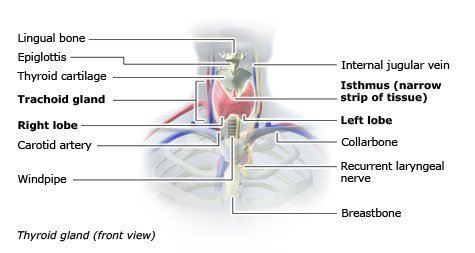
The thyroid, or thyroid gland, is an endocrine gland in vertebrates. In humans, it is in the neck and consists of two connected lobes. The lower two-thirds of the lobes are connected by a thin band of tissue called the thyroid isthmus. The thyroid is located at the front of the neck, below Adam’s apple. Microscopically, the functional unit of the thyroid gland is the spherical thyroid follicle, lined with follicular cells (thyrocytes), and occasional parafollicular cells that surround a lumen containing colloid. The thyroid gland secretes three hormones: the two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – and a peptide hormone, calcitonin. The thyroid hormones influence the metabolic rate and protein synthesis, and in children, growth and development. Calcitonin plays a role in calcium homeostasis.[1] Secretion of the two thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is secreted from the anterior pituitary gland. TSH is regulated by the thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus.[rx]
The thyroid gland is a midline structure located in the anterior neck. The thyroid functions as an endocrine gland and is responsible for producing thyroid hormone and calcitonin, thus contributing to the regulation of metabolism, growth, and serum concentrations of electrolytes such as calcium.[rx][rx]
Many disease processes can involve the thyroid gland, and alterations in the production of hormones can result in hypothyroidism or hyperthyroidism. The thyroid gland is involved in inflammatory processes (e.g., thyroiditis), autoimmune processes (e.g., Graves disease), and cancers (e.g., papillary thyroid carcinoma, medullary thyroid carcinoma, and follicular carcinoma).
In addition to considering its role in metabolism, growth, regulation of certain electrolytes, and its involvement in many disease processes, the thyroid gland deserves consideration for its anatomical location and its close relationship to important structures including the parathyroid glands, recurrent laryngeal nerves, and certain vasculature.
Anatomy of Thyroid
The thyroid gland is divided into two lobes that are connected by the isthmus, which crosses the midline of the upper trachea at the second and third tracheal rings. In its anatomic position, the thyroid gland lies posterior to the sternothyroid and sternohyoid muscles, wrapping around the cricoid cartilage and tracheal rings. It is located inferior to the laryngeal thyroid cartilage, typically corresponding to the vertebral levels C5-T1. The thyroid attaches to the trachea via consolidation of connective tissue, referred to as the lateral suspensory ligament or Berry’s ligament. This ligament connects each of the thyroid lobes to the trachea. The thyroid gland, along with the esophagus, pharynx, and trachea, is found within the visceral compartment of the neck which is bound by pretracheal fascia.
The “normal” thyroid gland has lateral lobes that are symmetrical with a well-marked centrally located isthmus. The thyroid gland typically contains a pyramidal extension on the posterior-most aspect of each lobe, referred to as the tubercle of Zuckerkandl. Despite these general characteristics, the thyroid gland is known to have many morphologic variations. The position of the thyroid gland and its close relationship with various structures brings about several surgical considerations with clinical relevance.
Blood Supply and Lymphatics of Thyroid
The thyroid gland has an extremely rich blood supply and is estimated to be six times as vascular as the kidney and relatively three to four times more vascular than the brain. It receives blood from the superior and inferior thyroid arteries. These paired vessels supply the superior and inferior aspects of the gland. The superior thyroid artery is the first branch of the external carotid artery as it arises near the level of the superior horn of the thyroid cartilage. The superior thyroid artery then moves anterior, inferior, and towards the midline behind the sternothyroid muscle to the superior pole of the lobe of the thyroid gland. From this point, the superior thyroid artery branches off. One branching point runs down the dorsal aspect of the thyroid gland. The other superficial branch runs along with the sternothyroid muscle and thyrohyoid muscles, supplying branches to these muscles as well as the sternohyoid. The superficial branch continues downward to further give off the cricothyroid branch and to supply the isthmus, inner sides of the lateral lobes, and when present, the pyramidal lobe.[rx]
The thyrocervical trunk arises from the anterosuperior surface of the subclavian artery and gives rise to three branches, one being the inferior thyroid artery. The inferior thyroid artery branches from the thyrocervical trunk at the inner border of the anterior scalene muscle and advances medially to the thyroid gland. The artery reaches the posterior surface of the lateral lobe of the thyroid gland at the level of the junction of the upper two thirds and lower third of the outer border. The largest branch of the inferior thyroid artery is the ascending cervical branch, and it is important not to mistake this branch for the inferior thyroid artery itself. [4]
In 10% of the population, there is an additional artery known as the thyroid ima artery. This artery has a variable origin including the brachiocephalic trunk, aortic arch, the right common carotid, the subclavian, the pericardiacophrenic artery, the thyrocervical trunk, transverse scapular, or internal thoracic artery. The thyroid ima most commonly originates from the brachiocephalic trunk and supplies the isthmus and anterior thyroid gland.
The thyroid gland is drained via the superior, middle, and inferior thyroid veins. The middle and superior thyroid veins follow a tortuous route and eventually drain into the internal jugular vein on either side of the neck. The drainage of the inferior thyroid vein may enter either the subclavian or brachiocephalic veins, located just posterior to the manubrium.
Lymphatic drainage of the thyroid gland involves the lower deep cervical, laryngeal, pretracheal, and paratracheal nodes. The paratracheal and lower deep cervical nodes, specifically, receive lymphatic drainage from the isthmus and the inferior lateral lobes. The superior portions of the thyroid gland drain into the superior paratracheal and cervical nodes.
Nerves Supply of Thyroid
The autonomic nervous system primarily innervates the thyroid gland. The vagus nerve provides the main parasympathetic fibers, while sympathetic fibers originate from the inferior, middle, and superior ganglia of the sympathetic trunk. These nerves do not play a role in the control of hormonal production or secretion but mostly influence vasculature. [rx]
Muscles attachment of Thyroid
Several muscles should be considered when discussing neck and thyroid surgical anatomy.
-
Platysma: The first muscle encountered during neck dissection, it is enveloped by the superficial cervical fascia. It sits in the anterior neck and extends from the superficial fascia of the deltoid, over the clavicle, reaching the mandible and superficial fascia of the face superiorly.
-
Sternocleidomastoid: This muscle forms the anterior portion of the posterior triangle of the neck. The muscle runs obliquely from the mastoid to the clavicle and sternum. The sternocleidomastoid is found anterolaterally relative to the thyroid gland.
-
Digastric muscle: This muscle extends from the mandibular tubercle, passes deep and inferior to the hyoid, and loops back up to attach to the mastoid tip.
-
Infrahyoid muscles: These are also referred to as “strap muscles.” They include four paired muscles found on the anterolateral surface of the thyroid gland. The strap muscles result in gross movement of the larynx during swallowing and also adjust the positioning of the larynx during vocalization.
-
Omohyoid muscle: The omohyoid muscle is found deep in the sternocleidomastoid. It extends from the hyoid bone to the lateral aspect of the clavicle.
-
Sternohyoid muscle: This muscle sits anterior the remaining strap muscles and the thyroid gland. The sternohyoid muscle extends from its superior attachment at the hyoid bone inferiorly to the sternum.
-
Sternothyroid muscle: This muscle extends from the oblique line of the thyroid cartilage to the sternum. This muscle contacts the anterior surface of the thyroid gland.
-
Thyrohyoid muscle: The thyrohyoid muscle extends from the oblique line of the thyroid cartilage to the hyoid bone superiorly.
-
Inferior pharyngeal constrictor: This muscle extends from its anterior attachment at the oblique line of the thyroid cartilage and lateral aspect of the cricoid cartilage to the pharyngeal raphe. This muscle contacts the superior pole of the lateral lobe of the thyroid gland medially.
Surgical Considerations
Due to its close relationship with several structures, the following must be considered during total thyroidectomy, thyroid lobectomy, or procedures involving the excision of a thyroglossal duct cyst.[rx][rx][rx]
-
A chest radiography or mediastinal computed tomography [CT] is performed preoperatively if anatomic abnormalities or substernal extension of the thyroid are suspected.
-
Due to the location of the thyroid gland, a slight neck extension of the patient on the operating table facilitates access to the neck.
-
The typical skin incision allowing proper access to the gland ranges from one to one and a half to two fingerbreadths above the clavicle. This incision is curvilinear and parallel or within a skin line.
More about Structure
- Larynx – In re-operative cases, it is recommended to perform laryngoscopy regardless of voice symptomology asymptomatic vocal cord paralysis can occur in up to 30% of patients after anterior neck surgery.
- Recurrent Laryngeal Nerve – The two nerves of importance that pass through the thyroid are the left and right recurrent laryngeal nerves [RLN]. They are often located on the lateral aspect of the thyroid gland near the vicinity of the inferior thyroid artery. When operating on the thyroid gland, it is vital to visualize these nerves and avoid trauma. The nerve can be exposed caudal to the inferior thyroid artery or following mobilization of the superior and inferior poles. The nerve is most likely to be injured in its distal portion [2-3cm]. This distal portion of the RLN is covered by either or both the tubercle of Zuckerkandl [a pyramidal extension on the most posterior aspect of each lobe] and the ligament of Berry. Most often, it is not until the tubercle of Zuckerkandl is medially retracted that the RLN is seen. The RLN most often traverses just medial to the tubercle and is hidden from view. The distal course of the RLN is more easily identified in total lobectomies as opposed to subtotal lobectomies, in which the distal course of the RLN may not always be visualized.
- Superior laryngeal nerve – When the superior pole of the thyroid gland is dissected, one may visualize the superior laryngeal nerve [SLN] which often runs next to the superior thyroid artery. High ligation of the superior thyroid artery should be avoided as one can easily injure the superior laryngeal nerve. Approximately 20% of patients are at risk of injury to the external branch of the SLN when using a technique in which the superior thyroid vessels are clamped, divided, and ligated en masse. Dividing the superior thyroid vessels as they enter the capsule prevents injury to those nerves in close proximity to the artery. In practice, most surgeons do not insist on direct visualization of the superior laryngeal nerve.
- Cervical sympathetic trunk – Rarely, the cervical sympathetic trunk may be injured. This is a consideration when the carotid sheath is mobilized in order to treat retro esophageal extension of a goiter or malignancy.
- Esophagus – Altered anatomy and displacement of the trachea can result in the exposure of the anterior esophageal surface, creating the risk of potential injury.
- Carotid artery – The carotid arteries, which course posterolateral to the thyroid gland, are rarely an issue during thyroidectomy. Excessive lateral traction in an individual with an enlarged thyroid gland may result in ocular or central nervous system damage from reduced blood flow. This is preventable with proper retraction and tissue handling.
- Parathyroid glands – The parathyroid glands are in a close anatomic relationship to the thyroid gland, sitting on the posterior aspect of the thyroid gland. The parathyroid glands also share arterial supply with the thyroid gland, being supplied by an end-artery, typically the inferior thyroid artery. Due to its anatomic relationship and vascular supply, there a few considerations with regards to the parathyroid glands in thyroid surgeries. By dividing the branches of the inferior thyroid artery beyond the parathyroid gland on the thyroid gland capsule, disruption of the end-artery can best be avoided. However, transplantation to a “dry” pocket in the sternocleidomastoid muscle, a subcutaneous area or forearm can be performed if end-artery damage does occur.
- Thyroglossal duct cyst procedure – Approximately 50% of thyroglossal duct cysts are close to or just inferior to the hyoid bone. Due to its relation to the hyoid bone and the rates of recurrence, surgical removal includes the cyst, the middle segment of the hyoid bone, and the track that leads to the base of the tongue. This procedure is referred to as the Sistrunk Procedure.
- Post Operative Bleeding – Due to the location, hematomas may lead to acute respiratory problems. Insidious hemorrhage may also result in laryngeal edema and infrequently can lead to the need for tracheostomy.
- Muscle Closure Following Thyroid Procedures – Surgical considerations for wound closure are under consideration of transversely divided muscles. One must consider a closure that would create space for blood to disperse if bleeding were to occur. When the strap muscles are separated from the midline and retracted laterally, reapproximation in the midline is performed, once again with consideration of space for possible bleeding. Additionally, some reapproximate the platysma muscle and its fascia.
Clinical Significance
- Goiter – It is a condition where the thyroid gland shows an abnormal enlargement. Goiters broadly classify into uni-nodular, multinodular, and diffuse types. Each further includes many different types of goiters. Some of the commonest with some of their important features are described below.[rx][rx]
- Colloid nodular goiter – This is the commonest of the non-neoplastic lesions of the thyroid.[rx] In these types of goiter, the thyroid follicles are filled with an abundant amount of colloid in their lumens and lined by squamous follicular cells.
- Hyperthyroidism (Thyrotoxicosis) – It is a condition of hypermetabolic state and hyperfunctioning of the thyroid gland resulting in increased T3 and T4 levels. Some symptoms included palpitations, tachycardia, nervousness, etc.
- Graves disease – This disease is a combination of thyrotoxicosis, exophthalmos, and dermopathy (myxedema). It is especially seen in women in the age group of 20 to 40 years, manifesting in the form of prolonged and violent palpitations.
- Thyroid cancer – Thyroid carcinomas arise either from the follicular epithelium or parafollicular C-cells. They are painless nodules and compression, displaces the adjacent structures. The carcinomas of the thyroid can manifest in the form of papillary carcinoma, follicular carcinoma, anaplastic carcinoma, and medullary carcinoma.
- Thyroiditis – Inflammation of the thyroid, usually from a viral infection or autoimmune condition. Thyroiditis can be painful or have no symptoms at all.
- Thyroid cancer – An uncommon form of cancer, thyroid cancer is usually curable. Surgery, radiation, and hormone treatments may be used to treat thyroid cancer.
- Thyroid nodule – A small abnormal mass or lump in the thyroid gland. Thyroid nodules are extremely common. Few are cancerous. They may secrete excess hormones, causing hyperthyroidism, or cause no problems.
- Thyroid storm – A rare form of hyperthyroidism in which extremely high thyroid hormone levels cause severe illness.
Symptoms of Hypothyroidism
Generalized decreased basal metabolic rate can present as apathy, slowed cognition, skin dryness, alopecia, increased low-density lipoproteins, and increased triglycerides. Hypothyroidism must be ruled out in psychiatry patients presenting with apathy and slowed cognition. Hypothyroidism can decrease sympathetic activity leading to decreased sweating, bradycardia, and constipation. Patients can present with myopathy and decreased cardiac output because of decreased transcription of sarcolemmal genes.
Hyperprolactinemia can be caused by hypothyroidism. Thyrotropin-releasing hormone (TRH) from the hypothalamus stimulates prolactin and TSH release. Prolactin release can suppress testosterone, LH, FSH, and GnRH release. Prolactin can also cause breast tissue growth.
Patients with hypothyroidism may present with myxedema caused by decreased clearance of complex glycosaminoglycans and hyaluronic acids from the reticular layer of the dermis. Initially, the nonpitting edema is pretibial. As the state of hypothyroidism continues, patients can develop generalized edema.
Symptoms related to decreased metabolic rate
-
Bradycardia
-
Fatigue
-
Cold intolerance
-
Weight gain
-
Poor appetite
-
Hair loss
-
Cold and dry skin
-
Constipation
-
Myopathy, stiffness, cramps, entrapment syndromes
-
Delayed deep tendon reflex relaxation
Symptoms from generalized myxedema
-
Myxedematous heart disease
-
Puffy appearance with doughy skin texture
-
Hoarse voice with difficulty articulate words
-
Pretibial and periorbital edema
Symptoms of hyperprolactinemia
-
Amenorrhea or menorrhagia
-
Galactorrhea
-
Erectile dysfunction, infertility in men
-
Decreased libido
Other symptoms
-
Depression
-
Impaired concentration and memory
-
Goiter
-
Hypertension
Congenital hypothyroidism
-
Umbilical hernia
-
Hypotonia
-
Prolonged neonatal jaundice
-
Poor feeding, absence of thirst (adipsia)
-
Decreased activity
-
Pot-belly, puffy-face, protuberant tongue
-
Poor brain development
Symptoms of Hyperthyroidism
Generalized hypermetabolism from hyperthyroidism causes increased Na+/K+-ATPase to promote thermogenesis. There is increased catecholamine secretion and, beta-adrenergic receptors are also upregulated in various tissues. As a result of the hyperadrenergic state, peripheral vascular resistance is decreased. In the heart, hyperthyroidism causes a decreased amount of phospholamban, a protein that normally decreases the affinity of calcium-ATPase for calcium in the sarcoplasmic reticulum. As a result of decreased phospholamban, there is increased Ca+ movement between the sarcoplasmic reticulum and cytosol, leading to increased contractility. Increased beta-receptors on the heart also lead to increased cardiac output.
General
-
Heat intolerance
-
Weight loss
-
Increased appetite
-
Increased sweating from cutaneous blood flow increase
-
Weakness
-
Fatigue
-
Onycholysis (separation of nails from nail beds)
-
Pretibial myxedema
Eyes
-
Lid lag (when looking down, sclera visible above cornea)
-
Lid retraction (when looking straight, sclera visible above the cornea)
-
Graves ophthalmopathy
Goiter
-
Diffuse, smooth, non-tender goiter
-
The audible bruit can be heard at the superior poles
Cardiovascular
-
Tachycardia (can be masked by patients taking beta-blockers)
-
Palpitations
-
An irregular pulse from atrial fibrillation
-
Hypertension
-
Widened pulse pressure because systolic pressure increases and diastolic pressure decreases
-
Heart failure (elderly patients)
-
Chest pain
-
Abnormal heart rhythms
Musculoskeletal
-
Fine tremors of the outstretched fingers. Face, tongue, and head can also be involved. Tremors respond well to treatment with beta-blockers.
-
Myopathy affecting proximal muscles. Serum creatine kinase levels can be normal.
-
Osteoporosis, caused by the direct effects of T3. Elderly patients can present with fractures.
Neuropsychiatric system
-
Restlessness
-
Anxiety
-
Depression
-
Emotional instability
-
Insomnia
-
Tremoulousness
-
Hyperreflexia
Conditions associated with hypothyroidism
-
Iodine deficiency [rx]
-
Cretinism [rx]
-
Wolff-Chaikoff effect
-
Subacute thyroiditis [rx]
-
Postpartum thyroiditis [rx]
-
Riedel thyroiditis [rx]
-
Hashimoto thyroiditis [rx]
-
Drug-induced [rx]
Conditions associated with hyperthyroidism
-
Graves disease [rx]
-
Iodine excess [rx]
-
Struma ovarii [rx]
-
Thyrotropic pituitary adenoma [rx]
-
Jod-Basedow phenomenon [rx]
-
Drug-induced: amiodarone, lithium [rx]
-
Thyrotoxicosis and thyroid storm [rx]
-
Toxic multinodular goiter [rx]
-
Thyroid adenoma [rx]
Diagnosis
History and Physical
Subclinical hypothyroidism is asymptomatic most of the time. However, it can present with symptoms of hypothyroidism.[rx] It is essential to assess hypothyroid symptoms as it influences whether thyroid replacement therapy requires initiation. The clinical features of hypothyroidism are as follows:
-
Integumentary: Dry skin, hair loss, loss of outer 1/3rd of eyebrows, facial puffiness.
-
Gastrointestinal: Constipation, dysphagia, loss of appetite, weight gain, cholelithiasis
-
Cardiovascular: Diastolic hypertension, bradycardia, pericardial effusions.
-
Neurological: Decreased attention span, pseudodementia, mononeuropathies (most commonly carpal tunnel syndrome)
-
Musculoskeletal: Muscular weakness, cramps, stiffness, fatigue.
-
Reproductive: Irregular periods, decreased libido.[rx]
Hypothalamus releases thyrotropin-releasing hormone (TRH) that stimulates the secretion of TSH in the pituitary gland. Increased free T4 and T3 inhibit the release of TRH and TSH through a negative feedback loop. As a result, T3 and T4 secretion and iodine uptake are reduced. Other hormones, such as somatostatin, glucocorticoids, and dopamine, also inhibit TSH production. Cold, stress, and exercise increase TRH release.
The initial tests of choice to screen for any thyroid abnormality are a TSH and free thyroxine (free T4) test. These determine whether the abnormality arises centrally from the thyroid gland (primary), peripherally from the pituitary (secondary), or hypothalamus (tertiary). In primary hypothyroidism is suspected, the thyroid gland is not releasing enough thyroid hormones. Therefore, TSH levels will be appropriately elevated, while free T4 levels will be lower. In primary hyperthyroidism, free T4 levels abnormally increased, and TSH levels will be appropriately decreased. Other lab tests such as TSH receptor antibodies or antibodies to thyroid peroxidase can help aid in diagnosing Graves disease or Hashimoto thyroiditis, respectively.[rx]
In pregnant women, thyroid-binding globulin production is increased because of estrogen and beta-human chorionic gonadotropin (beta-HCG). More free T4 will be bound to TGB, leading to increased production of T4. TSH levels and free T4 levels will normalize, and total T4 will increase. Therefore, laboratory values will show normal TSH, normal free T4, and elevated total T4.[rx]
Thyroid Tests
- Anti-TPO antibodies – In autoimmune thyroid disease, proteins mistakenly attack the thyroid peroxidase enzyme, which is used by the thyroid to make thyroid hormones.
- Thyroid ultrasound – A probe is placed on the skin of the neck, and reflected sound waves can detect abnormal areas of thyroid tissue.
- Thyroid scan – A small amount of radioactive iodine is given by mouth to get images of the thyroid gland. Radioactive iodine is concentrated within the thyroid gland.
- Thyroid biopsy – A small amount of thyroid tissue is removed, usually to look for thyroid cancer. A thyroid biopsy is typically done with a needle.
- Thyroid-stimulating hormone (TSH) – Secreted by the brain, TSH regulates thyroid hormone release. A blood test with high TSH indicates low levels of thyroid hormone (hypothyroidism), and low TSH suggests hyperthyroidism.
- T3 and T4 (thyroxine) – The primary forms of thyroid hormone, checked with a blood test.
- Thyroglobulins – A substance secreted by the thyroid that can be used as a marker of thyroid cancer. It is often measured during follow-up in patients with thyroid cancer. High levels indicate recurrence of cancer.
- Other imaging tests – If thyroid cancer has spread (metastasized), tests such as CT scans, MRI scans, or PET scans can help identify the extent of spread.
Thyroid Treatments
Antithyroid drugs that work in the thyroid gland [rx]
-
Perchlorate – inhibits Na+/I- symporter – blocks iodide uptake
-
Thionamides – inhibits TPO – block thyroid hormone synthesis
-
Iodide > 5mg – inhibits Na+/I- symporter and TPO – blocks iodide uptake and thyroid hormone synthesis
-
Lithium – inhibits thyroid hormone release (off-label use for thyroid storm)
- Thyroid surgery (thyroidectomy) – A surgeon removes all or part of the thyroid in an operation. Thyroidectomy is performed for thyroid cancer, goiter, or hyperthyroidism.
- Antithyroid medications – Drugs can slow down the overproduction of thyroid hormone in hyperthyroidism. Two common antithyroid medicines are methimazole and propylthiouracil.
- Radioactive iodine – Iodine with radioactivity that can be used in low doses to test the thyroid gland or destroy an overactive gland. Large doses can be used to destroy cancerous tissue.
- External radiation – A beam of radiation is directed at the thyroid, on multiple appointments. The high-energy rays help kill thyroid cancer cells.
- Thyroid hormone pills – Daily treatment that replaces the amount of thyroid hormone you can no longer make. Thyroid hormone pills treat hypothyroidism and are also used to help prevent thyroid cancer from coming back after treatment.
- Recombinant human TSH – Injecting this thyroid-stimulating agent can make thyroid cancer show up more clearly on imaging tests.
Antithyroid drugs that work in peripheral tissue – all these drugs inhibit the deiodinase enzymes. Deiodinase enzymes normally convert T4 into the active form T3. These drugs inhibit the conversion of T4 to T3 and reduce its activity.
-
Propylthiouracil (thionamide)
-
Dexamethasone
-
Amiodarone
-
Propranolol
References






