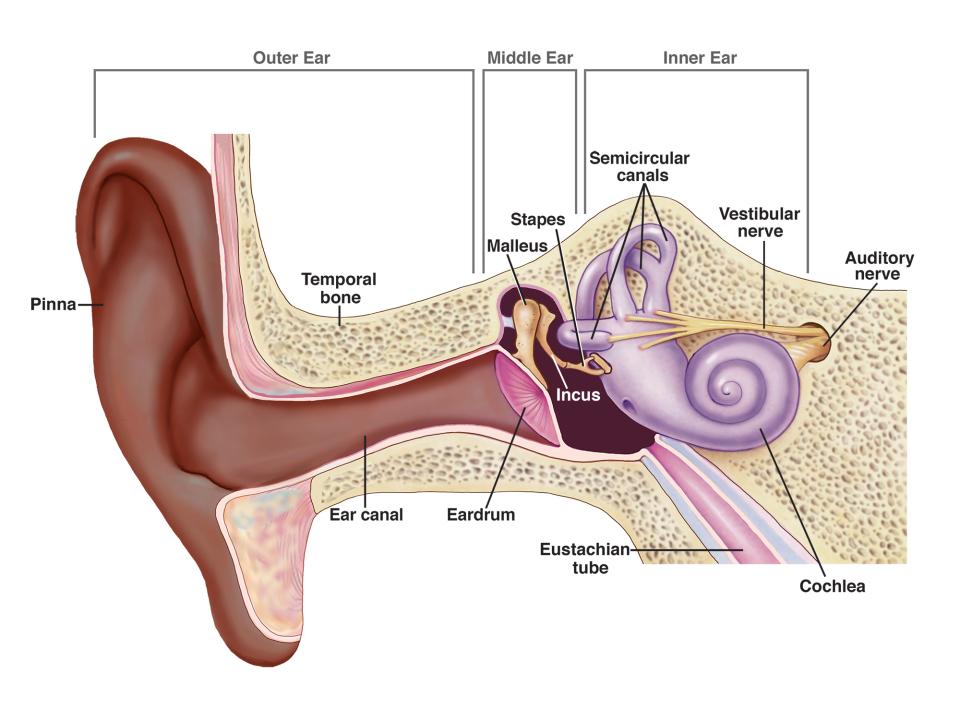
Healthy hearing relies on a series of events that change sound waves in the air into electrochemical signals within the ear. The auditory nerve then carries these signals to the brain.
First, sound waves enter the outer ear and travel through a narrow passageway called the ear canal, which leads to the eardrum.
The incoming sound waves make the eardrum vibrate, and the vibrations travel to three tiny bones in the middle ear called the malleus, incus, and stapes—the Latin names for hammer, anvil, and stirrup.
The middle-ear bones amplify the sound vibrations and send them to the cochlea, a fluid-filled structure shaped like a snail, in the inner ear. The upper and lower parts of the cochlea are separated by an elastic, “basilar” membrane that serves as the base, or ground floor, upon which key hearing structures sit.
Incoming sound vibrations cause the fluid inside the cochlea to ripple, and a traveling wave forms along the basilar membrane. Hair cells that sit on top of the membrane “ride” this wave and move up and down with it.
The bristly structures of the hair cells then bump up against an overlying membrane, which causes the bristles to tilt to one side and open pore-like channels. Certain chemicals then rush in, creating an electrical signal that is carried by the auditory nerve to the brain. The result is a recognizable sound.
Hair cells near the base of the cochlea detect higher-pitched sounds, such as a cell phone ringing. Those nearer the middle detect lower-pitched sounds, such as a large dog barking.
What causes otosclerosis?
Otosclerosis is most often caused when one of the bones in the middle ear, the stapes, become stuck in place. When this bone is unable to vibrate, the sound is unable to travel through the ear and hearing becomes impaired (see illustration).
Why this happens is still unclear, but scientists think it could be related to previous measles infection, stress fractures to the bony tissue surrounding the inner ear, or immune disorders. Otosclerosis also tends to run in families.
The exact etiology of otosclerosis is still unclear. The multiple etiologies that have been postulated include:
Anatomical: The most commonly affected part seems to be the fissula ante fenestram, where the remnants of the embryonic cartilage persist.[2]
Genetic: Many loci on chromosomes 6p, 9p, 1q, 3q, 6q, 7q, 15q, and 16q have been identified. In an open genome-wide analysis, a new locus on chromosome 7q22.1 has also been found. Besides, different genes that are involved including type I collagen (COL1A1 gene), TGF-beta 1 (BMP 2 and BMP 4 genes), angiotensin II (AGT M235T and ACE I/D genes), sex hormones, autoimmune reaction, human leucocyte antigen, inflammatory and regulatory cytokines, parathyroid hormone and expression of parathyroid hormone-related peptides receptors, and oxidative stress have also been regarded as causes of otosclerosis.[rx][rx][rx]
Hereditary: In more than half of the patients presenting with otosclerosis, there is a positive family history. Also, patients with a positive family history have an earlier onset of otosclerosis. Genetic studies show that an autosomal dominant mode of inheritance with reduced penetrance (40%) and a variable expressivity is found in most of the cases.[rx][rx]
Sex: The prevalence of otosclerosis is more in women compared to men suggesting the role of sex hormones.[rx]
Ethnicity: Otosclerosis is more common in Whites. However, it is rarer in the Black population.[rx][rx]
Age: Hearing loss is more commonly seen between the second and the third decade.[rx]
Pregnancy: Pregnancy does worsen deafness in osteosclerosis; however, the relationship of pregnancy with otosclerosis is still controversial.[rx]
Viral Infections: The role of measles virus infection in the pathogenesis of otosclerosis has been postulated. Measles virus ribonucleic acid has been detected in the footplate of stapes on electron microscopy and immunohistochemical studies. Moreover, vaccination against the measles virus is a protective factor against otosclerosis because of the significant decrease in the incidence of vaccinated populations.[rx]
In addition to the above factors, menopause, trauma, or a major operation have been associated with either causing or aggravating otosclerosis.[rx][rx]
Other conditions of the ear which present with conductive deafness and from which otosclerosis should be differentiated include:
-
Serous otitis media
-
Adhesive otitis media
-
Congenital stapes fixation
-
Meniere disease
-
Tympanosclerosis
-
Attic fixation of head of the malleus
-
Ossicular discontinuity
It may also have to do with the interaction among three different immune-system cells known as cytokines. Researchers believe that the proper balance of these three substances is necessary for healthy bone remodeling and that an imbalance in their levels could cause the kind of abnormal remodeling that occurs in otosclerosis.
What are the symptoms of otosclerosis?
Hearing loss, the most frequently reported symptom of otosclerosis, usually starts in one ear and then moves to the other. This loss may appear very gradually. Many people with otosclerosis first notice that they are unable to hear low-pitched sounds or can’t hear a whisper. Some people may also experience dizziness, balance problems, or tinnitus. Tinnitus is a ringing, roaring, buzzing, or hissing in the ears or head that sometimes occurs with hearing loss.
The initial symptoms include being unable to hear the low-frequency sounds, such as a whisper. Also, the patients may give a history that they can hear well in noisy surroundings termed “paracusis willisii.” Though it is not specific to otosclerosis, it is indicative of conduction deafness. The patients themselves may speak at a low volume and in a monotonous voice. As the disease becomes extensive, tinnitus may worsen as well. Dizziness is usually mild, but as the disease progresses, dizziness may deteriorate, mimicking Meniere’s disease.[rx]
Symptoms of otosclerosis include:
- Hearing loss (slow at first, but worsens over time)
- Ringing in the ears (tinnitus)
- Vertigo or dizziness
- hearing loss that gets gradually worse over time
- particular difficulty hearing low, deep sounds and whispers
- speaking quietly because your voice sounds loud to you
- finding it easier to hear when there’s background noise (unlike many other types of hearing loss)
- hearing sounds, such as buzzing or humming, that come from inside your body (tinnitus)
- dizziness (though this is rare)
The symptoms of otosclerosis can be hard to tell apart from other causes of hearing loss.
How is otosclerosis diagnosed?
Otosclerosis is diagnosed by healthcare providers who specialize in hearing. These include an otolaryngologist (commonly called an ENT, because they are doctors who specialize in diseases of the ears, nose, throat, and neck), an otologist (a doctor who specializes in diseases of the ears), or an audiologist (a health care professional trained to identify, measure, and treat hearing disorders).
On physical examination, otoscopy may reveal minimal details and may be normal. However, with active otosclerosis or cochlear otosclerosis, increased promontory vascularity may be visible through the eardrum and is clinically termed as the Schwartz sign.[rx] However, this finding is only apparent in around 10%.[rx][rx]
The first step in a diagnosis is to rule out other diseases or health problems that can cause the same symptoms as otosclerosis. The next steps include hearing tests that measure hearing sensitivity (audiogram) and middle-ear sound conduction (tympanogram). Sometimes, imaging tests—such as a CT scan—are also used to diagnose otosclerosis.
Tuning Fork Test – The tuning fork test shows a negative Rinne test. Webers test is lateralized to the ear with severe conductive loss.
Audiometry and Tympanometry – Pure tone audiometry shows lower frequency loss of air conduction. However, bone conduction is normal. A bone conduction dip in thresholds of 20-30 dB and more pronounced at 2000 Hz is called a Carhart notch. After stapedectomy, Carhart notch disappears. A Carhart notch may also be present in cases of incus or malleus fixation and incudostapedial joint detachment.[rx] Also, mixed hearing loss can be seen in audiometry in patients with otosclerosis. The discrimination score is normal speech audiometry. Generally, tympanometry is normal in early otosclerosis. However, in severe cases, a flattening or a stiffness curve may be observed, indicating low compliance of the ossicular chain and tympanic membrane. Tympanometry can further differentiate otosclerosis from the pathologies with low resonance, such as a disconnection in the middle ear bone system.
High-Resolution Computed Tomography (CT) – High-resolution computed tomography (CT) of the temporal bones is the standard choice to diagnose otosclerosis.[rx] It aids in identifying and ruling out other causes of deafness. In more than 80% of the cases, the fenestral foci, located in the area anterior to the oval window, can be found. Also, the thickening of the footplate and the round window involvement can guide the treatment. Retrosternal focus visualized as a double halo sign is seen with cochlear otosclerosis.[rx] A grading system suggested by Symons and Fanning can be used for CT grading of otosclerosis.[rx]
How is otosclerosis treated?
Currently, there is no effective drug treatment for otosclerosis, although there is hope that continued bone-remodeling research could identify potential new therapies. Mild otosclerosis can be treated with a hearing aid that amplifies sound, but surgery is often required. In a procedure known as a stapedectomy, a surgeon inserts a prosthetic device into the middle ear to bypass the abnormal bone and permit sound waves to travel to the inner ear and restore hearing.
- Monitoring: If your otosclerosis is mild, your doctor may take a watch-and-wait approach and test your hearing regularly. They might also recommend that you get a hearing aid.
- Devices: Hearing aids cannot cure otosclerosis, but they can improve the hearing loss you experience because of it.
Medical Management:
Medical treatment is primarily aimed to halt the progress or prevent disease progression. There is no medical therapy that is curative for otosclerosis. Though sodium fluoride is prescribed to slow the progression of otosclerosis, its efficacy is still controversial.[rx][rx]
Bisphosphonates exert antiresorptive action, by inducing osteoclastic apoptosis. Bisphosphonates, in particular, newer generation bisphosphonates are commonly used to treat otosclerosis with promising results.[rx][rx]
Bilateral hearing aids are also used in many patients, either alone or in combination with other treatments.
Surgical Management:
The treatment of choice is stapedotomy or stapedectomy, along with the placement of a prosthesis. Surgical treatment for otosclerosis has shown good results, irrespective of the surgical approaches. Revision surgery, if indicated for otosclerosis, is met with mixed success and maybe needed with facial nerve damage, persistent vertigo, or failure to improve the hearing. Though surgery is beneficial to restore hearing, in a few of the patients, there may be a need to use hearing aids after surgical treatment.[rx][rx][rx][rx]
It is important to discuss any surgical procedure with an ear specialist to clarify potential risks and limitations of the operation. For example, some hearing loss may persist after stapedectomy, and in rare cases, surgery can worsen hearing loss.
Are there complications associated with treatment?
Like any surgical procedure, a stapedectomy carries the risk of complications. While the procedure helps about 80% to 90% of people with otosclerosis, it may not be successful in some cases. In rare instances, hearing may even be worse after surgery. So, it’s important to talk with your healthcare provider about the possible risks and limitations of otosclerosis surgery.
How long does it take to recover from otosclerosis surgery?
Most people who have a stapedectomy can return to normal routines in about one week. However, if your job requires heavy lifting or strenuous activity, you may need to take up to one month off of work. Be sure to ask your healthcare provider what to expect if you’re about to undergo a stapedectomy.
Can I prevent otosclerosis?
Unlike other hearing problems, there are no preventable risk factors for otosclerosis (such as exposure to loud noises). Some people simply have a genetic predisposition for the condition. As a result, there’s no way to prevent otosclerosis from developing.
What can I expect if I have otosclerosis?
You’ll likely need a hearing aid or surgery, depending on the severity of your condition. In some cases, your healthcare provider may monitor your condition and recommend treatment only when symptoms worsen.
Can otosclerosis be cured?
Otosclerosis can’t be cured. Surgery can greatly improve the hearing loss caused by otosclerosis. Hearing aids can successfully manage your hearing loss as well.
When should I see my healthcare provider?
Any time you notice a change or decrease in your hearing ability, it’s important to schedule an appointment with your healthcare provider. Prompt diagnosis and treatment can help ease troublesome symptoms so you can return to normal life.
What questions should I ask my healthcare provider?
If you’ve been diagnosed with otosclerosis, you may want to ask the following questions:
- How serious is my condition?
- Would hearing aids help or do I need surgery?
- How long can I wait before scheduling surgery?
- How long will it take for my hearing to worsen without treatment?
References







