Your parasympathetic nervous system is part of your autonomic nervous system. It could be called your “automatic” nervous system, as it’s responsible for many functions that you don’t have to think about to control. This can include control of your heart rate, blood pressure, digestion, urination and sweating, among other functions.
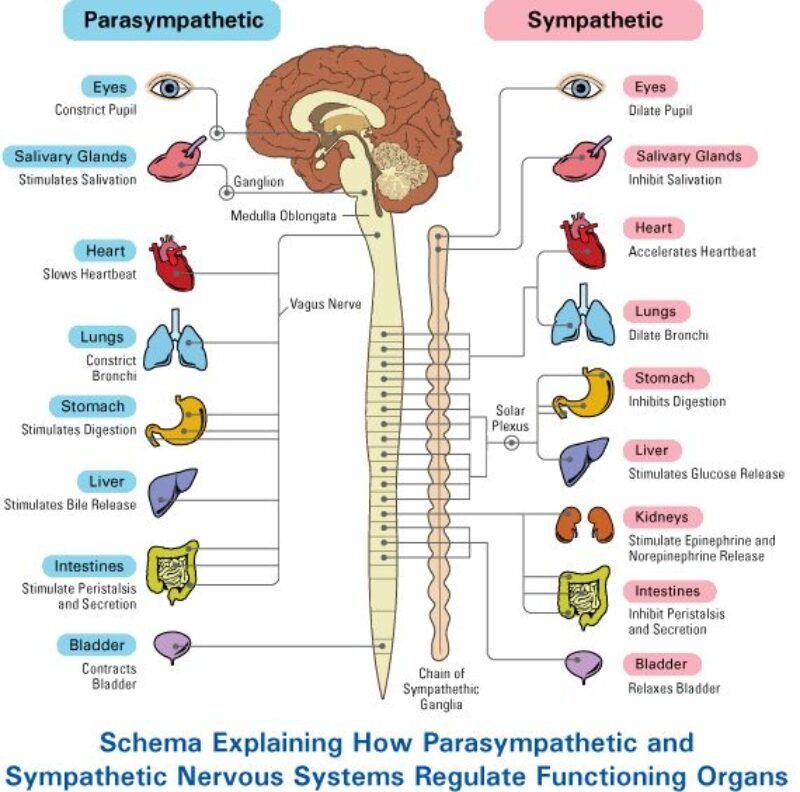
The parasympathetic part of your autonomic nervous system balances your sympathetic nervous system. While your sympathetic nervous system controls your body’s “fight or flight” response, your parasympathetic nervous system helps to control your body’s response during times of rest.
The parasympathetic nervous system (PNS) is one of two main divisions of the autonomic nervous system, the other being the sympathetic nervous system. The PNS primarily functions to promote “rest and digest” activities, helping the body recover from stressful situations and conserve energy. It does this by slowing down heart rate, increasing digestive activity, and regulating other bodily functions like urination and pupil dilation.
What is the Sympathetic and Parasympathetic Nervous System?
We have two main components to our nervous system, one that is under our conscious control (e.g. moving your body) and another that works automatically on our behalf (e.g. controlling heart rate). The automatic part (ANS) is responsible for all bodily processes that occur without conscious control, including our emotional expression, and helps us mobilise energy with our sympathetic nervous system or conserve energy through our parasympathetic nervous system. The nervous system and brain work together to make sense of what it happening inside the body and outside of the body to ensure that we adapt and respond as needed in order to survive.
- The sympathetic nervous system is associated with activated states such as the fight or flight response and is designed to energise and mobilise the body
- The parasympathetic system is associated with deactivated states such as rest, relaxation, digestion, and recovery after stress as well as freeze states
The sympathetic and parasympathetic nervous systems are meant to work together in a balanced way. When the nervous system is working adaptively we will find ourselves ‘dancing’ between these systems, back and forth with activating and deactivating states, throughout the day. If it has lost its flexibility then you may feel stuck in over-active, alert states like anxiety and physical tension or de-activated, unmotivated, foggy or flat states.
Anatomy
Where is the parasympathetic nervous system located?
Your parasympathetic nervous system is one of two parts of your autonomic nervous system. Your autonomic nervous system is a subsystem of your peripheral nervous system, which is all the nervous tissue in your body excluding your brain and spinal cord.
Your parasympathetic nervous system uses four of your 12 cranial nerves. These are nerves that connect directly to your brain. Three of those four only involve your senses and glands connected to your eyes, nose and mouth.
The fourth, your vagus nerve, connects to part of your mouth and also extends down through your neck to your chest and abdomen (belly). Your vagus nerve makes up about 75% of your parasympathetic nervous system overall, connecting to your heart, lungs and other vital internal organs.
Farther down, 31 spinal nerves connect directly to your spinal cord, but your parasympathetic nervous system only uses some of them in the lower part of your spine. This sends signals to your bladder and bowels to relax so you can use the bathroom.
Structure
The parasympathetic nerves are autonomic or visceral [rx][rx] branches of the peripheral nervous system (PNS). Parasympathetic nerve supply arises through three primary areas:
- Certain cranial nerves in the cranium, namely the preganglionic parasympathetic nerves (CN III, CN VII, CN IX and CN X) usually arise from specific nuclei in the central nervous system (CNS) and synapse at one of four parasympathetic ganglia: ciliary, pterygopalatine, otic, or submandibular. From these four ganglia the parasympathetic nerves complete their journey to target tissues via trigeminal branches (ophthalmic nerve, maxillary nerve, mandibular nerve).
- The vagus nerve (CN X) does not participate in these cranial ganglia as most of its parasympathetic fibers are destined for a broad array of ganglia on or near thoracic viscera (esophagus, trachea, heart, lungs) and abdominal viscera (stomach, pancreas, liver, kidneys, small intestine, and about half of the large intestine). The vagus innervation ends at the junction between the midgut and hindgut, just before the splenic flexure of the transverse colon.
- The pelvic splanchnic efferent preganglionic nerve cell bodies reside in the lateral gray horn of the spinal cord at the T12–L1 vertebral levels (the spinal cord terminates at the L1–L2 vertebrae with the conus medullaris), and their axons exit the vertebral column as S2–S4 spinal nerves through the sacral foramina.[7] Their axons continue away from the CNS to synapse at an autonomic ganglion. The parasympathetic ganglion where these preganglionic neurons synapse will be close to the organ of innervation. This differs from the sympathetic nervous system, where synapses between pre- and post-ganglionic efferent nerves in general occur at ganglia that are farther away from the target organ.
As in the sympathetic nervous system, efferent parasympathetic nerve signals are carried from the central nervous system to their targets by a system of two neurons. The first neuron in this pathway is referred to as the preganglionic or presynaptic neuron. Its cell body sits in the central nervous system and its axon usually extends to synapse with the dendrites of a postganglionic neuron somewhere else in the body. The axons of presynaptic parasympathetic neurons are usually long, extending from the CNS into a ganglion that is either very close to or embedded in their target organ. As a result, the postsynaptic parasympathetic nerve fibers are very short
| Organ | Nerves[rx] | Spinal column origin[rx] |
|---|---|---|
| stomach |
|
T5, T6, T7, T8, T9, sometimes T10 |
| duodenum |
|
T5, T6, T7, T8, T9, sometimes T10 |
| jejunum and ileum |
|
T5, T6, T7, T8, T9 |
| spleen |
|
T6, T7, T8 |
| gallbladder and liver |
|
T6, T7, T8, T9 |
| colon |
|
|
| pancreatic head |
|
T8, T9 |
| appendix |
|
T10 |
| bladder |
|
S2-S4 |
| kidneys and ureters |
|
T11, T12 |
Structure and Function
Both divisions of the ANS are comprised of a complex network of pathways responsible for maintaining the physiologic integrity of organs, tissues, and cells. They are composed of pre- and postganglionic neurons that act on effector organs.[rx] The preganglionic neurons of the PNS come from brainstem nuclei and the sacral spinal cord (specifically S2-S4). The axons of preganglionic PNS neurons are much longer than those of the SNS and synapse with the postganglionic neurons in the ganglia at or near the effector organs. The very short postganglionic axons then relay signals to the cells of the effector organs. Those preganglionic parasympathetic neurons that begin in the brainstem leave the central nervous system (CNS) through cranial nerves. Cranial nerves carrying parasympathetic functions include the oculomotor nerve (III) acting on the eyes, the facial nerve (VII) working on the lacrimal gland, the salivary glands, and the mucous membranes within the nasal cavity, the glossopharyngeal nerve (IX) acting on the parotid gland, and the vagus nerve (X) acting on the viscera of the abdomen and thorax. The vagus nerve is particularly influential within the PNS as it carries 75% of all parasympathetic fibers. The preganglionic fibers from the sacral cord join to form pelvic splanchnic nerves, which act on the pelvic cavity viscera.[rx]
The PNS uses acetylcholine as its neurotransmitter for pre- and postganglionic neurons activating muscarinic receptors. This differs from the SNS, which uses norepinephrine, which acts on adrenergic receptors, as the primary neurotransmitter for most postganglionic neurons. The primary exception is sweat glands stimulated by the SNS, which have cholinergic postganglionic neurons.[rx] Muscarinic receptors are integral membrane proteins comprised of 5 subtypes (M1-M5) located on different effector organs. M1, M3, and M5 are coupled to Gq proteins, which signal through the IP3 pathway, while M2 and M4 receptors couple to Gi proteins, which signal through the cAMP pathway.[rx] The type of receptor and its location determine the functions of the PNS. The actions of the PNS are listed below:
-
In the male reproductive tract, parasympathetic stimulation of M3 receptors causes smooth muscle relaxation in the helicine arteries of the penis, allowing blood to fill the corpora cavernosa and corpus spongiosum, causing an erection. The PNS also gives excitatory signals to the vas deferens, seminal vesicles, and prostate.[rx]
-
In the eye, parasympathetic stimulation of M3 receptors causes contraction of the iris’s sphincter muscle, leading to pupil constriction (miosis). Additionally, it causes contraction of the ciliary muscle, improving near vision.
-
In the heart, parasympathetic stimulation of M2 receptors causes decreased heart rate and conduction velocity through the AV node.
-
In the vasculature, parasympathetic stimulation of M3 receptors leads to vasodilation.
-
In the lungs, parasympathetic stimulation of M3 receptors leads to bronchoconstriction. It also increases bronchial secretions.
-
In salivary glands, parasympathetic stimulation of M1 and M3 receptors leads to high-volume secretion of potassium ions, water, and amylase.
-
In the stomach and intestines, parasympathetic stimulation of M receptors leads to increased motility and relaxation of sphincters. Stimulation of M receptors also increases gastric secretions to aid in digestion.
-
In the gallbladder, parasympathetic stimulation of M3 receptors stimulates contraction to release bile.
-
In the pancreas, parasympathetic stimulation of M3 receptors leads to the release of digestive enzymes and insulin.
-
In the kidneys and bladder, parasympathetic stimulation of M3 receptors stimulates ureter peristalsis, contraction of the detrusor muscle, and relaxation of the internal urethral sphincter, aiding in the flow and excretion of urine.
After being released from cholinergic neurons and acting on muscarinic receptors, acetylcholine is quickly inactivated or removed from the neuroeffector junction to allow new signals to come through. In cholinergic synapses, this action is primarily performed enzymatically by acetylcholinesterase. It hydrolyzes acetylcholine into choline and acetate in less than 1 millisecond, making it 1 of the fastest enzymes in the body.[rx]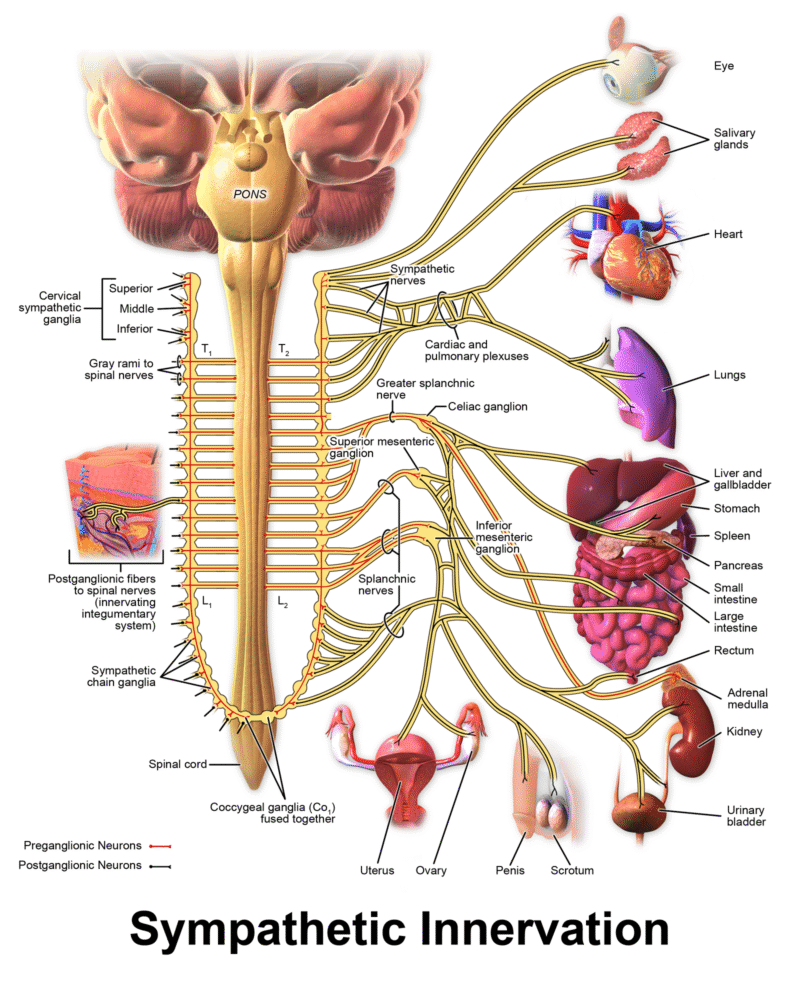
What does the parasympathetic nervous system do?
Your parasympathetic nervous system’s job is usually to relax or reduce your body’s activities. Because of the signals it carries, the rhyming phrases “rest and digest” or “feed and breed” are easy ways to remember what your parasympathetic nervous system does.
Your parasympathetic nervous system can have the following effects:
- Eyes: It constricts your pupils to limit how much light enters your eyes. It also makes changes that can help improve your close-up vision, and causes tear production in your eyes.
- Nose and mouth: It makes glands in your mouth produce saliva, and glands in your nose produce mucus. This can be helpful with digestion and breathing during times of rest.
- Lungs: It tightens airway muscles and ultimately reduces the amount of work your lungs do during times of rest.
- Heart: It lowers your heart rate and the pumping force of your heart.
- Digestive tract: It increases your rate of digestion and diverts energy to help you digest food. It also tells your pancreas to make and release insulin, helping your body break down sugars into a form your cells can use.
- Waste removal: It relaxes the muscles that help you control when you pee (urinate) or poop (defecate).
- Reproductive system: It manages some of your body’s sexual functions, including feeling aroused (erections in people with a penis and secreting fluids that provide lubrication during sex in people with a vagina).
What Influences Activation of the Nervous System Branches?
As previously mentioned the brain and nervous system work together to make sense of what is happening inside and outside of the body to ensure effective adaptation and survival. I like to think of the body, mind and brain as representing a mass communication device, both transmitting and receiving information to inform conscious and unconscious responses. With survival as the the most fundamental aspect of our human programming, we are designed to adapt by heeding the demands of the body, rising to challenges inside and outside of us, avoiding threat and discomfort and then to drop back down to rest, safety and recovery.
Influences on the branches include many factors including: genetics, personality, tolerance of uncertainty, physical demand, competition for needed resources, illness, lack of safe and comfortable downtime, stress, lack of relationships that offer emotional safety, good nutrition, functional mobility and breathing and oxidative stress.
When it comes to the parasympathetic nervous system we need to talk about the Vagus Nerve which is its main component. I have made this a subject for another page because it deserves to be understood in much more detail in its own right. Understanding the Vagus Nerve and how to influence it is very helpful in helping learn to balance the very normal and high amount of stress that life often involves.
What’s the difference between the parasympathetic and sympathetic nervous systems?
Your sympathetic and parasympathetic nervous systems have opposite but complementary roles. Your sympathetic nervous system carries signals that put your body’s systems on alert, and your parasympathetic carries signals that return those systems to their standard activity levels.
Your sympathetic nervous system takes the lead when your safety and survival are at risk, but that system’s actions can strain body systems when it’s active for too long. Because these two systems offset each other, they help maintain balance in your body.
Your parasympathetic nervous system also manages the activity in organs throughout your body when you feel calm and safe. These functions don’t involve risk or danger but are still key in keeping you alive and healthy.
Sympathetic and parasympathetic nervous system flexibility is key to maintaining emotional and physical wellbeing. The nervous system is involved in nearly every aspect of our health and guides everyday activities such as waking up, breathing; and complex processes such as thinking, reading, remembering, and generating emotions. Most commonly it is known to determine our stress response and recovery but it is involved so many of our body/mind processes beyond that. Understanding how your nervous system works is key to developing good health and wellbeing strategies.
The Sympathetic and parasympathetic nervous system controls:
- Brain growth and development
- Sensations (such as touch or hearing)
- Perception (interpreting sensory information)
- Thought and emotions
- Learning and memory
- Movement, balance, and coordination
- Sleep
- Healing and rehabilitation
- Stress and the body’s responses to stress
- Ageing
- Breathing and heartbeat
- Body temperature
- Hunger, thirst, and digestion
- reproductive health, and fertility
Conditions and Disorders
What are the common conditions and disorders that affect the parasympathetic nervous system?
Many conditions and problems can affect your autonomic nervous system, including your parasympathetic nervous system. Potential problems include:
- Type 2 diabetes. Uncontrolled Type 2 diabetes can damage your autonomic nervous system, including your parasympathetic nervous system.
- Congenital and genetic conditions. These are disorders or conditions you have at birth. You have genetic conditions because you inherit them from one or both parents. Inherited forms of amyloidosis can cause parasympathetic nervous system problems.
- Parasympathetic nervous system problems can cause incontinence when there’s damage to the nerves that control your bladder and bowels.
- Multiple system atrophy. This severe condition is similar to Parkinson’s disease, damaging autonomic nerves over time.
- Sexual dysfunction. People with parasympathetic nervous system damage may have erectile dysfunction.
- Trauma. Nerve damage from injuries is potentially long-term or even permanent. This is especially the case when you have injuries to your spinal cord or main nerve structures that impair or cut off parasympathetic connections farther down.
What are some common signs and symptoms of parasympathetic nervous system problems?
Your parasympathetic nervous system controls processes in your body that should happen automatically. That means these problems usually get noticed when something doesn’t happen as expected. Possible symptoms include:
- Constipation.
- Fast heart rate (tachycardia) even when resting.
- Heart rhythm problems (including arrhythmias such as atrial fibrillation).
- Sexual dysfunction.
- Trouble digesting food (including gastroparesis).
What are some common tests to check parasympathetic nervous system functions?
Potential tests include:
- Blood tests (these can detect many problems, ranging from immune system problems to the levels of neurotransmitters in your blood).
- Electrocardiogram (EKG).
- Genetic testing.
- Magnetic resonance imaging (MRI).
- Sweat testing (including how much you sweat and seeing if there are places on your body where you don’t sweat as you should).
What are the common treatments for parasympathetic nervous system conditions?
Treating conditions that affect your parasympathetic nervous system is often challenging. That’s because the treatments can change dramatically, depending on what’s behind the problem. The treatments can also include many different approaches, ranging from medication to surgery.
Sometimes, treatment of a parasympathetic nervous system problem requires treating or curing an underlying problem. In other cases, a condition isn’t curable, and the goal will be to treat and minimize the impact of symptoms.
Care
How can I prevent conditions and problems that affect the sympathetic nervous system?
Prevention can make all the difference in protecting and maintaining your parasympathetic nervous system. The best preventive measures include:
- Eat a balanced diet. Vitamin deficiencies, especially vitamin B12, can damage your nervous system. You should also avoid overusing vitamins (especially B6, which has toxic effects on your nervous systems at high levels).
- Avoid abusing drugs and alcohol. Substance use, including frequent heavy drinking, can have toxic effects and damage your sympathetic nervous system.
- Stay physically active and maintain a healthy weight. Type 2 diabetes damages your autonomic nerves over time. That’s why preventing it, or at least delaying when it starts, can make a big difference in your overall well-being.
- Wear safety equipment as needed. Safety equipment can be a big help if you want to prevent nerve damage from injuries, regardless of whether you use the equipment during work or play activities.
- Manage chronic conditions as recommended. If you have a chronic condition that can damage your nervous system, you should take steps to manage this condition. Your healthcare provider can help guide you on how to do that. That guidance can make a big difference in helping you limit the condition’s progress or how it affects your life.
Disclaimer: Each person’s journey is unique, treatment plan, life style, food habit, hormonal condition, immune system, chronic disease condition, geological location, weather and previous medical history is also unique. So always seek the best advice from a qualified medical professional or health care provider before trying any treatments to ensure to find out the best plan for you. This guide is for general information and educational purposes only. Regular check-ups and awareness can help to manage and prevent complications associated with these diseases conditions. If you or someone are suffering from this disease condition bookmark this website or share with someone who might find it useful! Boost your knowledge and stay ahead in your health journey. We always try to ensure that the content is regularly updated to reflect the latest medical research and treatment options. Thank you for giving your valuable time to read the article.
The article is written by Team Rxharun and reviewed by the Rx Editorial Board Members
Last Updated: April 23, 2025.






