Osteoarthritis of spine is known as degenerative of spinal joints, the breakdown of the cartilage, tendon, ligaments of the joints and discs in the neck and lower back. Sometimes, osteoarthritis produces spurs that put pressure on the nerves leaving the spinal column. This can cause weakness and pain in the arms or legs.

Joints of Spine
Joints provide flexibility, support, stability, and protection. Specific parts of the joint: the synovium and cartilage, provide these functions.
Synovium. The synovium is the tissue that lines a joint. Synovial fluid is a lubricating fluid that supplies nutrients and oxygen to cartilage.
Cartilage. The cartilage is a slippery tissue that coats the ends of the bones. Cartilage is composed of four components:
- Water – Cartilage is composed mostly of water, which decreases with age. About 85% of cartilage is water in young people. Cartilage in older people is about 70% water.
- Chondrocytes – Chondrocytes, the basic cartilage cells, are critical for joint health.
- Proteoglycans – These large molecules bond to water, which keeps high amounts of water in cartilage.
- Collagen – This essential protein in cartilage forms a mesh to give joint support and flexibility. Collagen is the main protein found in all connective tissues of the body, including the muscles, ligaments, and tendons.
Anatomy of Spine
Individual radiographic features of the spine commonly studied and referred to as the “three-joint complex”, are the structures of vertebral osteophytes (OST), facet joint OA (FOA), and disc space narrowing (DSN) from intervertebral disc degeneration [rx]. All of these spinal structures have adequate nerve supply capable of generating LBP.
The vertebral facet joints (zygapophyseal joints) are synovial joints with the typical features of hyaline cartilage over subchondral bone, a synovial membrane, and a joint capsule [rx]. Facet joint OA is a multifactorial process, and it has been thought that the presence of intervertebral disc degeneration leads to a greater load and motion at the facet joint, resulting in degenerative changes similar to those seen in other synovial joints [rx]. However, the presence of facet joint OA has been found to be present even in the absence of intervertebral disc degeneration [rx].
Situated between two vertebral bodies, the intervertebral disc is made up of two main regions: the soft inner nucleus pulposus and the firm outer collagenous annulus fibrosis [rx]. The collagen content of the intervertebral disc consists of both type I and II collagen, with the nucleus containing only type II whereas the annulus contains both types I and II [rx]. Changes to the disc collagen content can occur naturally with aging, a process commonly referred to as intervertebral disc degeneration. These aging-related changes include a decrease in aggrecan, water, and collagen content [rx], resulting in DSN on plain film radiographs.
A vertebral osteophyte is a bony outgrowth that arises from the periosteum at the junction of bone and cartilage [rx]. Osteophyte formation in the vertebral column has been shown to be a general indicator of age [rx]. Osteophytes, however, may form without overt cartilage damage, implying they may form in an otherwise healthy joint [rx]. However, the presence of disc space narrowing is highly associated with osteophyte formation [rx].
The process of degeneration in the spine is thought to be initiated by disc degeneration; this disc degeneration is hypothesized to result in segmental instability that increases the load on the facet joints and leads to cartilage alterations [rx]. This process has been clinically debated with little research support. Recently, Suri and colleagues [rx] reported results from an ancillary project using 435 participants in the Framingham Heart Study. Using computed tomography (CT), they report that, for most individuals, there is ordered progression of spine degeneration beginning with the intervertebral disc. They also remark that increasing age, body mass index (BMI), and female sex may be related to isolated facet joint degeneration in some individuals [rx].
Spine Osteoarthritis or Degeneration?
Osteoarthritis is the clinical outcome of a disease process that results in structural and functional failure of synovial joints. This process has been characterized by damage to articular cartilage, subchondral bone alteration, a synovial inflammatory response, and an overgrowth of bone and cartilage [rx]. In the spine, both the presence of intervertebral disc degeneration and osteophyte formation at the same vertebral level has been used to define lumbar spine OA, otherwise known as spondylosis [rx]. Intervertebral disc degeneration and osteophyte formation may not share the same pathophysiological process of degeneration or have the anatomical synovial structures necessary to collectively meet the definition of OA.
Types of Arthritis In the Spine
However, inflammation is typically absent in osteoarthritis until the later stages of the disease. Because of this, osteoarthritis can go by several different names including:
- Spondylosis
- Osteoarthrosis
- Spinal Stenosis
- Degenerative Joint Disease
- Degenerative Disc Disease
The joints are the connection between two bones that allow movement while providing support. In between the bones of the joint is a cavity filled with liquid known as synovial fluid.
Covering the ends of each bone is a type of flexible, yet strong, connective tissue known as articular cartilage. The synovial fluid acts as a shock absorber and helps to prevent wear and tear of this cartilage caused by friction. The cartilage further protects the bones from everyday wear and tear and also helps to absorb shock.
Our spine, or vertebral column, is set up a bit differently than other joints. The spine is broken down into five different sections:
- The Neck, or Cervical Spine
- Mid-back, or Thoracic Spine
- Lower back, or Lumbar Spine
- The upper portion of the pelvic cavity, or Sacral Spine
- Tailbone, or Coccyx
It has 24 individual vertebrae (essentially the joints) and is covered in cartilage as well. However, the spine has gel-like pads, called discs, instead of cavities filled with synovial fluid.
These discs are filled with a fluid that is comprised of degenerated collagen, proteoglycans and water. This gel-like center is called the nucleus pulposus, and it acts as the shock absorber for the spine.
Risk factors for osteoarthritis back pain include
- Age
Genetic factors
- Heritability estimates for hand, knee and hip OA are about 40-60%.
- The responsible genes are largely unknown.
Local, largely biomechanical risk factors
- Joint injury.
- Occupational and recreational stresses on joints.
- Reduced muscle strength.
- Joint Laxity.
- Joint malalignment.
Constitutional factors
- Aging.
- Female sex.
- Obesity.
- High bone density – a risk factor for the development of OA.
- Low bone density – a risk factor for the progression of knee and hip OA
- Weight – “Carrying around excess weight increases the wear and tear on your spine,” notes Dr. Kovacs.
- Back injury – A history of trauma to your spine or a history of spinal surgery can increase your risk of developing spinal arthritis. Additionally, joint injury is a common cause of osteoarthritis in younger populations, according to NIAMS.
- Stress and strain – Repetitive strain on the neck and back from leaning, twisting, and lifting can also increase the risk of osteoarthritis. This may be from athletic activities like hockey, football, gymnastics, or weightlifting, as well as from certain occupations.
- Spinal misalignment – Scoliosis, a sideways curvature of the spine, or other forms of spinal misalignment can put stress on the joints and increase the risk of spinal osteoarthritis.

Osteoarthritis causes the breakdown of the articular cartilage and primarily affects the weight-bearing joints including the knees, hips, and spine. However, it can affect any of the joints such as the fingers and toes.
As the articular cartilage degenerates, the bones begin to rub against each other causing friction. Over time, this friction causes the bones to become worn down essentially compressing the joint. In the later stages, this can cause inflammation, which exacerbates the problem and the pain.
Osteophytes, or bone spurs, begin to grow on the bones where the articular cartilage is worn down. This is Mother Nature’s attempt at healing the degeneration.
Unfortunately, bone spurs can lead to even more problems including interfering with the blood flow to the vertebrae and the curvature of the spine. This can cause stiffness in the joints and a very uncomfortable feeling called “locking.”
Locking is essentially a joint getting stuck. It can be very painful, or there may be no pain whatsoever. It can be very disconcerting, but normally the joint will unlock with a little bit of gentle manipulation. Osteophytes can also cause entrapment of the spinal nerves, and spinal stenosis (loss of space for the nerves to pass through).
Osteoarthritis is one of the leading causes of back pain, and the pain it causes in the joints is difficult to distinguish from muscle pain. When osteoarthritis settles into the spine, the vertebrae aren’t the only parts affected. The discs are affected as well.
Degeneration of the vertebral joints causes excessive strain on the discs, which can cause dehydration of the nucleus pulposus (the gel-like center) of the disc. As a result, the ability to absorb shock and lubricate the joint is lost. This can lead to a number of problems including:
- Bulging of the disc out of the vertebral space
- Compression of the vertebrae
- Herniation is when the jelly-like contents escape through a thinned portion of the disc wall and spill into the spinal canal, which can put pressure on the spinal nerves
Anatomical structures relevant to osteoarthritis of the spine:
- Vertebrae
- Intervertebral discs
- Spinal cord
- Facet joints
- Vertebral body
- Spinous process
- Transverse process
- Lamina
- Pedicle
- Sacrum
- Coccyx
- Cervical spine
- Thoracic spine
- Lumbar spine
- Articular cartilage
- Synovial membrane
- Synovial fluid
- Ligaments (e.g., anterior longitudinal ligament, posterior longitudinal ligament)
- Annulus fibrosus
- Nucleus pulposus
- Zygapophyseal joint
- Spinal nerves
- Intervertebral foramina
- Spinal canal
- Epidural space
- Vertebral arch
- Vertebral foramen
- Intertransverse ligament
- Interbody joint
- Paraspinal muscles

Crepitus, or cracking sounds, can occur after being in one position for long periods. The sound is caused by the bones of the joints rubbing together, or a bone spur rubbing against one of the bones of the joint. Crepitus tends to occur more frequently in the neck, hips, and knees.
Many people with osteoarthritis notice improvement in their pain after exercising. I’m one of these people. Cardio exercise and weight training exercises have made a huge difference in my pain levels.
www.rxharun.com
Causes of Osteoarthritis of the Spine
Lower back pain is mainly triggered due to the condition of osteoarthritis of the lumbar spine. Due to this degenerative joint disease, the lumbar joints become inflamed which results in severe pain, restricted mobility, and in extreme cases it may result in permanent paralysis. If you are experiencing the following cases it is of utmost importance that you consult your doctor immediately.
- Repetitive stress: Activities or occupations that involve repetitive motions or heavy lifting can contribute to spinal degeneration.
- Joint injury: Previous injuries, such as fractures or dislocations, can increase the risk of osteoarthritis in the affected area.
- Poor posture: Incorrect posture and spinal alignment may contribute to increased stress on the spinal joints.
- Smoking: Smoking has been linked to increased inflammation and a higher risk of osteoarthritis.
- Gender: Women tend to be at a slightly higher risk of developing osteoarthritis of the spine.
- Hormonal changes: Some studies suggest that hormonal changes, particularly in women after menopause, may play a role in the development of osteoarthritis.
- Inflammation: Chronic inflammation in the body can contribute to the breakdown of cartilage in the spine.
- Bone and joint disorders: Conditions like rheumatoid arthritis or gout can increase the risk of developing osteoarthritis.
- Congenital abnormalities: Some individuals may be born with spinal abnormalities that increase the risk of osteoarthritis later in life.
- Joint hypermobility: Excessive joint flexibility can lead to increased wear and tear on the spinal joints.
- Nutritional factors: Poor nutrition, including a diet lacking in essential vitamins and minerals, may contribute to joint degeneration.
- Diabetes: People with diabetes have an increased risk of developing osteoarthritis.
- Metabolic disorders: Certain metabolic conditions, such as hemochromatosis, can lead to joint damage and osteoarthritis.
- Certain occupations: Jobs that involve heavy lifting, repetitive motions, or prolonged sitting or standing can increase the risk of spine osteoarthritis.
- Previous spine surgeries: Prior surgeries on the spine can contribute to altered biomechanics and increase the risk of osteoarthritis.
- Spinal misalignments: Conditions like scoliosis or abnormal curvature of the spine can lead to uneven stress distribution and joint degeneration.
- Joint instability: Ligamentous laxity or weak supporting structures can increase the risk of osteoarthritis.
- Immobility: Prolonged periods of immobility or bed rest can weaken the muscles supporting the spine and contribute to joint degeneration.
- Environmental factors: Exposure to certain toxins or pollutants may increase the risk of osteoarthritis.
- Certain medications: Some medications, such as long-term corticosteroid use, may increase the risk of osteoarthritis.
- Trauma: Traumatic injuries, such as fractures or dislocations, can lead to joint damage and osteoarthritis.
- Other medical conditions: Certain conditions like Paget’s disease or acromegaly can increase the risk of osteoarthritis.
- Joint infections: Infections that affect the joints can lead to joint damage and osteoarthritis.
- Autoimmune diseases: Some autoimmune conditions, such as lupus or psoriasis, can contribute to joint degeneration.
- Nerve compression: Conditions like spinal stenosis or herniated discs can lead to nerve compression and contribute to joint degeneration.
- Unknown factors: In some cases, the exact cause of osteoarthritis of the spine may be unknown.
Degeneration or wear and tear of the joints due to the natural process of aging.
- Injury or trauma, such as a car accident triggers the process of joint cartilage erosion or joint irritation.
- Repetitive stress injury like typing on the computer for long hours without taking a break or lifting a heavy load on a daily basis is one of the most common causes of osteoarthritis.
- The hereditary cause may also contribute to osteoarthritis.
- Disc degeneration may also cause osteoarthritis. The intervertebral disc supporting the two lumbar vertebrae may undergo degeneration due to stress and aging. This may cause pain, stiffness, and difficulty in moving the lumbar joint.
- The exercise-induced injury is most common among active individuals like athletes. This is because the increased activity level increases friction when the bones in the joints rub against each other. This causes the wearing off of the cartilage and the supporting structures that provide joint stability.
- Wear and tear due to aging Injuries such as whiplash
- A genetic cartilage defect
- Poor posture
- Repetitive movement
- Obesity
- Poor diet
- Genetics
- Gender
- Other diseases such as diabetes or gout
Symptoms of Osteoarthritis of the Spine
Common symptoms associated with osteoarthritis of the spine:
- Back pain: Persistent or intermittent pain in the back, often worsened by movement.
- Stiffness: Feeling stiff or inflexible, particularly after rest or in the morning.
- Reduced range of motion: Difficulty bending, twisting, or turning the spine.
- Neck pain: Pain or discomfort in the neck region.
- Headaches: Frequent headaches, especially at the base of the skull.
- Radiating pain: Pain that travels from the spine to other areas of the body, such as the arms or legs.
- Numbness or tingling: Sensations of numbness, tingling, or pins and needles in the arms or legs.
- Muscle weakness: Weakness in the muscles of the arms or legs.
- Loss of balance: Difficulty maintaining balance while standing or walking.
- Difficulty walking: Problems with walking due to pain or stiffness.
- Limited mobility: Reduced ability to perform daily activities or tasks.
- Fatigue: Feeling tired or lacking energy.
- Muscle spasms: Involuntary contractions or tightening of muscles.
- Joint swelling: Swelling or inflammation in the affected joints.
- Grinding sensation: A sensation of grinding or popping when moving the spine.
- Morning stiffness: Stiffness and discomfort in the spine upon waking up.
- Worsening pain with activity: Pain that intensifies with movement or physical exertion.
- Pain with prolonged sitting or standing: Discomfort or pain when sitting or standing for extended periods.
- Loss of height: Gradual loss of height over time due to compression of the spine.
- Changes in posture: Changes in the alignment or curvature of the spine.
- Difficulty sleeping: Trouble sleeping due to pain or discomfort.
- Decreased grip strength: Reduced strength and coordination in the hands.
- Swelling or tenderness in the joints: Joint inflammation or tenderness in the spine.
- Limited flexibility: Reduced ability to bend or flex the spine.
- Increased pain during weather changes: Heightened pain during changes in weather or barometric pressure.
- Nerve impingement: Compression or irritation of spinal nerves, leading to radiating pain.
- Difficulty with fine motor skills: Challenges with tasks requiring precise hand movements.
- Balance problems: Impaired balance and stability.
- Changes in bowel or bladder function: Rare cases may involve bowel or bladder dysfunction.
- Generalized discomfort: A sense of overall discomfort or unease in the affected areas.
It’s important to note that these symptoms may vary from person to person, and not everyone with osteoarthritis of the spine will experience all of them. If you suspect you have osteoarthritis or are experiencing any of these symptoms, it’s recommended to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Lab Diagnostic of Osteoarthritis of Spine
Common diagnosis and tests used for osteoarthritis of the spine:
- Medical history assessment: The doctor will inquire about your symptoms, their duration, and any relevant medical history.
- Physical examination: The doctor will examine your spine, checking for signs of tenderness, swelling, or limited range of motion.
- X-rays: X-ray images provide a detailed view of the bones and can reveal bone spurs, narrowing of the joint space, and other osteoarthritis-related changes.
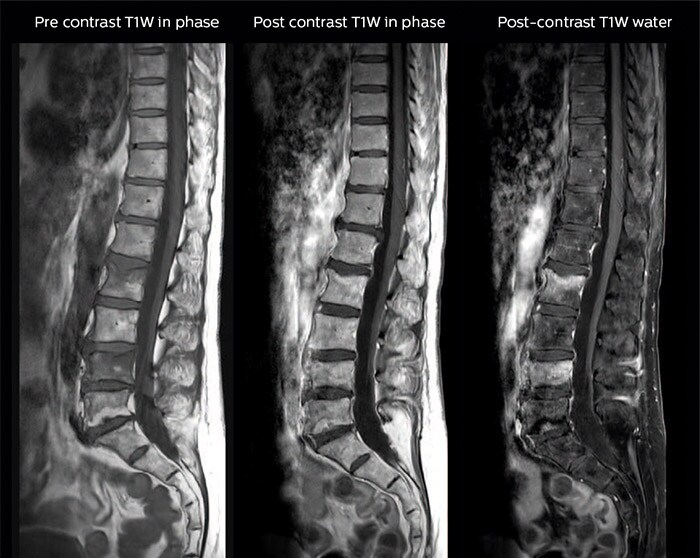
- Magnetic resonance imaging (MRI): This imaging technique uses powerful magnets and radio waves to generate detailed images of the spine’s soft tissues, such as discs and ligaments.
- Computed tomography (CT) scan: CT scans combine X-ray images taken from different angles to create cross-sectional views of the spine, helping to detect bone abnormalities.
- Bone scan: A bone scan involves injecting a small amount of radioactive material into the bloodstream, which then accumulates in areas of increased bone activity, indicating possible osteoarthritis-related changes.
- Electromyography (EMG): EMG measures the electrical activity of muscles and nerves, helping to determine if nerve compression or damage is contributing to symptoms.
- Nerve conduction studies: This test evaluates the speed and strength of electrical signals as they travel along nerves, helping to identify nerve-related abnormalities.
- Joint aspiration: In this procedure, a needle is used to extract fluid from the affected joint for analysis, which can help rule out other causes of joint pain.
- Blood tests: Although there is no specific blood test to diagnose osteoarthritis, blood tests can help rule out other conditions with similar symptoms, such as rheumatoid arthritis or infection.
- Erythrocyte sedimentation rate (ESR): An elevated ESR level can indicate the presence of inflammation in the body.
- C-reactive protein (CRP): Elevated CRP levels are also associated with inflammation and can be useful in ruling out other conditions.
- Rheumatoid factor (RF): RF is a blood marker that can help differentiate osteoarthritis from other types of arthritis, such as rheumatoid arthritis.
- Antinuclear antibody (ANA) test: ANA tests can help rule out other autoimmune diseases.
- HLA-B27 test: This genetic test can be helpful in diagnosing conditions like ankylosing spondylitis, which can present with similar symptoms.
- Urinalysis: This test can help identify any underlying kidney problems that may contribute to joint symptoms.
- Ultrasound: Ultrasound imaging uses sound waves to produce images of soft tissues and can assist in evaluating joint inflammation or fluid accumulation.
- Flexion and extension X-rays: These specialized X-rays assess the spine’s range of motion and stability.
- Discography: This test involves injecting a contrast dye into the discs to assess their integrity and identify potential sources of pain.
- Myelogram: A myelogram is a diagnostic procedure in which contrast dye is injected into the spinal canal, followed by X-rays or CT scans to evaluate the spinal cord and nerve roots.
- Bone density test: This test, known as a dual-energy X-ray absorptiometry (DXA) scan, measures bone density to assess the risk of osteoporosis, which can contribute to spinal degeneration.
- Functional assessment: Physical therapists or occupational therapists may assess functional abilities, such as flexibility, mobility, and strength, to evaluate the impact of osteoarthritis on daily activities.
- Visual analog scale (VAS): The VAS is a subjective pain assessment tool that allows individuals to rate the severity of their pain on a scale.
- Oswestry Disability Index: This questionnaire evaluates the impact of spinal pain on daily functioning and quality of life.
- SF-36 Health Survey: The SF-36 assesses overall health and functioning in various domains, providing a comprehensive picture of the impact of osteoarthritis on a person’s well-being.
- Spinal mobility tests: These tests measure the range of motion of the spine and can help identify limitations caused by osteoarthritis.
- Grip strength test: Assessing grip strength can provide insight into the functional impact of osteoarthritis in the hands and fingers.
- Tinetti Performance-Oriented Mobility Assessment: This assessment evaluates balance and gait, which can be affected by osteoarthritis-related joint changes.
- Slump test: This test helps evaluate the presence of nerve root compression or irritation in the spine.
- 24-hour ambulatory blood pressure monitoring: This test may be ordered to assess the impact of pain on blood pressure regulation.
It’s important to note that not all these tests may be necessary in every case, and the specific diagnostic approach may vary depending on individual circumstances. Consulting with a healthcare professional is crucial to determine the appropriate diagnostic strategy for a particular case of osteoarthritis of the spine.
Treatments for Osteoarthritis of the Spine
There is no cure for osteoarthritis, but there are many treatments that can relieve symptoms and significantly improve the quality of life.
The goals of osteoarthritis treatment are to reduce pain and improve joint function. Treatment approaches include
American College of Rheumatology guidelines
The American College of Rheumatology (ACR) has issued guidelines for the pharmacologic treatment of osteoarthritis of the hand, hip, and knee. For hand osteoarthritis, the ACR conditionally recommends using one or more of the following
-
Topical capsaicin
-
Topical nonsteroidal anti-inflammatory drugs (NSAIDs), including trolamine salicylate
The ACR conditionally recommends against using intra-articular therapies or opioid analgesics for hand osteoarthritis. For patients 75 years and older, the ACR conditionally recommends the use of topical rather than oral NSAIDs.
For knee osteoarthritis, the ACR conditionally recommends using one of the following:
-
Acetaminophen
-
Oral NSAIDs
-
Topical NSAIDs
-
Tramadol
-
Intra-articular corticosteroid injections
The ACR conditionally recommends against using chondroitin sulfate, glucosamine, or topical capsaicin for knee osteoarthritis. The ACR has no recommendations regarding the use of intra-articular hyaluronates, duloxetine, and opioid analgesics.
For hip osteoarthritis, the ACR conditionally recommends using one or more of the following for initial management:
The ACR conditionally recommends against using chondroitin sulfate or glucosamine for hip osteoarthritis. The ACR has no recommendation regarding the use of topical NSAIDs, intra-articular hyaluronate injections, duloxetine, or opioid analgesics.
American Academy of Orthopaedic Surgeons guidelines
-
Tramadol
The AAOS was unable to recommend for or against the use of the following for symptomatic knee osteoarthritis
-
Opioids
-
Pain patches
The recommendation on acetaminophen is a downgrade from the previous AAOS guideline and reflects the use of new criteria that resulted in the selection of only one study, which found no statistical significance or minimum clinically important improvement with acetaminophen compared with placebo.
The AAOS does not recommend treatment with any of the following
-
Intra-articular hyaluronic acid
-
Glucosamine and/or chondroitin sulfate or hydrochloride
New Guidelines
In 2012, the American College of Rheumatology (ACR) released updated recommendations for drug and non-drug treatment of hand, knee, and hip osteoarthritis. Key points include:
- The recommendations emphasize the early use of non-drug treatments, especially aerobic, aquatic, and resistance exercise. Overweight patients are encouraged to lose weight. While not strongly recommended, the ACR considers tai chi, acupuncture, and transcutaneous electrical stimulation (TENS) appropriate options for some patients.
- For patients older than 75 years old, the ACR recommends skin-applied (topical) NSAIDs instead of oral NSAIDs. For older patients, topical NSAIDs pose fewer risks for stomach bleeding and other side effects. (However, see Drug Warning below.)
- Topical capsaicin, a pain reliever derived from chili pepper, is recommended for hand osteoarthritis but not knee or hip osteoarthritis.
- The ACR does not recommend the use of glucosamine and chondroitin supplements.
Agency for Healthcare Research and Quality findings
A comparison of analgesics for osteoarthritis carried out by the Agency for Healthcare Research and Quality (AHRQ) found that “no currently available analgesic reviewed in this report offers a clear overall advantage compared with the others. The choice of analgesic for an individual patient should take into account the trade-off between benefits and adverse effects, which differs across analgesics. Patient age, comorbid conditions, and concomitant medication are key considerations.
The AHRQ comparison found that acetaminophen was modestly inferior to NSAIDs in reducing osteoarthritis pain but was associated with a lower risk of GI adverse effects. On the other hand, acetaminophen poses a higher risk of liver injury.
AHRQ findings on adverse effects included the following
-
Selective NSAIDs as a class were associated with a lower risk of ulcer complications than were the nonselective NSAIDs naproxen, ibuprofen, and diclofenac
-
The partially selective NSAIDs meloxicam and etodolac were associated with a lower risk of ulcer-related complications and symptomatic ulcers than were various nonselective NSAIDs
-
The risk of serious GI adverse effects was found to be higher with naproxen than with ibuprofen
-
Celecoxib and the nonselective NSAIDs ibuprofen and diclofenac were associated with an increased risk of cardiovascular adverse effects when compared with the placebo
-
The nonselective NSAIDs ibuprofen and diclofenac, but not naproxen, were associated with an increased risk of heart attack when compared with placebo
The AHRQ noted that topical diclofenac was found to have efficacy similar to that of oral NSAIDs in patients with localized osteoarthritis. No head-to-head trials compared topical salicylates or capsaicin with oral NSAIDs for osteoarthritis.
Medications
The goal of treatment is to decrease pain and increase mobility.
- Acetaminophen – is the first choice for treating osteoarthritis pain. (Acetaminophen may be less effective than NSAIDs in reducing moderate-to-severe pain.) Because acetaminophen has fewer side effects, most doctors suggest trying this drug first, then switching to an NSAID if acetaminophen does not provide sufficient pain relief.
- Analgesics – Prescription-strength drugs that relieve pain but not inflammation.
- Antidepressants – Drugs that block pain messages from your brain and boost the effects of endorphins (your body’s natural painkillers).
- Medication – Common pain remedies such as aspirin, acetaminophen, ibuprofen, and naproxen can offer short-term relief. All are available in low doses without a prescription. Other medications, including muscle relaxants and anti-seizure medications, treat aspects such as muscle spasms and damaged nerves.
- Corticosteroid injections – Your doctor will inject a steroid such as prednisone into your thumb joints. Steroids make the inflammation go down. However, because of side effects, they are used sparingly.
- Anesthetics – Used with precision, an injection of a “nerve block” can stop the pain for a time.
- Muscle Relaxants – These medications provide relief from spinal muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications –These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation in the skin.
- Calcium & vitamin D3 – to improve bone health and healing fracture.
- Glucosamine & diacerein – can be used to tighten the loose tension and regenerate cartilage or inhabit the further degeneration of cartilage.
- Muscle relaxants – such as cyclobenzaprine might be prescribed to relieve the discomfort associated with muscle spasms. However, these medicines might cause confusion in older people. Depending on the level of pain, prescription pain medicines might be used in the initial period of treatment.
- Over-the-counter – non-narcotic pain relievers and anti-inflammatory medications are usually the first choices of therapy for arthritis of the knee. Acetaminophen is a simple, over-the-counter pain reliever that can be effective in reducing arthritis pain that is following
- Glucose Amaine with Chondroitin Sulphate – Glucosamine and chondroitin have been widely promoted as a treatment for OA. Glucosamine, an amino sugar, is thought to promote the formation and repair of cartilage. Chondroitin, a carbohydrate, is a cartilage component that is thought to promote water retention and elasticity and to inhibit the enzymes that break down cartilage. Both compounds are manufactured by the body. Glucosamine supplements are derived from shellfish shells; chondroitin supplements are generally made from cow cartilage.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs) – Nonsteroidal anti-inflammatory drugs (NSAIDs) block prostaglandins, the substances that dilate blood vessels and cause inflammation and pain. There are dozens of NSAIDs available
- Oral NSAIDs should be used only for a short period of time. Long-term use of NSAIDs does not delay the progression of osteoarthritis and can increase patients’ risk of side effects.
Patients should use only the lowest effective dose because high dosages of NSAIDs can cause heart problems (such as increased blood pressure and risk of heart attack), kidney problems, and stomach bleeding. Because of these risks, the American College of Rheumatology recommends using topical NSAIDs in place of oral NSAIDs for patients 75 years and older.
Patients who take daily low-dose aspirin for heart protection should consider using an oral NSAID other than ibuprofen. Ibuprofen may make the aspirin less effective.
Patients who are at increased risk of stomach bleeding and ulcers should either switch to another type of pain reliever, or take the NSAID along with a proton-pump inhibitor drug, such as omeprazole (Prilosec, generic) or esomeprazole (Nexium), an H2 blocker such as famotidine (Pepcid, generic), or with the synthetic prostaglandin misoprostol (Cytotec, generic). (Misoprostol can cause miscarriage and should not be used by women who may be pregnant.) Some NSAIDs are available as combination pills; they include diclofenac/misoprostol (Arthrotec) and ibuprofen/famotidine (Duexis)

www.rxharun.com
Prescription analgesic medications include
- Tramadol
- Celecoxib
- Topical or Oral Diclofenac
- Oral Steroids
- Topical Capsaicin
- Hyaluronic Acid Injections
There are several alternatives to prescription medications. Although I use Voltaren Gel and Ultram, I also use alternatives that have alleviated the constant need for prescription analgesics.
Capsaicin and Other Topical Products
Capsaicin is a component of hot red peppers and may bring pain relief when used as a skin cream (Zostrix, generic). This is the only skin preparation that does more than just mask pain or reduce it temporarily. Capsaicin seems to reduce a substance in the body, known as substance P, which contributes both to inflammation and the delivery of pain impulses from the central nervous system.
A small amount of capsaicin must be applied to the area of inflammation about four times a day. During the first few days of use, the patient will experience a warm, stinging sensation when the cream is applied. This sensation goes away, and pain relief usually begins within 1 – 2 weeks. The American College of Rheumatology recommends topical capsaicin for hand osteoarthritis but not for knee or hip osteoarthritis.
Topical over-the-counter joint pain relievers that contain menthol, methyl salicylate, and (less commonly) capsaicin may in rare cases cause chemical burns. Menthol and methyl salicylate products are sold under brand names such as Bengay, Flexall, Icy Hot, and Mentholatum. Products that contain capsaicin include Capzasin as well as Zostrix. The risks appear more severe for combination products that contain higher doses of both menthol (greater than 3%) and methyl salicylate (greater than 10%). The FDA recommends:
- Don’t apply these products to damaged or irritated skin
- Don’t apply bandages, heating pads, or hot water bottles to areas treated with these products
- If you see any signs of blisters or burns, stop using the product and seek medical attention.
These warnings also apply to topical NSAID products that contain trolamine salicylate.
COX-2 Inhibitors (Coxibs)
Coxibs inhibit an inflammation-promoting enzyme called COX-2. This drug class was initially thought to provide benefits equal to NSAIDs but cause less gastrointestinal distress. However, following numerous reports of cardiovascular events, as well as skin rashes and other adverse effects, most COX-2 inhibitors were withdrawn from the market. Celecoxib is still available, but patients should discuss with their doctors whether this drug is appropriate and safe for them.
Duloxetine (Cymbalta)
Duloxetine (Cymbalta) is a serotonin-norepinephrine reuptake inhibitor (SNRI) antidepressant that is used to treat depression, anxiety disorders, diabetic nerve pain, and fibromyalgia. In 2010, the FDA approved duloxetine for the treatment of chronic musculoskeletal pain associated with osteoarthritis.
Tramadol
Tramadol (Ultram, generic) is a pain reliever that has been used as an alternative to opioids. It has opioid-like properties but is not as addictive. (Dependence and abuse have been reported, however.) It can cause nausea but does not cause severe gastrointestinal problems, as NSAIDs can. Some patients experience severe itching. A combination of tramadol and acetaminophen (Ultracet, generic) is available.
Narcotics
Narcotics, pain-relieving and sleep-inducing drugs that act on the central nervous system, are the most powerful medications available for the management of moderate-to-severe pain. There are two types of narcotics:
- Opiates, which are derived from natural opium (morphine and codeine)
- Opioids, which are synthetic drugs. They include oxycodone (such as Percodan, Percocet, Roxicodone, OxyContin, generic), hydrocodone (Vicodin, generic), oxymorphone (Numorphan, Opana), and fentanyl (Duragesic, generic)
Although the use of narcotics for arthritic pain is controversial, they may have a place in osteoarthritis treatment when milder drugs are not effective or appropriate. These drugs can be highly addictive and should be prescribed at the lowest possible effective dose.
Common side effects include anxiety, constipation, nausea and vomiting, dizziness, drowsiness, paranoia, urinary retention, restlessness, and labored or slow breathing.
Corticosteroid Injections
When pain becomes a major problem and less potent pain relievers are ineffective, doctors may try corticosteroid (steroid) injections, usually by giving the patient a shot in their joint every 3 months. Corticosteroid shots are useful only if inflammation is present in the joint. Relief from pain and inflammation is of short duration, and this treatment is rarely used for chronic osteoarthritis. These drugs may not be as effective for women as they are for men. The American College of Rheumatology does not recommend these injections for hand osteoarthritis.
Patients are usually advised not to have more than two or three injections a year since there is some concern that repeated injections over the long term may be harmful. Because long-term use of corticosteroids has many potentially serious side effects, steroid medications are never given by mouth or systemically for the treatment of osteoarthritis.
Hyaluronic Acid Injections (Viscosupplementation)
Injections of hyaluronic acid (such as Hyalgan, Synvisc, Artzal, and Nuflexxa) into the joint — a procedure called viscosupplementation — may provide pain relief for knee osteoarthritis. Relief usually lasts several months. The most common side effects, pain at the injection site and knee pain and swelling, are usually mild and temporary. Some studies report that these injections provide only very modest pain relief at best.
Spinal Injections
Spinal injections are sometimes used when pain does not respond to non-invasive treatments. A mixture of a corticosteroid (a powerful anti-inflammatory) and a local anesthetic is used in spinal injections. Many people experience relief from one injection, others may need up to three. Results vary widely with many people receiving relief that lasts from a few weeks to a few months. The injection is sometimes ineffective in relieving pain. There are rare but serious risks involved.
- Facet Joint Injections – In moderate to advanced arthritis, where inflammation is causing severe pain and restricted mobility, injections of corticosteroids into the affected facet joints (spinal joints) may be given. Some people experience relief that lasts up to three months, though results vary widely.
- Epidural Steroid Injection (ESI) – An injection into the epidural space – the narrow space between the membranes covering the spinal cord and the wall of the spinal canal. The medication travels up and down the epidural space to coat the facet joints and the spinal nerves near the area of the injection.
Your physical therapist can help with a variety of treatment options, including
Exercise
Joints need the motion to stay healthy. Long periods of inactivity cause the arthritic joint to stiffen and the adjoining tissue to atrophy (waste away). A moderate exercise program that includes low-impact aerobics and power and strength training has benefits for patients with osteoarthritis, even if exercise does not slow down the disease progression. Exercise helps
- Reduce stiffness and increase flexibility. It may also help improve the strength and elasticity of knee cartilage.
- Promote weight loss.
- Improve strength, which in turn improves balance and endurance.
-
Reduce stress and improve feelings of well-being, which helps patients cope with the emotional burden of pain.
Caution – Please consult your physical therapist or doctor before starting any exercise program.
Stretching – Your physical therapist will prescribe specific stretching exercises for your spine, arms, or legs based on the results of your initial evaluation. Obese individuals are in special need of stretching and exercises. Combined with strengthening, stretching may help slow the progression of the disease.
Symptom management – Symptom management means learning to feel better and remain active. Sometimes people are fearful that increased activity will worsen their symptoms or increase their pain. Your physical therapist will help you learn how to be more active without worsening your symptoms. He or she will help you find your appropriate activity levels and develop a unique program to keep you moving.
Daily activity training – Your physical therapist can teach you how to get in and out of bed, in and out of the bathtub, or out of a chair, and how to bend and walk with more ease.
Use of modalities – Treatment “modalities” such as heat or ice may be used to help manage your symptoms.
Manual therapy – Your physical therapist may use gentle hands-on techniques (manual therapy) to help improve your spinal flexibility and ease stiffness.
Balance and walking training – Exercises and instruction may be used to improve your balance safely and reduce your risk of falls.
Specialized braces or taping – Your physical therapist may use taping or specialized braces to help support your joints. Back bracing is used most in more advanced conditions.
Weight control – If you are obese, you are likely to have more spinal impairment in your upper back. Your physical therapist can help you improve your activity levels, and refer you to nutritional experts.
Remember, all cases of OA of the spine are different. Your physical therapist will choose the best treatment options for you based on his or her evaluation of your specific problem.
Exercise especially helps patients with mild-to-moderate osteoarthritis in the hip or in the knee. Many patients who begin an aerobic or resistance exercise program report less disability and pain. They are better able to perform daily chores and remain more independent than their inactive peers. Older patients and those with medical problems should always check with their doctors before starting an exercise program.

Three types of exercise are best for people with osteoarthritis:
- Strengthening and resistance exercise
- Range-of-motion exercise
-
Aerobic, or endurance, exercise
Strengthening and Resistance Exercise
Strengthening exercises include isometric exercises (pushing or pulling against static resistance). Isometric training builds muscle strength while burning fat, helps maintain bone density, and improves digestion. For patients with arthritis in the hip or knees, exercises that strengthen the muscles of the upper leg are important.
Exercise, such as weightlifting, helps build muscle that is usually lost with age and puts stress on bones, helping keep them strong and healthy.
Range-of-Motion Exercise
These exercises increase the amount of movement in the joints. In general, they are stretching exercises. The best examples are yoga and tai chi, which focus on flexibility, balance, and proper breathing.
Aerobic Exercise
Aerobic exercises help control weight and may reduce inflammation in some joints. Low-impact workouts also help stabilize and support the joint. Cycling and walking are beneficial, and swimming or exercising in water is highly recommended, for people with arthritis. (Patients with osteoarthritis should avoid high-impact sports, such as jogging, tennis, and racquetball if they cause pain.
Occupational Therapy
In addition to exercise, treatment of muscles and joints by a physical therapist can be helpful. An occupational therapist can show you ways to perform daily tasks of living without putting stress on your joints. Your therapist can recommend how to make changes in your workplace or work tasks to avoid repetitive or damaging motions.
Weight Reduction
Overweight patients with osteoarthritis can lessen the shock on their joints by losing weight. Knees, for example, sustain an impact three to five times the body weight when descending stairs. Losing 5 pounds of weight can eliminate 20 pounds of stress on the knee. The greater the weight loss, the greater the benefit.
Heat and Ice
Ice. When a joint is inflamed (particularly in the knee) applying ice for 20 – 30 minutes can be helpful. If an ice pack is not available, a package of frozen vegetables works just as well.
Heat Treatments. Soaking in a warm bath or applying a heating pad may help relieve stiffness and pain.
Mechanical Aids
A wide variety of devices are available to help support and protect joints. They include splints or braces, and shoe inserts or orthopedic shoes. A commonly used brace for knee osteoarthritis that involves only one side of the knee joint is called an offloading brace.
Assistive Devices
There are many different types of assisted devices that can help make your life easier in the home. Kitchen gadgets, such as jar openers, can assist with gripping and grabbing. Door-knob extenders and key turners are helpful for patients who have trouble turning their wrists. Bathrooms can be fitted with shower benches, grip bars, and raised toilet seats. An occupational therapist can advise you on choosing the right kinds of assistive devices.
Acupuncture
Acupuncture for neck and back pain seems to work to alleviate current pain, but it doesn’t have any significant long-term effects. Physical therapy, on the other hand, does have long-term benefits. It also offers immediate relief for symptoms.
Manual traction performed by a skilled physical therapist can alleviate quite a bit of pain by opening up the compressed discs. Physical therapy can also help build muscles around the vertebral column, which can keep the vertebrae open after manual traction.
Pain Management
Relaxation techniques such as guided imagery and breathing exercises may help some patients better cope with chronic pain.
Acupuncture, Transcutaneous Electric Nerve Stimulation (TENS), Therapeutic Ultrasound, and Massage
Some patients use acupuncture to reduce osteoarthritis pain. The technique is painless and involves the insertion of small fine needles at select points in the body. Some studies have found that acupuncture can help provide short-term pain relief for knee osteoarthritis.
Transcutaneous electric nerve stimulation (TENS) uses low-level electrical pulses to suppress pain. A variant (sometimes called percutaneous electrical nerve stimulation, or PENS) applies these pulses through a small needle to acupuncture points. Some patients with knee osteoarthritis find this treatment helpful.
Ultrasound therapy uses high-energy sound waves to produce heat within the tissue, which may help reduce inflammation, relieve pain, and improve function. Therapeutic ultrasound is usually performed by a physical therapist using an ultrasound machine. The therapist applies gel to the affected area and moves a handheld ultrasound transducer over the joint. Some evidence suggests that therapeutic ultrasound may be beneficial for patients with knee osteoarthritis.
Massage therapy may also help provide short-term pain relief. It is important to work with an experienced massage therapist who understands how not to injure sensitive joint areas.
Herbs and Dietary Supplements
Glucosamine and Chondroitin
Glucosamine hydrochloride and chondroitin sulfate are natural substances that are part of the building blocks found in and around cartilage. For many years, researchers have been studying whether these dietary supplements really work for relieving osteoarthritis pain. Earlier studies suggested a potential benefit from these supplements.
However, several recent high-quality studies involving large numbers of patients have indicated that glucosamine and chondroitin, either alone or in combination, do not seem to work any better than a placebo for relieving symptoms of osteoarthritis. Based on these studies, the American College of Rheumatology does not recommend the use of these supplements. Some doctors suggest a trial period of three months to see if glucosamine and chondroitin work. If the patient does not experience any benefit, the supplements should be discontinued.
S-adenosylmethionine (SAMe)
S-adenosylmethionine (SAMe, pronounced “Sammy”) is a synthetic form of a natural byproduct of the amino acid methionine. It has been marketed as a remedy for arthritis, but scientific evidence supporting these claims is lacking.
Generally, manufacturers of herbal remedies and dietary supplements do not need FDA approval to sell their products. Just like a drug, herbs and supplements can affect the body’s chemistry, and therefore have the potential to produce side effects that may be harmful. There have been several reported cases of serious and even lethal side effects from herbal products. Always check with your doctor before using any herbal remedies or dietary supplements.
Arthroscopy and Debridement
Arthroscopy is performed to clean out bone and cartilage fragments (debridement) that, in theory at least, may cause pain and inflammation. It is also sometimes used to diagnose osteoarthritis. In this procedure, the surgeon makes a small incision and inserts the arthroscope, a pencil-width fiber-optic instrument that contains a light and magnifying lens. The arthroscope is attached to a miniature television camera that allows the surgeon to see the inside of the joint.
Research and debate continue on whether arthroscopy provides true benefits for those with osteoarthritis and, if so, which patients may benefit the most from it. Arthroscopy is most likely to benefit people with mild-to-moderate osteoarthritis who have evidence of bone and cartilage fragments in the joint, or patients whose joints lock or catch with movements
Joint Replacement (Arthroplasty)
When osteoarthritis becomes so severe that pain and immobility make normal functioning impossible, many people become candidates for artificial (prosthetic) joint implants using a procedure called arthroplasty. Hip replacement is the most established and successful replacement procedure, followed by knee replacement. Other joint surgeries (such as shoulders, elbows, wrists, and fingers) are less common, and some arthritic joints (in the spine, for instance) cannot yet be treated in this manner. When two joints, such as both knees, need to be replaced, having the operations done sequentially rather than at the same time may result in fewer complications
Candidates. The primary indications for surgery are pain and significant limitations of movement, including walking, that cannot be treated by less invasive therapies.
Patients who may not be good candidates are those with the following conditions:
- Severe neurologic, emotional, or mental disorders
- Severe osteoporosis
- Other chronic medical conditions
- Obesity
Surgeons often prefer to delay prosthetic implantation in younger patients, because implants wear out and the patient will need at least one revision procedure later on. Newer, longer-lasting materials, however, may help reduce the rate of revision operations.
Elderly patients with poorly controlled osteoarthritis often do very well after joint replacement surgery. While full recovery may take older patients longer to achieve than younger people, the long-term outcome of the surgery is usually excellent and can lead to significant improvements in pain and quality of life.
Complications
- Complications can occur, and, although uncommon, some can be life-threatening. In addition to blood loss and infection, deep blood clots in the legs (deep venous thrombosis) are a serious potential complication. These clots can potentially travel to the lungs (pulmonary embolism) and pose a risk of death. Patients who are overweight are at higher than average risk for blood clots.
- Recovery and Rehabilitation. Aside from the surgeon’s skill and the patient’s underlying condition, the success rate depends on the kind and degree of activity the joint receives following replacement surgery. Physical therapy takes about 6 weeks to rebuild adjoining muscles and strengthen surrounding ligaments. Patients typically experience considerable pain during this time.
- While many patients find that joint replacement eventually provides pain relief and restores some mobility, they need time to adjust to the artificial joint.
Limitations after hip surgery include:
- Usually, patients with new hips are able to walk several miles a day and climb stairs, but they cannot run.
- Prosthetic hips should not be flexed beyond 90 degrees, so patients must learn new ways to perform activities requiring bending down (like tying a shoe).
Limitations after knee surgery include:
- Walking distance improves after knee replacement surgery, but patients still cannot run.
- Artificial knee joints generally have a limited range of motion of just 110 degrees and stair climbing may remain difficult.
Minimally Invasive Arthroplasty – Surgeons are exploring a variety of new techniques for a “minimally invasive” approach to knee and hip arthroplasty. They include using a shorter incision, and new types of smaller specialized instruments. The goal is to give the patient a shorter recovery time and less postoperative pain. However, minimally invasive arthroplasty is still in its early stages. At this time, there is no consensus on which minimally invasive technique works best, or if it actually achieves any additional benefits beyond the recovery period.
Hip Resurfacing – Hip resurfacing is a surgical alternative to total hip replacement. It involves scraping the surfaces of the hip joint and femur and placing a metal cap over the bone. The procedure preserves much of the bone so that a standard hip replacement can be done years later if needed. It may provide more stability, a faster recovery, and greater range of motion, making it a potentially good option for young, physically active patients.
Revision Arthroplasty – A repair procedure called arthroplasty revision may be used in cases where the original transplant fails. The specific procedure depends on whether the bone defects that occurred are contained or uncontained.
- Contained defects can be repaired with small bone grafts, the use of cement, or oversized cementless implants as required.
- Uncontained defects are more severe and may require a large bone graft or specially constructed implants to restore bone.
If a second arthroplasty is required, the potential for complications is magnified: more bone is cut, more blood is lost, and the operation takes longer. Patients are also generally older and more vulnerable to complications.
Realigning Bones (Osteotomy)
Osteotomy is a surgical procedure used to realign bone and cartilage and reposition the joint. If only a certain section (the medial compartment) of the knee is damaged and deformed by osteoarthritis, the surgeon may choose to perform an osteotomy:
Lifestyle Changes
Many people don’t know that animal products (such as meat, milk, and cheese) cause the pH of the body to become more acidic. To neutralize this change in pH balance, the body strips calcium from the bones.
For those who already have osteoarthritis, this exacerbates the problem. It can also increase the risk for those who have not developed the disease. Reducing the number of animal products in the diet (or better yet, going vegetarian or vegan) can have a huge impact on the symptoms of osteoarthritis and its prevention.
Obesity is another problem. Being overweight puts more strain on the joints as well as the vertebral column, especially the lower back, that is natural. Losing even a few pounds can make a considerable difference in pain levels, and progression of the disease.
Health Tips Osteoarthritis of the spine
The aims of treatment for spinal osteoarthritis are to manage your pain, maintain your mobility and, where possible, prevent it from worsening. Helpful strategies may include:
- Educating yourself about back pain – ask your doctor to point you in the direction of reputable sources of information
- Regular, low-impact exercise (with your doctor’s approval), such as walking, swimming, or cycling
- Sleeping on a supportive mattress and using supportive chairs
- Weight loss if required
- Over-the-counter medications like paracetamol or ibuprofen
- Prescription anti-inflammatory medications
- Strong pain medication, which should only be used for short periods of time to relieve very high levels of pain
- Relaxation therapy, such as meditation, visualization, and special breathing
- Acupuncture
- Injections into the epidural space, facet joints or to block specific spinal nerves – are usually performed under the guidance of a special x-ray machine.
Talk to your doctor about the most suitable strategies for you.
References












