The lateral cricoarytenoid (LCA) muscle is a small but important muscle located in the voice box (larynx). Tumors developing in this muscle are extremely rare. However, because even rare tumors can affect vocal function and breathing, understanding the anatomy, possible causes, symptoms, diagnostic methods, treatment options, and preventive measures is important.
Anatomy of the Lateral Cricoarytenoid Muscle
Understanding the structure and function of the lateral cricoarytenoid muscle is key before discussing tumor pathology.
Location and Structure
-
Location:
The lateral cricoarytenoid muscle is located in the larynx (voice box). It is found along the lateral (side) wall of the cricoid cartilage, which is the ring-shaped cartilage in the throat. -
Origin:
It originates from the outer surface of the cricoid cartilage, a sturdy structure that supports the larynx. -
Insertion:
The muscle attaches to the muscular process of the arytenoid cartilage, which is one of the small paired cartilages that help control the position of the vocal cords.
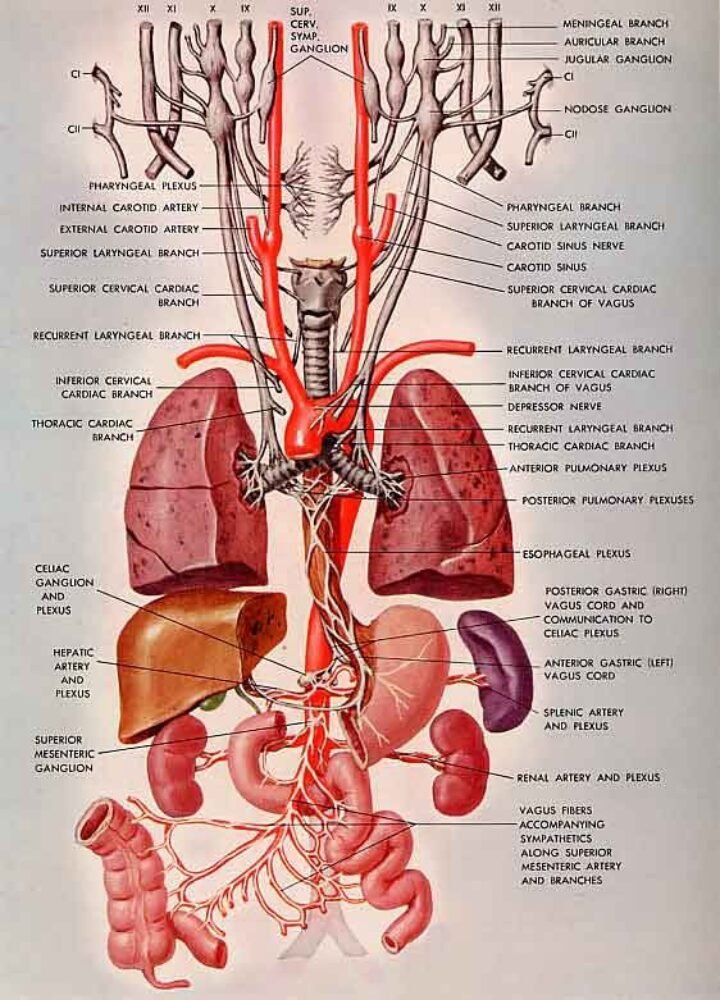
Blood Supply and Nerve Supply
-
Blood Supply:
The lateral cricoarytenoid muscle typically receives blood from branches of nearby arteries. In many cases, the superior thyroid artery (or its branches) supplies blood to the laryngeal muscles, including the LCA. -
Nerve Supply:
The recurrent laryngeal nerve supplies motor innervation to the lateral cricoarytenoid muscle. This nerve is critical for controlling the movements that affect voice and airway protection.
Key Functions
-
Adduction of Vocal Folds:
The LCA muscle contracts to pull the arytenoid cartilages forward, which helps bring the vocal folds together. This is crucial for producing sound. -
Voice Production:
By regulating the position and tension of the vocal folds, the muscle helps in modulating pitch and volume. -
Breathing Regulation:
It plays a role in managing the opening of the airway, thereby affecting the passage of air during breathing. -
Prevention of Aspiration:
Proper movement of the vocal folds helps protect the airway from food and fluids entering the lungs. -
Assisting with Coughing:
It contributes indirectly to an effective cough, which is essential for clearing the airway. -
Stabilization of the Larynx:
The muscle also acts as a stabilizer, ensuring that the laryngeal cartilages maintain proper alignment during speaking and swallowing.
Types of Lateral Cricoarytenoid Muscle Tumors
Tumors involving the LCA muscle are uncommon, but they can range in their behavior and severity. Broadly, they are classified into two categories:
Benign Tumors
These are non-cancerous growths that generally grow slowly and do not spread:
-
Leiomyoma: A benign tumor that arises from smooth muscle cells.
-
Fibroma: A growth composed of fibrous tissue.
-
Lipoma: Although more common in other parts of the body, lipomas can occasionally occur near laryngeal muscles.
-
Hemangioma: A benign tumor composed of blood vessels.
-
Neuroma: A benign nerve tissue growth that might be found incidentally in the region.
Malignant Tumors
These are cancerous growths that can invade surrounding tissues and spread (metastasize):
-
Sarcoma: A broad term covering malignant tumors arising from muscle or connective tissue.
-
Chondrosarcoma: A cancer that forms in cartilage, which may involve nearby structures.
-
Rhabdomyosarcoma: A rare cancer arising from muscle tissue; though more common in children, it is one possibility.
-
Undifferentiated Carcinoma: A category sometimes used when the tumor cells appear very abnormal and do not clearly belong to a specific tissue type.
-
Mixed Tumors: Tumors that have both benign and malignant components or display features of more than one type of cancer.
Because the lateral cricoarytenoid muscle is small and embedded within the complex anatomy of the larynx, tumors here are difficult to isolate. Often, these tumors are discovered as part of broader laryngeal pathology.
Possible Causes of Lateral Cricoarytenoid Muscle Tumors
While many factors may contribute to the development of tumors (including those in the LCA), not every factor is fully proven. However, evidence and clinical observations suggest that the following 20 causes or risk factors can be involved:
-
Genetic Mutations: Inherited gene changes that predispose individuals to tumor formation.
-
Exposure to Tobacco Smoke: Smoking is a well-known risk factor for many laryngeal tumors.
-
Alcohol Consumption: Chronic alcohol use can contribute to the development of head and neck cancers.
-
Environmental Carcinogens: Exposure to chemical irritants or pollutants may increase risk.
-
Occupational Exposures: Working in industries with inhaled chemicals or pollutants, such as construction or manufacturing.
-
Chronic Laryngitis: Prolonged inflammation of the larynx may predispose tissue to malignant changes.
-
Viral Infections: Certain viruses (e.g., human papillomavirus, HPV) have been linked to head and neck cancers.
-
Radiation Exposure: Previous radiation therapy to the neck region for other cancers might increase risk.
-
Age: Increased age is a risk factor for many types of tumors, including those in the larynx.
-
Gender: Men are statistically more likely to develop laryngeal tumors.
-
Dietary Factors: Poor nutrition or deficiencies may weaken immune surveillance of abnormal cells.
-
Occupational Stress: Chronic stress and its biological effects might influence tumor growth indirectly.
-
Hormonal Imbalances: Changes in hormone levels can influence cellular growth.
-
Immune System Suppression: A compromised immune system might not detect and destroy abnormal cells effectively.
-
Genetic Syndromes: Rare inherited conditions that predispose to multiple tumors.
-
Chronic Irritation: Repeated minor traumas or irritants in the laryngeal area.
-
Inflammatory Conditions: Long-term inflammatory diseases can contribute to abnormal cell growth.
-
Vocal Overuse: Chronic strain from excessive speaking or singing might lead to microtrauma.
-
Prior Laryngeal Surgery: Scar tissue or alterations in local anatomy may predispose the area to tumor formation.
-
Unknown Factors: In some cases, no clear risk factor is identified despite comprehensive evaluation.
These causes underline why lifestyle, environmental, and genetic factors often interact in complex ways to contribute to tumor formation.
Symptoms of Lateral Cricoarytenoid Muscle Tumors
Symptoms of a tumor in the lateral cricoarytenoid muscle can vary depending on the size and location of the tumor and whether it affects surrounding structures. Here are 20 possible symptoms:
-
Hoarseness: A change in the quality or strength of the voice.
-
Breathing Difficulty: Feeling of shortness of breath or stridor.
-
Throat Pain: Discomfort or pain in the throat area.
-
Dysphagia: Difficulty swallowing.
-
Voice Fatigue: Tiring easily when speaking for long periods.
-
Pain on Speaking: Discomfort that is noticeable while talking.
-
Foreign Body Sensation: Feeling like something is stuck in the throat.
-
Chronic Cough: A non-resolving cough that persists.
-
Sore Throat: An ongoing sore or irritated throat.
-
Difficulty Projecting the Voice: Reduced volume or power of the voice.
-
Loss of Vocal Range: Inability to reach higher or lower notes.
-
Throat Tightness: A feeling of tightness or constriction in the throat.
-
Swelling: Visible or palpable lumps in the neck area.
-
Pain Radiating to the Ear: Sometimes throat pain may be referred to the ear.
-
Difficulty Breathing During Exercise: Problems intensify with physical exertion.
-
Changes in Voice Timbre: The quality of the voice may sound different.
-
Stridor: A high-pitched wheezing sound during breathing.
-
Fatigue: Overall tiredness that may be associated with systemic illness.
-
Unexplained Weight Loss: May occur in malignant cases.
-
Persistent Throat Clearing: Feeling the need to constantly clear the throat.
Not every patient will experience all these symptoms, and the severity can range from mild to severe. Early symptoms are often subtle.
5. Twenty Diagnostic Tests for Lateral Cricoarytenoid Muscle Tumors
Due to the anatomical location of these tumors, a combination of imaging, endoscopy, and laboratory tests is generally used. Below are 20 diagnostic tests that might be considered:
-
Laryngoscopy: A flexible or rigid scope is used to visualize the larynx and its muscles.
-
Direct Laryngoscopy: A procedure performed under anesthesia to get a detailed look.
-
Videostroboscopy: Uses a strobe light to evaluate vocal fold vibration.
-
Computed Tomography (CT) Scan: Provides detailed cross-sectional images of the larynx.
-
Magnetic Resonance Imaging (MRI): Offers high-resolution images of soft tissues.
-
Ultrasound Examination: May help assess superficial lesions.
-
Positron Emission Tomography (PET) Scan: Detects metabolic activity often elevated in tumors.
-
Biopsy: Tissue sampling is critical for determining the type and nature of the tumor.
-
Fine Needle Aspiration (FNA): A minimally invasive method to obtain cells for analysis.
-
Endoscopic Ultrasound: Combines endoscopy and ultrasound imaging for better visualization.
-
Voice Analysis: Objective measurements of voice quality and function.
-
Blood Tests: To rule out infection or markers of systemic disease.
-
Immunohistochemical Staining: Helps identify cell types in tumor tissue.
-
Genetic Testing: For identifying genetic mutations associated with cancer.
-
Bronchoscopy: If the tumor is suspected to impact the airway beyond the larynx.
-
Chest X-ray: To check for potential spread, particularly in malignant cases.
-
Sputum Cytology: Analysis of mucus or sputum cells for cancer cells.
-
Staging Scans: A combination of imaging tests to determine the extent of disease spread.
-
Laryngeal Electromyography (EMG): To assess neuromuscular function of laryngeal muscles.
-
Histopathological Examination: Detailed laboratory examination of removed tissue to evaluate the tumor type.
The choice of diagnostic test depends on the initial clinical findings and the suspected stage or type of the tumor.
6. Thirty Non-Pharmacological Treatments
Non-pharmacological approaches play a crucial role in managing laryngeal tumors, especially to improve quality of life and support recovery. Here are 30 strategies:
-
Voice Therapy: Work with a speech-language pathologist to improve voice use.
-
Vocal Rest: Resting the voice to prevent further irritation.
-
Lifestyle Modifications: Reducing factors (like smoking) that may worsen symptoms.
-
Dietary Modifications: Eating a balanced diet to support overall health.
-
Hydration: Drinking plenty of water to keep throat tissues moist.
-
Humidified Air: Using a humidifier to maintain moisture in the air.
-
Smoking Cessation: Programs or support groups to help quit smoking.
-
Stress Management: Techniques such as meditation to reduce stress-induced muscle tension.
-
Respiratory Therapy: Exercises to enhance breathing and support lung function.
-
Posture Training: Maintaining good posture to reduce strain on the neck and throat.
-
Physical Therapy: Exercises to strengthen and stabilize nearby neck muscles.
-
Acupuncture: May help alleviate pain and improve overall well-being.
-
Yoga: Certain gentle practices may improve breathing and reduce stress.
-
Biofeedback Therapy: Using electronic monitoring to learn how to control physiological functions.
-
Dietary Supplements: Under professional guidance, supplements can support tissue repair.
-
Nutritional Counseling: Guidance on nutrition tailored to recovery and health.
-
Alternative Therapies: Including herbal remedies that some patients find useful.
-
Mindfulness Techniques: Practicing mindfulness to reduce anxiety.
-
Breathing Exercises: Techniques that strengthen respiratory muscles.
-
Vocal Hygiene: Learning good vocal practices to minimize strain.
-
Environmental Modifications: Adjusting work and home environments to reduce exposure to irritants.
-
Support Groups: Connecting with others who have similar conditions.
-
Cognitive Behavioral Therapy (CBT): To manage anxiety and stress.
-
Relaxation Techniques: Progressive muscle relaxation to ease tension.
-
Manual Therapy: Hands-on techniques from a trained therapist to relieve tightness.
-
Aromatherapy: Using essential oils (with caution) for relaxation.
-
Home Remedies: Warm teas or lozenges to soothe throat discomfort.
-
Sleep Hygiene: Good practices to ensure restful sleep and recovery.
-
Speech Modification Training: Learning to use your voice in ways that reduce stress on the larynx.
-
Regular Monitoring: Routine self-checks and follow-ups to note any changes in symptoms.
These options can be used alongside medical treatments, and many patients benefit from a multidisciplinary approach.
7. Twenty Drugs That May Be Used in Management
Although drug therapy is typically more relevant for cancers affecting the larynx rather than strictly benign tumors, here are 20 drugs that might be part of a treatment plan for lateral cricoarytenoid muscle tumors when indicated:
-
Cisplatin: A chemotherapy drug commonly used in head and neck cancers.
-
Carboplatin: Often used in combination with other agents for cancer treatment.
-
5-Fluorouracil (5-FU): A chemotherapeutic agent that interferes with tumor cell division.
-
Docetaxel: A drug used in some regimens for advanced laryngeal cancers.
-
Paclitaxel: A chemotherapy drug that may be included in treatment protocols.
-
Epirubicin: An anthracycline used in some head and neck cancer treatments.
-
Bleomycin: Sometimes added in combination therapies.
-
Methotrexate: Can be used in certain regimens for head and neck malignancies.
-
Cetuximab: A targeted therapy that blocks receptors on cancer cells.
-
Pembrolizumab: An immunotherapy drug used in selected head and neck cancer patients.
-
Nivolumab: Another immunotherapy option showing promise in controlling tumor growth.
-
Interferon-alpha: May be used in particular settings as an immunomodulatory agent.
-
Erlotinib: A targeted therapy drug sometimes evaluated in head and neck cancers.
-
Vinorelbine: A chemotherapy option in some treatment combinations.
-
Gemcitabine: A drug used in certain protocols for tumor control.
-
Ifosfamide: Part of combination regimens in soft tissue sarcoma.
-
Doxorubicin: Frequently used against soft tissue cancers.
-
Lenvatinib: A targeted therapy for certain cancers in the head and neck region.
-
Sorafenib: Another multikinase inhibitor sometimes trialed in these tumors.
-
Supportive Medications: Such as analgesics, antiemetics, and corticosteroids to manage symptoms during cancer treatment.
Treatment with these drugs depends heavily on tumor type, stage, and overall patient health. In many cases, a multidisciplinary team makes these decisions.
8. Ten Surgical Approaches
Surgery is often considered when a tumor is localized and operable. Depending on the tumor’s characteristics, these surgical options might be used:
-
Transoral Laser Surgery: Minimally invasive laser techniques to remove small tumors.
-
Microlaryngoscopic Surgery: Uses small instruments and a microscope for precise removal.
-
Endoscopic Resection: Using an endoscope to excise the tumor with minimal incisions.
-
Partial Laryngectomy: Removal of part of the larynx if the tumor is confined.
-
Total Laryngectomy: In advanced cases, complete removal of the larynx might be necessary.
-
Open Resection: Traditional surgery involving an external neck incision for tumor removal.
-
Neck Dissection: Removal of nearby lymph nodes if there is spread.
-
Reconstructive Surgery: To repair or rebuild laryngeal structures after tumor removal.
-
Salvage Surgery: Performed when initial treatments do not yield the desired result.
-
Laser-Assisted Endoscopic Resection: A combination of laser technology with endoscopy to maximize precision while minimizing tissue damage.
The exact procedure will depend on the tumor’s size, location, and malignancy.
9. Ten Prevention Tips
Prevention of tumors in the laryngeal region is largely about reducing risk factors that predispose to cancer. Here are ten prevention tips:
-
Avoid Smoking: Tobacco is a major risk factor for laryngeal and other head and neck cancers.
-
Limit Alcohol Use: Excessive alcohol consumption increases risk.
-
Minimize Exposure to Pollutants: Reduce contact with industrial chemicals and air pollutants.
-
Vaccination: Consider HPV vaccination, which can lower the risk of certain head and neck cancers.
-
Healthy Diet: A diet rich in fruits and vegetables supports overall tissue health.
-
Regular Exercise: Helps boost overall health and immune function.
-
Maintain Vocal Hygiene: Avoid overusing or straining your voice.
-
Regular Check-Ups: Early screening and check-ups can help in detecting changes sooner.
-
Use Protective Equipment: In occupations with potential exposure to harmful chemicals, always use proper protective gear.
-
Stress Reduction: Techniques to manage stress may help reduce overall risk factors for chronic inflammation.
10. When to See a Doctor
It’s important to consult a healthcare provider if you notice any issues with your voice or breathing. See a doctor if you experience:
-
Persistent hoarseness or change in your voice lasting more than two weeks.
-
Difficulty breathing or a noisy breathing pattern.
-
Ongoing throat pain or a lump in your neck.
-
Trouble swallowing or feeling that something is stuck in your throat.
-
Unexplained weight loss or fatigue coupled with throat symptoms.
-
Changes in the quality or volume of your voice, especially if you use your voice professionally.
Early evaluation can lead to timely diagnosis and treatment.
11. Fifteen Frequently Asked Questions (FAQs)
Below are answers to 15 common questions regarding lateral cricoarytenoid muscle tumors:
Q1: What is the lateral cricoarytenoid muscle?
A: It is a muscle in your larynx that helps move the vocal cords for speaking, breathing, and protecting your airway.
Q2: How common are tumors in the lateral cricoarytenoid muscle?
A: They are very rare, which is why information mostly comes from broader research into laryngeal tumors.
Q3: What are the signs of a tumor in this muscle?
A: Common signs include hoarseness, difficulty breathing, throat pain, and persistent cough, among others.
Q4: What causes these tumors?
A: Causes may include smoking, alcohol use, genetic factors, environmental carcinogens, chronic inflammation, viral infections, prior radiation, and more.
Q5: How is a tumor in the LCA muscle diagnosed?
A: Through a variety of tests including laryngoscopy, CT or MRI scans, biopsies, and voice analysis.
Q6: Are these tumors usually benign or malignant?
A: They can be both. Benign tumors like fibromas may occur; malignant forms, though rare, can be more serious.
Q7: What non-drug treatments are available?
A: Voice therapy, vocal rest, physical therapy, lifestyle changes, and supportive care are among the non-pharmacological options.
Q8: Which drugs might be used if treatment is needed?
A: Chemotherapy drugs such as cisplatin, targeted therapies like cetuximab, and supportive medications are sometimes employed.
Q9: What surgical options exist?
A: Options range from minimally invasive laser surgery to partial or total laryngectomy, depending on the tumor.
Q10: Can I prevent a tumor in the larynx?
A: While not all tumors can be prevented, avoiding smoking, limiting alcohol, and maintaining overall health can lower your risk.
Q11: How does vocal therapy help?
A: It helps by teaching you proper voice use, reducing strain, and improving overall vocal health.
Q12: What are common diagnostic imaging tests used?
A: CT scans, MRI, PET scans, and detailed endoscopic procedures are commonly used.
Q13: When is surgery recommended?
A: Surgery is considered when the tumor is localized and significantly affecting breathing or voice, especially in malignant cases.
Q14: How important is early detection?
A: Very important. Early detection leads to better outcomes and a greater chance for preserving voice function.
Q15: Where can I find more information?
A: Trusted sources include medical journals, hospital websites, and consultations with laryngologists or head and neck surgeons.
Conclusion
Lateral cricoarytenoid muscle tumors, though rare, affect a vital part of the voice box involved in speaking and breathing. This guide has provided comprehensive details—from the exact anatomy of the muscle and its functions to lists of potential causes, symptoms, diagnostic tests, treatment options (both non-pharmacological and pharmacological), surgical approaches, and prevention tips. Understanding the complexity of these tumors can help you recognize symptoms early and seek the appropriate medical care.







