Chedoke-McMaster Stroke Assessment (CMSA) is a screening and assessment tool utilized to measure physical impairment and activity of an individual following a stroke[1]. The CMSA consists of two inventories. First is the Impairment Inventory, which assesses 6 domains (shoulder pain and stages of recovery of postural control, arm, hand, leg and foot). Each domain is scored on a 7-point scale (Stage 1 through 7, most impairment through to no impairment, respectively). Second is the Activity Inventory, formerly Disability Inventory, which assesses gross motor function (10 items evaluating rolling, sitting, transferring and standing) and walking (5 items)[1]. The 15 items are scored on a 7-point scale (1 through 7, complete dependence to independent, respectively).
Purpose
The CMSA has three overall purposes:
- Stage motor recovery to classify individuals in terms of clinical characteristics
- Predict rehabilitation outcomes
- Measure clinically important change in physical function[1]
Intended Population
The CMSA was initially developed for the assessment of patients with stroke, its application has been more widely demonstrated, specifically for the Activity Inventory.
This assessment tool was initially developed and validated for use with clients from an inpatient and day-hospital population. The initial development and validation studies were carried out on a Stroke Unit of the Chedoke Rehabilitation Centre[2]. The Activity Inventory (formerly the Disability Inventory) has been shown to be a valid measure of functional change in clients in an acute neurological setting[3] and for those with acquired brain injury[4]. The Chedoke Assessment has been shown to function as discriminative, predictive, and evaluative measure. The minimal clinically important difference (MCID) of the Activity Inventory for neurological clients, including those with stroke, is 7 points when determined a physiotherapist, 4, 6, 7 and the MCID of the Activity Inventory is 8 points when determined by clients with stroke and their caregivers.[5][6] In addition, predictive equations have been developed for both the Impairment Inventory and the Activity Inventory for use with patients with acute stroke8 or patients with stroke in the rehabilitation setting[7]. The predictive equations can be found in Chapter 8 of the manual. The potential for using the Impairment Inventory scores as a predictor of independent ambulation has also been reported[8].
Methods of Use
Users of the CMSA should read the manual (linked below) prior to administration for the measures and be familiar with relevant administration, scoring and interpretation . No special training is required.[1]
Overview of the Measure
The CMSA is composed of 2 inventories:
- The Impairment Inventory
- The Activity Inventory
Impairment Inventory: Used to determine the presence and severity of common physical impairments. It has 6 dimensions:
- Recovery stage of the arm
- Hand
- Leg
- Foot
- Postural control
- Shoulder pain
Each dimension is measured on a 7-point scale, each point corresponds to seven stages of motor recovery. The 7-point scale for shoulder pain is based on pain severity.
Activity Inventory: measures clinically important changes in the client’s functional ability. This Activity Inventory is made up of a gross motor function and walking subscale.
The Gross Motor Function index consists of the 10 following items:
- Supine to side lying on strong side
- Supine to side lying on weak side
- Side lying to long sitting through strong side
- Side lying to sitting on side of the bed through strong side
- Side lying to sitting on side of the bed through weak side
- Standing
- Transfer to and from bed toward strong side
- Transfer to and from bed toward weak side
- Transfer up and down from floor to chair
- Transfer up and down from floor and standing
The Walking Index consists of the 5 following items:
- Walking indoors
- Walking outdoors, over rough ground, ramps, and curbs
- Walking outdoors several blocks
- Stairs
- Age and sex appropriate walking distance in meters for 2 minutes
The maximum score is 100, where higher scores reflect normal function[2]
Framework
Physical Setting, Environment and Clothing
- Ensure patient feels comfortable and at ease during administration of assessment
- Distractions kept to a minimum
- Testing room should be comfortable warm and large enough to accommodate a low plinth (large enough to allow patient to roll from supine to sidelying), floor mat and wheelchair
- Access to full flight of stairs and outdoors required for Activity Inventory
- Patients should wear comfortable clothing (i.e., shorts and tank top) exposing knees and elbows
- During testing of shoulder pain, shoulder region should be free of clothing
- Shoes and orthoses not worn during Physical Impairment Inventory, but worn for Activity Inventory[1]
Equipment
All equipment should be assembled ahead of time.
- Foot stool
- Pillows
- 2 meter line marked on the floor
- Chair with armrest
- Adjustable table
- Plastic measuring cup (250 ml)
- Wide, low plinth
- Stop watch
- Floor mat
- Ball, 6.5 cm (2.5 in) in diameter
- 1 liter plastic pitcher with water
Testing
Testing takes approximately 45 to 60 minutes to complete an assessment. It may not be feasible to complete the entire test in one session, however, effort should be made to complete the assessment within 2 days. Prior to assessment, the therapist should check relevant medical history and identify any condition(s) that may put a patient at risk.[1]
During assessment, the physiotherapist’s instruction, whether words or gestures, should be clear and concise. To ensure thorough understanding, a movement task may be demonstrated, a patient’s limb may be passively moved through a task or patient may be asked to perform a task on the uninvolved side. Once the patient understands, test instructions are given and movement task is observed. Tasks can only be attempted twice in the Impairment Inventory and once in the Activity Inventory.[2]
The following are reasons to end a task or assessment:
- Neither safe nor prudent
- Activity may worsen patient’s condition (i.e., rolling onto painful shoulder)
- Patient becomes excessively fatigued or apprehensive
Administration Guidelines
Impairment Inventory
Starting Positions
Standard starting positions are indicated at the top of each Score Form. If standard position is changed, indicate on form. Therapist may assist patient to starting position. When indicated may stabilize part being tested and may provide assistive support (only light support, no weight bearing) to patient so balance is not lost.
Testing begins at:
- Stage 3 for arm, hand and foot
- Stage 4 for postural control and leg
Testing Procedures[1]
When instructing patient, use simple commands. Modifications to instructions may be necessary to ensure patient understands required movements.
| Stage | Testing Procedure | Acceptable Assistance | Inacceptable Assistance |
|---|---|---|---|
| 2 | Involves facilitated active movement, in any range. Testing for tone – part passively put through available range of motion briskly with two repetitions. |
Visible muscle contractions qualify as movement. Facilitatory stimulus (i.e., manual stimuli). Maximum of two repetitions per task. |
Increased muscle tone alone. Ice or mechanical devices. |
| 3 to 7 | Voluntary movement is tested. | Facilitation techniques. | |
| 6 | Full range of motion with near normal timing and coordination. | ||
| 7 | Full range of motion and rapid complex movements with normal timing. Timing and coordination of the task must be comparable to the uninvolved side. |
Movements not equal to uninvolved side. |
*Any tasks involved greater than half or full range of motion, compare with range on uninvolved side.
Interpretation and Scoring
Impairment Inventory
Shoulder Pain
When assessing stage of shoulder pain, consider any pain that is present and its relationship to functional activities, even those not involving the shoulder or arm. Steps in the Shoulder Assessment are as follows:
- Ask questions regarding pain and function
- Test range of motion
- Examine shoulder and scapula
Ensure prognostic indicators are noted that assist in predicting shoulder pain. The following indicators are most significant:
- Arm is in low stage of recovery, Stage 1 or 2
- Scapula is misaligned. It can be elevated, depressed, abducted or adducted
- Loss of range of motion with flexion or abduction < 90˚ or external rotation < 60˚[1]
Stages of Shoulder Pain
Proceed with the shoulder pain assessment using the following descriptions. Match the descriptions with your impression of the client’s pain. Record the stage of shoulder pain in the appropriate box on the Score Form.
Stage 1 – Constant, severe arm and shoulder pain in more than just the shoulder
Stage 2 – Intermittent, severe arm and shoulder pain in more than just the shoulder
Stage 3 – Constant shoulder pain in just the shoulder
Stage 4 – Intermittent shoulder pain in just the shoulder
Stage 5 – Shoulder pain is noted during testing, but the functional activities that the client normally performs are not affected by the pain
Stage 6 – No shoulder pain, but at least one prognostic indicator is present
Stage 7 – Shoulder pain and prognostic indicators are absent[1]
Motor Recovery for Postural Control, Arm, Hand, Leg and Foot
Stages of Motor Recovery
Principles of Motor Recovery:
- Motor recovery from hemiplegia follows a stereotyped sequence of events
- Performance of selected motor tasks, requiring increased complex motor control, indicates central nervous system recovery
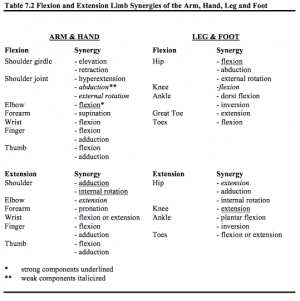
- In the early stages, movement first occurs in limb synergy patterns. As stages progress, movement patterns out of the synergy in more complex and independent patterns.
- Postural control, arm, hand, leg and foot may recover at different rates. The stage of recovery of the proximal part of the limbs is often in a higher stage than the distal. Movements involving flexion are at a different stage of recovery than movements involving extension.
- Stages of Motor Recovery measure the amount of neurological impairment
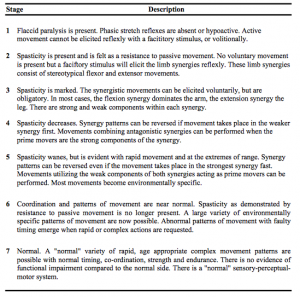
Definitions of the Stages of Motor Recovery
Stage 1 – Flaccid paralysis is present. Phasic stretch reflexes are absent or hypoactive. Active movement cannot be elicited reflexly with a facititory stimulus, or volitionally.
Stage 2 – Spasticity is present and is felt as a resistance to passive movement. No voluntary movement is present but a faciftory stimulus will elicit the limb synergies reflexly. These limb synergies consist of stereotypical flexor and extensor movements.
Stage 3 – Spasticity is marked. The synergistic movements can be elicited voluntarily, but are obligatory. In most cases, the flexion synergy dominates the arm, the extension synergy the leg. There are strong and weak components within each synergy.
Stage 4 – Spasticity decreases. Synergy patterns can be reversed if movement takes place in the weaker synergy first. Movements combining antagonistic synergies can be performed when the prime movers are the strong components of the synergy.
Stage 5 – Spasticity wanes, but is evident with rapid movement and at the extremes of range. Synergy patterns can be reversed even if the movement takes place in the strongest synergy fast. Movements utilizing the weak components of both synergies acting as prime movers can be performed. Most movements become environmentally specific.
Stage 6 – Coordination and patterns of movement are near normal. Spasticity as demonstrated by resistance to passive movement is no longer present. A large variety of environmentally specific patterns of movement are now possible. Abnormal patterns of movement with faulty timing emerge when rapid or complex actions are requested.
Stage 7 – Normal. A “normal” variety of rapid, age appropriate complex movement patterns are possible with normal timing, co-ordination, strength and endurance. There is no evidence of functional impairment compared to the normal side. There is a “normal” sensory-perceptualmotor system. [1]
Stage of Postural Control
Standard Starting Position: No shoes and socks. No standard position. Encourage good sitting posture (ie. with hips and knees at 90°) during testing when indicated. Start the assessment at Stage 4.
STAGE 1 – Unable to demonstrate at least two of the Stage 2 tasks
STAGE 2
Task 1: Facilitated log roll to side lying
Task 2: Resistance to trunk rotation
Task 3: Static righting with facilitation
STAGE 3
Task 1: Log roll to side lying
Task 2: Move forward and backward
Task 3: Remain upright for 5 seconds
STAGE 4
Task 1: Segmental rolling to side lying
Task 2: Righting within the base of support
Task 3: Standing Up
STAGE 5
Task 1: Dynamic righting side to side, feet on floor
Task 2: Standup with equal weight bearing
Task 3: Step forward onto weak leg, transfer weight
STAGE 6
Task 1: Dynamic righting backward or sideways with displacement, feet off floor
Task 2: On weak leg 5 seconds
Task 3: Sideways braiding for 2 meters
STAGE 7
Task 1: Abduction of strong leg
Task 2: Tandem walking 2 meters in 5 seconds
Task 3: Walk on toes 2 meters
Stage of ARM
Standard Starting Position: Sitting with the forearm in the lap or supported on a pillow in the lap in a neutral position, wrist at 0° and fingers slightly flexed. Sitting either unsupported over the side of the bed or plinth, or supported in a chair or wheelchair. Feet should be supported. Encourage good sitting posture during testing (ie. with hips and knees at 90°). Start the assessment at Stage 3.
STAGE 1 – Unable to demonstrate at least two of the Stage 2 tasks.
STAGE 2
Task 1: Resistance to passive shoulder abduction or elbow extension
Task 2: Facilitated elbow extension
Task 3: Facilitated elbow flexion
STAGE 3
Task 1: Touch opposite knee
Task 2: Touch chin
Task 3: Shoulder shrugging greater than half range
STAGE 4
Task 1: Extension synergy, then flexion synergy
Task 2: Shoulder flexion to 90°
Task 3: Supination then pronation
STAGE 5
Task 1: Flexion synergy, then extension synergy
Task 2: Shoulder abduction to 90° with pronation
Task 3: Pronation then supination
STAGE 6
Task 1: Hand from knee to forehead 5 times in 5 seconds
Task 2: Trace a vertical figure 8
Task 3: Raise arm overhead with full supination
STAGE 7
Task l: Clap hands overhead, then clap hands behind back 3 times in 5 seconds
Task 2: Scissor in front 3 times in 5 seconds
Task 3: Resisted shoulder external rotation
Stage of Hand
Standard Starting Position: Sitting with the forearm in the lap, or supported on a pillow, in a neutral position, wrist at 0° and fingers slightly flexed. The client can sit either unsupported on the side of the bed or plinth, or supported in a chair or wheelchair. Feet should be supported. Encourage good sitting posture for testing (ie. with hips and knees at 90°). Start the assessment at Stage 3.
STAGE 1 – Unable to demonstrate at least two of the Stage 2 tasks.
STAGE 2 – Support the limb as necessary while facilitating the movements.
Task 1: Positive Hoffman
Task 2: Resistance to passive wrist or finger extension
Task 3: Facilitated finger flexion
STAGE 3
Task 1: Wrist extension greater than 1/2 of the remaining range
Task 2: Finger or wrist flexion greater than 1/2 of the remaining range
Task 3: Thumb to index finger
STAGE 4
Task 1: Finger extension then flexion
Task 2: Thumb extension greater than 1/2 range, then lateral prehension
Task 3: Finger flexion with lateral prehension
STAGE 5
Task 1: Finger flexion then extension
Task 2: Finger abduction
Task 3: Opposition of thumb to little finger
STAGE 6
Task 1: Tap index finger 10 times in 5 seconds
Task 2: Pull trigger, then return
Task 3: Wrist and finger extension with finger abduction
STAGE 7
Task 1: Thumb to finger tips, then reverse 3 times in 12 seconds
Task 2: Bounce a ball 4 times in succession, then catch it
Task 3: Pour 250 ml. from 1 liter pitcher, then reverse
See Manual for stages of Leg and Foot (
Scoring the Impairment Inventory
Scoring is based on a 7-point ordinal scale corresponding to the stages of recovery. The patient may attempt each task twice. Additional attempts that train the patient to achieve a task are not permitted. To receive credit, patient muscle complete task at least once. Place an ‘X’ in corresponding box for tasks completed.
- If patient fails to complete two of the three tasks in the stage where testing began, move to lower stage until two tasks are accomplished in a single stage
- If two tasks are accomplished at the stage where testing began, assess the third task, but regardless of result, move up to next stage
- In order to progress from Stage 6 to 7, need to complete all tasks in Stage 6 and at least 2 tasks in Stage 7
- The patient’s stage of recovery is the highest stage where at least two of the three tasks are accomplished
- The score is placed in the box provided and note any limitations that will impact function
Impairment Inventory yields a total score of 42, with lower scores indicating greater impairment.[1]
Activity Inventory
Purpose of Activity Inventory is to assess the patient’s functional level. Therefore, focus on task accomplishment, not quality of movement.
Description of the Levels of Function and Scores
| Level | Description |
|---|---|
| Independent | Another person is not required for the activity (NO HELPER). |
| 7 – Complete Independence | All of the tasks which make up the activity are typically performed safely, without modification, assistive devices, or aids, and within reasonable time. |
| 6 – Modified Independence | Activity requires any one or both of the following to complete the task: an assistive device (i.e., foot orthoses, cane), or more than reasonable time (at least 3 times longer than normal). |
| Dependent | Another person is required for either supervision or physical assistance in order for the activity to be performed, or it is not performed (REQUIRES HELPER). |
| Modified Dependence | The subject expends half (50%) or more of the effort.
The levels of assistance required are: |
| 5 – Supervision | The client requires no more help than standby supervision, cueing or coaxing, without physical contact. |
| 4 – Minimal Contact Assistance | With physical contact the subject requires no more help than touching, and client expends 75% or more of the effort. |
| 3 – Moderate Assistance | The client requires more help than touching, or expends half (50%) or more (up to 75%) of the effort. |
| Complete Dependence | The client expends less than half (less than 50%) of the effort. Maximal or total assistance is required, or the activity is not performed.
The levels of assistance required are: |
| 2 – Maximal Assistance | The client expends less that 50% of the effort, but at least 25%. |
| 1 – Total Assistance | The client expends less than 25% of the effort, 2 persons are required for assistance, or the task is not tested for safety reasons. |
The therapist is expected to score each task, do not leave any item blank. If a task is not tested due to concerns for the patient’s safety, assign a score of 1.
The Activity Inventory yields a total score of 100, with lower scores indicating greater impairment. The minimum score is 14, where 7 points are allotted to the first 14 items and 2 points for item 15 (2-minute walk test). [1]
Evidence
Reliability
Reproducibility of the CMSA has been established, however, reliability of all testers during administration varies. Recommendations are that facilities test interrater and intrarater reliability, as appropriate, in regards to administration and scoring guidelines and clinical application. Following testing, intrarater reliability was 0.93-0.98 and interrater reliability was 0.85-0.96 for Impairment Inventory and 0.98 for Activity Inventory. Test-retest reliability for the total scores ranged from 0.97 to 0.99.
Validity
The CMSA has not been validated for use on patients who are less than one week post-stroke. Construct and concurrent validities were studied and confirmed that the Impairment Inventory total score was found to correlate with the Fugl-Meyer Test (r = 0.95, p < 0.001) and the Activity Inventory with the Functional Independence Measure (r = 0.79, p < 0.05).
The minimal clinically important difference (MCID) of the CMSA for neurological patients, including those with stroke, is 7 points when determined by a physiotherapist and 8 points when determined by patients with stroke and caregivers.
Overall, studies confirm that the CMSA yields both reliable and valid results. The CMSA can be used with confidence as both a clinical and a research tool that can discriminate among subjects and evaluate patient outcomes.
MINIMALLY CLINICALLY IMPORTANT DIFFERENCE (MCID)
Acute Stroke: (Gowland et al 1993; n = 32; mean age = 64; mean time since stroke onset = 9 months)[2]
- MCID = 8 points (total CMSA via stroke patients) and 7 points (total CMSA via caregivers of stroke patients).
CUT-OFF SCORES
> 9 on the leg and postural control scores indicates that the individual is able to ambulate independently.[9]
TEST/RETEST RELIABILITY[2]
- Excellent test-retest reliability, Disability Inventory (ICC = 0.98)
INTERRATER/INTRARATER RELIABILITY[2]
- Excellent inter-rater reliability, Impairment inventory ICC = 0.97
- Excellent inter-rater reliability, Disability inventory ICC = 0.99
- Excellent intra-rater reliability, Impairment inventory ICC = 0.98
INTERNAL CONSISTENCY[2]
- Excellent internal consistency, Total scale ICC = 0.98
CRITERION VALIDITY (PREDICTIVE/CONCURRENT)[2]
- Excellent concurrent validity: Fugl-Meyer (r = 0.95)
- Excellent concurrent validity: FIM (r = 0.79)
- Excellent concurrent validity: Barthel Index of ADLs (r = 0.75 -0.87 *Disability Index)
- Poor concurrent validity with, Barthel Index: areas of shoulder pain & eating and bowel incontinence (r <0.30)
- Excellent predictive validity, Physical Impairment Scale Leg postural control scores of >9 showed 100% sensitivity and 80% specificity in prediction of independent ambulation.
- Excellent predictive validity, Total outcome of CMSA stroke assessment could be predicted by 7 items on the Barthel Index (R-2 = 0.75)
CONSTRUCT VALIDITY[2]
- Excellent convergent validity with subscales of the Fugl-Meyer Assessment (FMA)
- Excellent convergent validity with the CMSA Arm and hand Impairment Inventory and FMA shoulder, elbow, forearm, wrist and hand scale (r = 0.95)
- Excellent convergent validity with the CMSA Leg and foot Impairment Inventory and FMA hip, knee, foot and ankle scale (r = 0.93)
- Excellent convergent validity with the CMSA Postural control and FMA balance scale (r = 0.84)
- Excellent convergent validity with the CMSA Shoulder pain Impairment Inventory and FMA upper limb joint pain scale (r = 0.76)