Pancreatic cancer is a type of cancer that starts in the pancreas, an organ located deep inside your abdomen. The pancreas plays a crucial role in digestion and blood sugar control. When cells in the pancreas begin to grow out of control, they can form a tumor, which can be cancerous.
Types of Pancreatic Cancer
There are two main types of pancreatic cancer: exocrine tumors and endocrine tumors.
Exocrine tumors: These are the most common type and start in the cells that make digestive juices. They are often found in the ducts of the pancreas.
Endocrine tumors: These are much rarer and begin in the hormone-producing cells of the pancreas.
Or
Each type behaves differently and requires unique treatment approaches.
1. Pancreatic Adenocarcinoma
Pancreatic adenocarcinoma is the most common type of pancreatic cancer, accounting for approximately 85% of all cases. It primarily starts in the exocrine cells of the pancreas, which are responsible for producing digestive enzymes.
This type of cancer often doesn’t show symptoms in its early stages, which is why it’s usually diagnosed at an advanced stage. Treatment typically involves surgery, chemotherapy, and radiation therapy.
2. Pancreatic Neuroendocrine Tumors (PNETs)
Pancreatic neuroendocrine tumors, or PNETs, are a less common type of pancreatic cancer, making up only about 5% of cases. These tumors originate from the endocrine cells of the pancreas, which produce hormones like insulin and glucagon.
Unlike adenocarcinoma, PNETs often grow more slowly and may not cause symptoms until they reach a larger size. Surgery is the primary treatment, and in some cases, medications can help manage hormone production.
3. Acinar Cell Carcinoma
Acinar cell carcinoma is an extremely rare form of pancreatic cancer, accounting for less than 1% of cases. It starts in the acinar cells of the pancreas, which produce digestive enzymes.
This type of cancer can be more aggressive than other pancreatic cancers, and treatment usually involves surgery, chemotherapy, and sometimes targeted therapy.
4. Intraductal Papillary Mucinous Neoplasms (IPMNs)
IPMNs are precancerous growths that can develop in the pancreatic ducts. While not cancer themselves, they can progress to cancer if left untreated.
Treatment often involves surgery to remove the IPMN or a portion of the pancreas, especially if the growth shows signs of becoming cancerous.
5. Mucinous Cystic Neoplasms (MCNs)
Similar to IPMNs, MCNs are cystic growths that can develop in the pancreas. They are also considered precancerous.
Treatment usually involves removing the cyst or, in some cases, part of the pancreas. Monitoring is essential because MCNs can become cancerous.
6. Solid Pseudopapillary Neoplasms (SPNs)
Solid pseudopapillary neoplasms are rare, slow-growing tumors that typically affect young women. While they’re usually less aggressive than other types of pancreatic cancer, they still require treatment.
Treatment usually involves surgery to remove the tumor. Fortunately, SPNs tend to have a good prognosis.
7. Pancreatic Lymphoma
Pancreatic lymphoma is a rare form of pancreatic cancer that originates in the lymphatic tissue of the pancreas.
Treatment typically involves chemotherapy and sometimes radiation therapy. The prognosis can vary depending on the type and stage of the lymphoma.
8. Metastatic Pancreatic Cancer
Metastatic pancreatic cancer is not a distinct type but rather refers to cancer that has spread from the pancreas to other parts of the body, such as the liver, lungs, or lymph nodes.
Treatment for metastatic pancreatic cancer often involves chemotherapy, targeted therapy, and sometimes surgery or radiation therapy to manage symptoms.
The following stages are used for pancreatic cancer:
Stage 0 (Carcinoma in Situ)
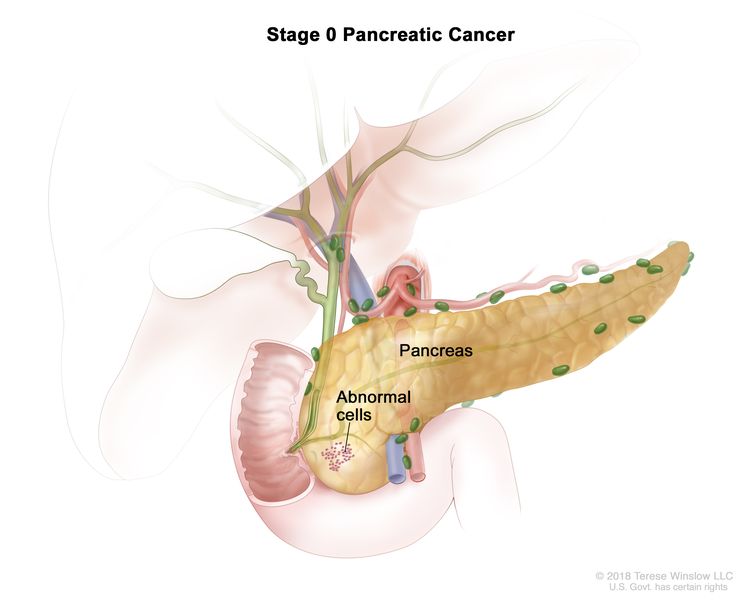
In stage 0, abnormal cells are found in the lining of the pancreas. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.
Stage I
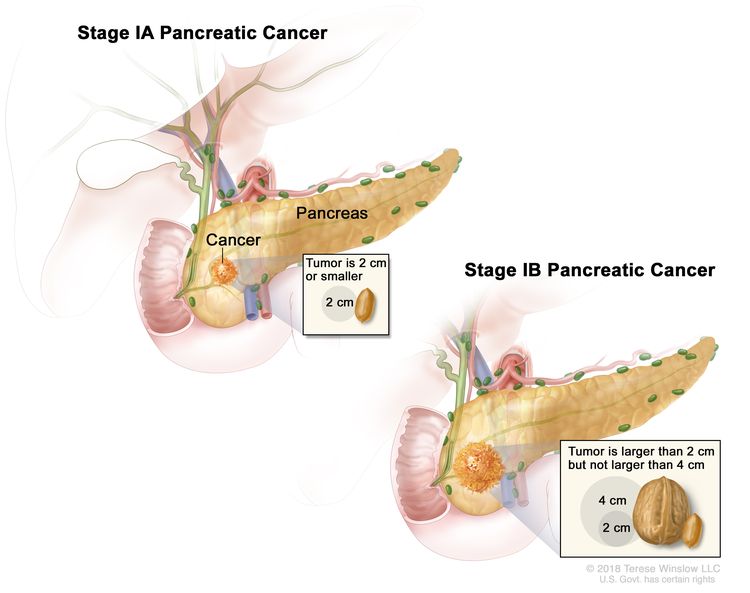
In stage I, cancer has formed and is found in the pancreas only. Stage I is divided into stages IA and IB, depending on the size of the tumor.
- Stage IA: The tumor is 2 centimeters or smaller.
- Stage IB: The tumor is larger than 2 centimeters but not larger than 4 centimeters.
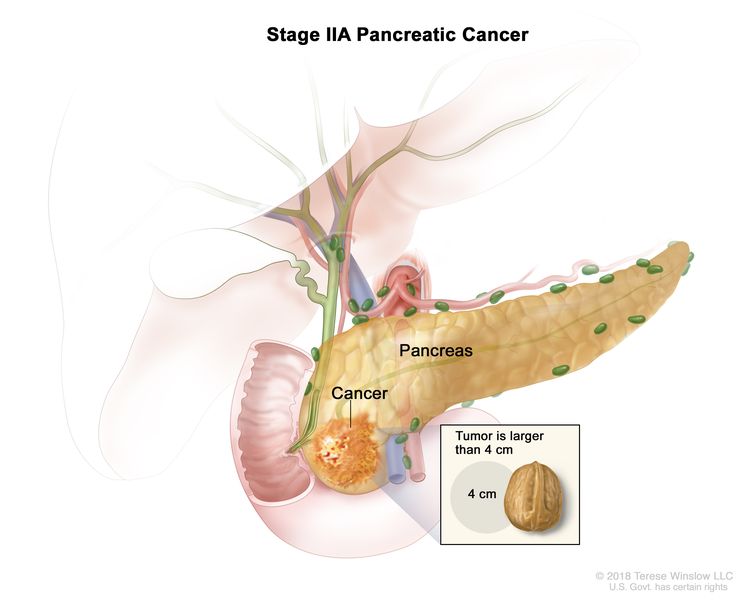
Stage II
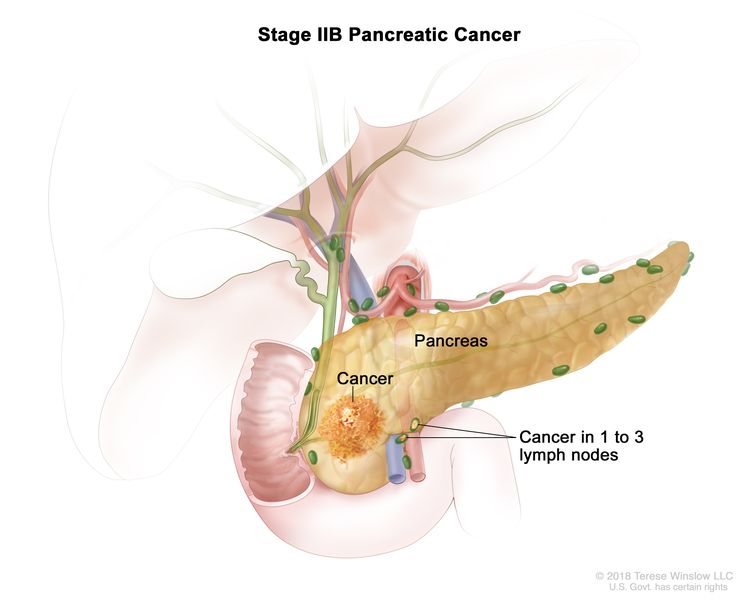
Stage II is divided into stages IIA and IIB, depending on the size of the tumor and where the cancer has spread.
- Stage IIA: The tumor is larger than 4 centimeters.

Stage IIA pancreatic cancer. The tumor is larger than 4 centimeters. - Stage IIB: The tumor is any size and cancer has spread to 1 to 3 nearby lymph nodes.

Stage IIB pancreatic cancer. The tumor is any size and cancer has spread to 1 to 3 nearby lymph nodes.
Stage III
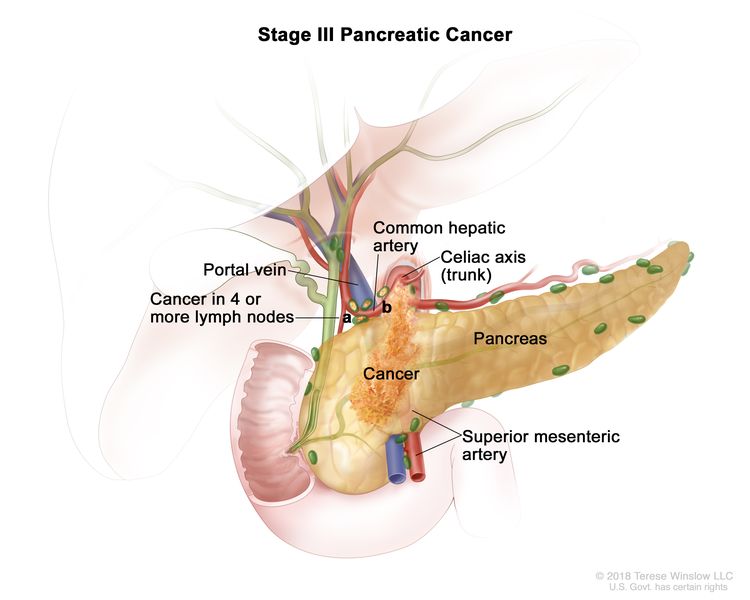
In stage III, the tumor is any size and cancer has spread to:
- four or more nearby lymph nodes; or
- the major blood vessels near the pancreas.
Stage IV
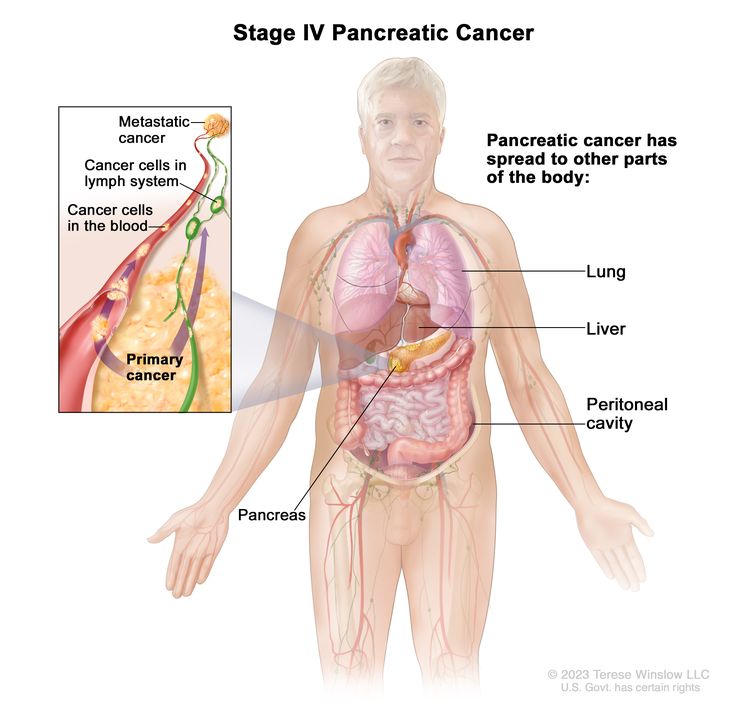
In stage IV, the tumor is any size and cancer has spread to other parts of the body, such as the liver, lung, or peritoneal cavity (the body cavity that contains most of the organs in the abdomen).
Causes
Common causes of pancreatic cancer in simple, plain English. By the end, you’ll have a better grasp of what you can do to protect yourself.
1. Smoking: Smoking is a major cause of pancreatic cancer. The chemicals in tobacco can damage your pancreas over time.
2. Age: As we grow older, our risk of developing pancreatic cancer increases. It’s more common in people over 65.
3. Family History: If someone in your family has had pancreatic cancer, your risk is higher. It may be linked to inherited genes.
4. Obesity: Being overweight puts extra stress on your pancreas and can increase your risk.
5. Diabetes: Long-term diabetes may raise your chances of developing pancreatic cancer. High blood sugar levels can harm the pancreas.
6. Chronic Pancreatitis: Inflammation of the pancreas over time can lead to cancer. Alcohol abuse is a common cause of chronic pancreatitis.
7. High Fat Diet: Diets high in fat, especially animal fats, may contribute to pancreatic cancer.
8. Red Meat Consumption: Eating a lot of red meat, like beef and pork, might increase your risk.
9. Low Fruit and Veggie Intake: Not getting enough fruits and vegetables in your diet may play a role.
10. Processed Meats: Sausages, hot dogs, and bacon contain chemicals that may increase the risk.
11. Alcohol: Excessive alcohol use can lead to chronic pancreatitis, raising cancer risk.
12. Chemical Exposure: Some workplace chemicals, like those in the dry-cleaning or metalworking industries, could be linked to pancreatic cancer.
13. Pesticides: Exposure to certain pesticides might contribute to the disease.
14. Gender: Men are slightly more likely to develop pancreatic cancer than women.
15. Race and Ethnicity: African Americans are at a higher risk than Caucasians, but the reasons aren’t clear.
16. Blood Group: Some studies suggest that people with blood group A may have a higher risk.
17. Certain Medications: Some drugs, like certain blood pressure medications, might raise the risk slightly.
18. Peptic Ulcers: A history of peptic ulcers could be a contributing factor.
19. Gallbladder Removal: Surgery to remove the gallbladder might increase the risk.
20. Hepatitis B Infection: Chronic infection with hepatitis B may be linked to pancreatic cancer.
21. Helicobacter pylori Infection: This stomach infection could potentially raise the risk.
22. Liver Cirrhosis: A damaged liver, often caused by excessive alcohol use, can increase risk.
23. Cystic Fibrosis: This genetic condition is associated with a higher risk of pancreatic cancer.
24. BRCA1 and BRCA2 Mutations: Mutations in these genes, often linked to breast and ovarian cancer, may also raise the risk.
25. Lynch Syndrome: People with this genetic condition are at an increased risk of several cancers, including pancreatic.
26. Hereditary Pancreatitis: Some rare genetic conditions can lead to chronic pancreatitis and an increased risk of cancer.
27. Radiation Exposure: High levels of radiation, like during cancer treatment, could potentially increase risk.
28. Estrogen Replacement Therapy: Long-term use of estrogen replacement therapy might slightly raise the risk.
29. Viral Infections: Some viruses, such as the Epstein-Barr virus, have been studied for their potential connection to pancreatic cancer.
30. Lack of Physical Activity: Leading a sedentary lifestyle may contribute to obesity, which is a known risk factor.
Symptoms
Common symptoms of pancreatic cancer
- Jaundice (Yellowing of the Skin and Eyes):
- Description: Jaundice makes your skin and the whites of your eyes turn yellow. It happens when the cancer blocks the bile duct, which affects the flow of bile, a digestive fluid.
- Jaundice in pancreatic cancer results from bile duct blockage, causing yellowing of the skin and eyes.
- Abdominal Pain:
- Description: Pancreatic cancer can cause pain in the upper or middle abdomen. It may be constant or come and go, and it can be mild or severe.
- Abdominal pain associated with pancreatic cancer varies in intensity and location.
- Unexplained Weight Loss:
- Description: Sudden and unexplained weight loss can be a sign of pancreatic cancer. You may lose weight without changing your diet or activity level.
- Pancreatic cancer may lead to unexpected weight loss even when eating habits remain unchanged.
- Loss of Appetite:
- Description: A reduced desire to eat is common in pancreatic cancer patients. This can contribute to weight loss and weakness.
- Pancreatic cancer often results in a decreased appetite, contributing to weight loss.
- Fatigue:
- Description: Pancreatic cancer can cause extreme tiredness or fatigue, which may not improve with rest.
- Fatigue in pancreatic cancer can be persistent and not alleviated by rest.
- Nausea and Vomiting:
- Description: Nausea and vomiting may occur, particularly if the cancer is blocking the digestive tract or affecting digestion.
- Pancreatic cancer-related nausea and vomiting can stem from digestive disruptions.
- Pale Stools and Dark Urine:
- Description: Pancreatic cancer can affect the color of your stools, making them pale, and cause your urine to become dark.
- Dark urine and pale stools may indicate pancreatic cancer due to changes in bile flow.
- Itchy Skin:
- Description: Itchy skin, also known as pruritus, can result from pancreatic cancer due to the buildup of bile salts in the body.
- Pancreatic cancer-related itching is caused by the accumulation of bile salts.
- New-Onset Diabetes:
- Description: Some individuals may develop diabetes suddenly when they have pancreatic cancer, as the pancreas is responsible for regulating blood sugar.
- Pancreatic cancer can trigger the onset of diabetes due to pancreas dysfunction.
- Back Pain:
- Description: Pancreatic cancer can cause pain in the upper back or between the shoulder blades. This pain may radiate to the front.
- Upper back pain, often radiating to the front, can be a symptom of pancreatic cancer.
- Indigestion:
- Description: Frequent indigestion or discomfort after eating may be a symptom, as the pancreas plays a crucial role in digestion.
- Pancreatic cancer can lead to recurring indigestion and post-meal discomfort.
- Changes in Bowel Habits:
- Description: Pancreatic cancer can affect the digestive process, leading to changes in bowel habits like diarrhea or constipation.
- Altered bowel habits, such as diarrhea or constipation, may be indicative of pancreatic cancer.
- Fever and Sweating:
- Description: Pancreatic cancer can sometimes cause fever and excessive sweating, especially at night.
- Fever and night sweats can be associated with pancreatic cancer.
- Enlarged Gallbladder:
- Description: An enlarged gallbladder, often detected during a physical examination, can be a sign of pancreatic cancer.
- An enlarged gallbladder can be a physical indicator of pancreatic cancer.
- Blood Clots:
- Description: Pancreatic cancer increases the risk of blood clots, which can lead to swelling, pain, and redness in the affected area.
- Blood clots are a potential complication of pancreatic cancer, causing swelling and pain.
- Depression and Anxiety:
- Description: The emotional toll of a pancreatic cancer diagnosis can lead to feelings of depression and anxiety.
- Pancreatic cancer can have emotional effects, including depression and anxiety.
- Enlarged Lymph Nodes:
- Description: Swollen lymph nodes, often detected during imaging tests, can be a sign that the cancer has spread.
- Enlarged lymph nodes may indicate the spread of pancreatic cancer.
- Weakness:
- Description: General weakness and a lack of energy can be a symptom of pancreatic cancer, impacting daily activities.
- Pancreatic cancer-related weakness can hinder daily activities.
- Bloating:
- Description: Abdominal bloating and discomfort can occur due to pancreatic cancer’s impact on digestion.
- Pancreatic cancer may lead to abdominal bloating and discomfort.
- Yellow or Greasy Stools:
- Description: Stools that are pale, yellow, or greasy can result from poor digestion, which can be caused by pancreatic cancer.
- Pancreatic cancer can lead to yellow or greasy stools due to impaired digestion.
Diagnosis and Tests
Common diagnosis and test methods used to identify pancreatic cancer explained in simple terms.
1. Physical Examination:
A doctor examines your body for any signs of discomfort, pain, or unusual changes that might suggest pancreatic issues.
2. Blood Tests:
Blood samples are checked for abnormal levels of certain chemicals, such as bilirubin or liver enzymes, which can indicate problems in the pancreas.
3. Imaging Techniques:
Doctors use various imaging tools like CT scans, MRIs, and ultrasounds to visualize the pancreas and surrounding areas for any abnormalities.
4. Biopsy:
A tiny sample of tissue is extracted from the pancreas and examined under a microscope to identify cancer cells.
5. Endoscopic Ultrasound (EUS):
A thin tube with an ultrasound probe is inserted through the mouth to create detailed images of the pancreas.
6. ERCP (Endoscopic Retrograde Cholangiopancreatography):
A tube is passed through the mouth to examine the bile ducts and pancreatic ducts for blockages or tumors.
7. Laparoscopy:
A small incision is made to insert a camera to visualize the pancreas and surrounding areas up close.
8. PET Scan (Positron Emission Tomography):
A radioactive substance is injected to highlight areas of potential cancer activity in the body.
9. MRCP (Magnetic Resonance Cholangiopancreatography):
MRI scans are used to create detailed images of the bile ducts and pancreatic ducts.
10. Blood Tumor Marker Test:
Blood is tested for specific proteins that may be elevated in the presence of pancreatic cancer.
11. CA19-9 Test:
A blood test to measure the levels of CA19-9, a marker that might be higher in pancreatic cancer patients.
12. Cytology:
Cells from the pancreas are examined under a microscope to detect any abnormalities.
13. Biopsy via ERCP:
During an ERCP procedure, a small tissue sample can be taken for biopsy.
14. Laparoscopic Ultrasound:
Combining laparoscopy and ultrasound to visualize the pancreas more clearly.
15. Percutaneous Biopsy:
Tissue samples are obtained using a needle inserted through the skin, guided by imaging techniques.
16. Blood Clotting Tests:
Pancreatic cancer can affect blood clotting factors, so these tests can provide additional diagnostic insights.
17. Abdominal Fluid Analysis:
Fluid extracted from the abdomen is analyzed for cancer cells or other abnormalities.
18. Genetic Testing:
Inherited gene mutations that increase pancreatic cancer risk can be identified through genetic tests.
19. Laparoscopic Biopsy:
Using laparoscopy to obtain larger tissue samples for more accurate biopsy results.
20. Fine-Needle Aspiration (FNA):
A thin needle is used to extract fluid or tissue from the pancreas for examination.
21. Laparoscopic Staging:
Determining the extent of cancer spread using laparoscopy.
22. Exploratory Surgery:
Surgery to visually inspect the pancreas and surrounding organs for signs of cancer.
23. Biopsy via EUS:
While conducting an endoscopic ultrasound, doctors can take biopsy samples.
24. Brush Cytology:
A brush is used to collect cell samples from the bile or pancreatic ducts for analysis.
25. Laparoscopic Liver Biopsy:
If cancer spread is suspected, a biopsy of the liver can provide valuable information.
26. Laparoscopic Peritoneal Lavage:
Checking for cancer cells in the abdominal cavity’s fluid.
27. Chest X-ray:
To see if cancer has spread to the lungs or chest.
28. Angiography:
Dye is injected into blood vessels to create detailed images and detect tumors.
29. Laparoscopic Biopsy of Lymph Nodes:
If cancer spread is suspected, nearby lymph nodes can be biopsied.
30. Laparoscopic Biopsy of Ascites:
If fluid accumulates in the abdomen, it can be tested for cancer cells.
The following tests and procedures may be used:
- Physical exam and health history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances, such as bilirubin, released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Tumor marker test: A procedure in which a sample of blood, urine, or tissue is checked to measure the amounts of certain substances, such as CA 19-9, and carcinoembryonic antigen (CEA), made by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the body. These are called tumor markers.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. A spiral or helical CT scan makes a series of very detailed pictures of areas inside the body using an x-ray machine that scans the body in a spiral path.
- PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do. A PET scan and CT scan may be done at the same time. This is called a PET-CT.
- Abdominal ultrasound: An ultrasound exam used to make pictures of the inside of the abdomen. The ultrasound transducer is pressed against the skin of the abdomen and directs high-energy sound waves (ultrasound) into the abdomen. The sound waves bounce off the internal tissues and organs and make echoes. The transducer receives the echoes and sends them to a computer, which uses the echoes to make pictures called sonograms. The picture can be printed to be looked at later.
- Endoscopic ultrasound (EUS): A procedure in which an endoscope is inserted into the body, usually through the mouth or rectum. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. This procedure is also called endosonography.
- Endoscopic retrograde cholangiopancreatography (ERCP): A procedure used to x-ray the ducts (tubes) that carry bile from the liver to the gallbladder and from the gallbladder to the small intestine. Sometimes pancreatic cancer causes these ducts to narrow and block or slow the flow of bile, causing jaundice. An endoscope (a thin, lighted tube) is passed through the mouth, esophagus, and stomach into the first part of the small intestine. A catheter (a smaller tube) is then inserted through the endoscope into the pancreatic ducts. A dye is injected through the catheter into the ducts and an x-ray is taken. If the ducts are blocked by a tumor, a fine tube may be inserted into the duct to unblock it. This tube (or stent) may be left in place to keep the duct open. Tissue samples may also be taken.
- Percutaneous transhepatic cholangiography (PTC): A procedure used to x-ray the liver and bile ducts. A thin needle is inserted through the skin below the ribs and into the liver. Dye is injected into the liver or bile ducts and an x-ray is taken. If a blockage is found, a thin, flexible tube called a stent is sometimes left in the liver to drain bile into the small intestine or a collection bag outside the body. This test is done only if ERCP cannot be done.
- Laparoscopy: A surgical procedure to look at the organs inside the abdomen to check for signs of disease. Small incisions (cuts) are made in the wall of the abdomen and a laparoscope (a thin, lighted tube) is inserted into one of the incisions. The laparoscope may have an ultrasound probe at the end in order to bounce high-energy sound waves off internal organs, such as the pancreas. This is called laparoscopic ultrasound. Other instruments may be inserted through the same or other incisions to perform procedures such as taking tissue samples from the pancreas or a sample of fluid from the abdomen to check for cancer.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. There are several ways to do a biopsy for pancreatic cancer. A fine needle or a core needle may be inserted into the pancreas during an x-ray or ultrasound to remove cells. Tissue may also be removed during a laparoscopy or surgery to remove the tumor.
Treatment
Different treatments for pancreatic cancer. Whether you’re a patient, a caregiver, or just looking to learn more, this guide aims to make these treatment options easy to understand.
1. Surgery: Surgery involves removing the tumor from the pancreas. This can be done if the cancer is contained and hasn’t spread. It’s like taking out the bad part to help the rest of the body stay healthy.
2. Chemotherapy: Chemotherapy is like strong medicine that travels through the body to kill cancer cells. It’s like an army going after the bad guys wherever they are.
3. Radiation Therapy: Radiation therapy uses special rays to target and destroy cancer cells. It’s like shining a light on the darkness to make it go away.
4. Immunotherapy: Immunotherapy helps the body’s own immune system fight cancer. It’s like giving the body extra soldiers to defeat the enemy.
5. Targeted Therapy: Targeted therapy targets specific molecules that help cancer grow. It’s like cutting the supply lines that feed the bad guys.
6. Palliative Care: Palliative care focuses on relieving symptoms and improving the quality of life. It’s like giving comfort and support to make things easier.
7. Clinical Trials: Clinical trials are research studies testing new treatments. It’s like trying out new tools to see if they work better.
8. Ablation Therapy: Ablation therapy uses heat or cold to destroy cancer cells. It’s like melting away the bad stuff.
9. Radiofrequency Ablation: Radiofrequency ablation uses heat to kill cancer cells. It’s like cooking the bad cells until they’re gone.
10. Cryoablation: Cryoablation uses cold to freeze and destroy cancer cells. It’s like freezing the bad cells until they’re no longer a threat.
11. Chemoradiotherapy: Chemoradiotherapy combines chemotherapy and radiation therapy. It’s like attacking the enemy from multiple sides at once.
12. Proton Therapy: Proton therapy uses protons to target and destroy cancer cells. It’s like using tiny, powerful arrows to hit the bullseye.
13. Whipple Procedure: The Whipple procedure removes the head of the pancreas, the gallbladder, and parts of other nearby organs. It’s like carefully removing a section of a puzzle.
14. Pancreatectomy: Pancreatectomy is the removal of all or part of the pancreas. It’s like taking out a damaged engine part to keep the car running.
15. Palliative Bypass Surgery: Palliative bypass surgery helps with symptoms by redirecting the flow of substances in the body. It’s like creating a detour around a roadblock.
16. Endoscopic Stent Placement: Stent placement uses a tube to keep pathways open. It’s like placing a small pipe to prevent clogs.
17. Total Pancreatectomy: Total pancreatectomy removes the entire pancreas. It’s like replacing a whole machine when fixing parts won’t work.
18. Partial Pancreatectomy: Partial pancreatectomy removes only the part of the pancreas with cancer. It’s like removing a slice of a pie.
19. Chemotherapy Pills: Instead of IV, some chemo comes in pill form. It’s like taking medicine at home to fight the bad cells.
20. Photodynamic Therapy: Photodynamic therapy uses special light to activate drugs that kill cancer cells. It’s like using a superhero flashlight to defeat villains.
21. Intensity-Modulated Radiation Therapy (IMRT): IMRT uses precise radiation doses to target cancer. It’s like using a laser pointer to hit specific spots.
22. Stereotactic Body Radiation Therapy (SBRT): SBRT delivers high doses of radiation to the tumor in a few sessions. It’s like using a sniper to take out the bad cells from a distance.
23. Nanoparticle Drugs: Nanoparticles are tiny particles that deliver drugs to cancer cells. It’s like sending tiny messengers to deliver a package to the enemy.
24. PARP Inhibitors: PARP inhibitors block proteins that help cancer cells repair themselves. It’s like jamming the enemy’s communication lines.
25. Angiogenesis Inhibitors: Angiogenesis inhibitors block the growth of blood vessels that feed tumors. It’s like cutting off the enemy’s food supply.
26. Monoclonal Antibodies: Monoclonal antibodies are proteins that target specific cancer cells. It’s like having a lock that only fits a certain key.
27. Personalized Vaccines: Personalized vaccines help the immune system recognize and fight cancer cells. It’s like giving the body a wanted poster to identify the bad guys.
28. Adoptive T Cell Therapy: T cell therapy boosts the immune system to attack cancer cells. It’s like training soldiers to fight a specific enemy.
29. Hedgehog Pathway Inhibitors: Hedgehog inhibitors block signals that promote cancer growth. It’s like putting a stop sign in front of the enemy.
30. MEK Inhibitors: MEK inhibitors interfere with cancer cell growth. It’s like disrupting the enemy’s assembly line.
Medications
Different drug treatments for pancreatic cancer in easy-to-understand language.
1. Gemcitabine (Gemzar)
Gemcitabine is a drug that targets fast-growing cancer cells by hindering their ability to replicate. It’s often used in combination with other drugs to enhance its effectiveness.
2. Abraxane (Paclitaxel Albumin-bound)
Abraxane works by disrupting cancer cell division, slowing down tumor growth. It’s given along with another drug called gemcitabine.
3. FOLFIRINOX
FOLFIRINOX is a combination treatment involving four drugs. It works by attacking cancer cells’ DNA and interfering with their ability to divide and multiply.
4. Erlotinib (Tarceva)
This drug blocks signals that stimulate cancer growth. It’s often used in advanced cases to slow down tumor progression.
5. Sunitinib (Sutent)
Sunitinib cuts off blood supply to tumors, starving them of nutrients. It’s a targeted therapy aiming to shrink the cancer.
6. Bevacizumab (Avastin)
Bevacizumab restricts blood vessel growth around tumors, effectively slowing their growth. It’s often used with chemotherapy.
7. Pancreatic Enzyme Replacement Therapy (PERT)
PERT helps manage digestive problems caused by pancreatic cancer. It aids in proper food digestion and nutrient absorption.
8. Veliparib
Veliparib is a targeted therapy that enhances the effects of chemotherapy. It prevents cancer cells from repairing themselves after chemotherapy.
9. ABRAXANE (Nab-paclitaxel)
Similar to paclitaxel, ABRAXANE blocks cell division and can increase survival rates when combined with other treatments.
10. 5-fluorouracil (5-FU)
5-FU disrupts cancer cell growth and division. It’s often used in combination with other drugs or radiation therapy.
11. Irinotecan (Camptosar)
Irinotecan interferes with DNA replication in cancer cells, preventing them from multiplying. It’s sometimes used when other treatments fail.
12. Oxaliplatin
Oxaliplatin damages cancer cell DNA, preventing them from dividing. It’s commonly used in combination with other drugs.
13. Liposomal Irinotecan (Onivyde)
This is a specialized form of irinotecan that specifically targets cancer cells in the pancreas, increasing the treatment’s effectiveness.
14. Pembrolizumab (Keytruda)
Pembrolizumab boosts the body’s immune system to fight cancer cells. It’s used in cases where the cancer has a specific genetic marker.
15. NAPOLI-1 Regimen
A combination of nanoliposomal irinotecan, 5-FU, and leucovorin, the NAPOLI-1 regimen is often used when standard treatments have failed.
16. MM-398 (Onivyde)
MM-398, in combination with 5-FU and leucovorin, targets cancer cells and enhances the effects of chemotherapy.
17. Eryaspase
Eryaspase depletes an amino acid necessary for cancer cell growth. It’s used in combination with other treatments.
18. Rucaparib (Rubraca)
Rucaparib targets inherited gene mutations in pancreatic cancer, inhibiting cancer cell growth.
19. Veliparib (PARP inhibitor)
Veliparib works against cancer with specific genetic mutations, preventing the cancer cells from repairing themselves after damage.
20. AM0010
AM0010 stimulates the immune system to attack cancer cells. It’s often used alongside other treatments.
Conclusion:
Pancreatic cancer treatment can be complex, but understanding these options can help patients and their families make informed decisions. Remember, each case is unique, and doctors will recommend the best treatment plan based on individual circumstances. By simplifying these treatments, we hope to empower you with the knowledge needed to navigate the journey of pancreatic cancer. Always consult with medical professionals for personalized guidance.