The scrotum is a male reproductive structure located under the penis. It has the shape of a sac and divides into two compartments. The structures contained in this sac include external spermatic fascia, testes, epididymis, and spermatic cord. The scrotum derives from the labioscrotal swelling, which is an embryonic structure that appears in the fourth week of embryonic development. Congenital malformations may occur during the development of the scrotum. These malformations can present in conjunction with other defects due to a common embryologic origin.
Structure and Function
Structure:
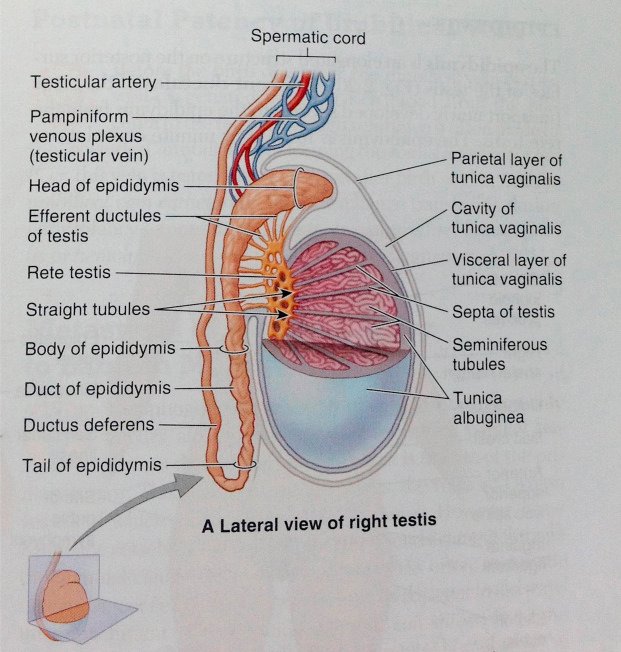
The scrotum is a thin external sac that is located under the penis and is composed of skin and smooth muscle. This sac is divided into two compartments by the scrotal septum. The average wall thickness of the scrotum is about 8 mm. It has a parietal and a visceral layer. The parietal layer has the function of covering the inner aspect of the scrotal wall and the visceral layer coats the testis and epididymis. The structures contained in the scrotal sac are the external spermatic fascia, testes, epididymis, and spermatic cord.
Function:
The scrotum is responsible for protecting the testes. It helps with the thermoregulation of the testicles. It keeps the temperature of the testis several degrees below the average body temperature, which is an essential factor for sperm production.
It is sperm production, or spermatogenesis, in the testes that highlights the essential function of the scrotum. The production of sperm is most efficient within a small range of temperature. The presence of the testes in the scrotum means they are located just outside of the body, allowing them to be slightly cooler than the internal body temperature.
However, if the temperature of the testes drops, the dartos muscle of the scrotum, and the cremaster muscle (one of the layers covering the testes), will contract, pulling the scrotum and the testes closer to the body. This will raise the temperature in the testes. On the other hand, if the temperature in the testes is too high, the dartos and cremaster muscles can relax, lowering the scrotum and testes away from the body, and consequently lowering the temperature of the testes.

Blood Supply and Lymphatics
Blood Supply:
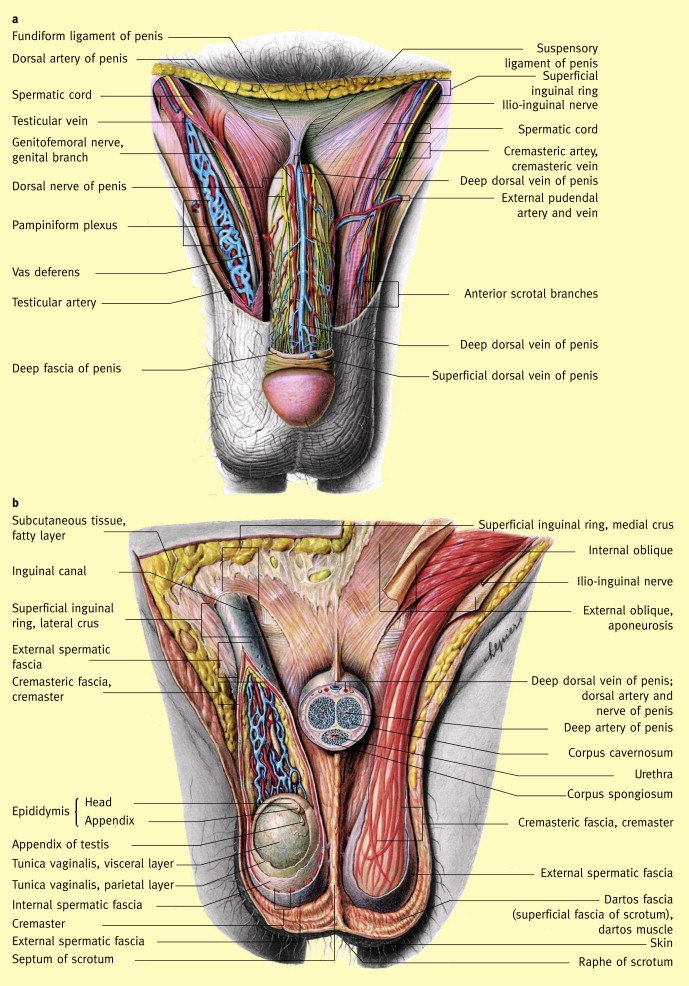
Arteriovenous anastomoses and subcutaneous plexuses are responsible for providing blood supply to the scrotum. The external pudendal branches arising from the femoral arteries and the scrotal branches of the in the internal pudendal arteries play a significant role in supplying blood to the scrotum. The nomenclature of the venous drainage of the scrotum mirrors the previously mentioned corresponding arteries.
Lymphatic drainage:
The arrangement of the lymphatic drainage of the scrotum is related to the development of this sac. The wall of the scrotum drains into the superficial inguinal lymph nodes. On the other hand, the contents of the scrotum drain to the lumbar lymph nodes. It is important to recall that the testes migrate from the abdominal wall through the inguinal canal and into the scrotum. During this path, the testis will drag its blood supply and lymph vessels into the scrotal sac.[rx]

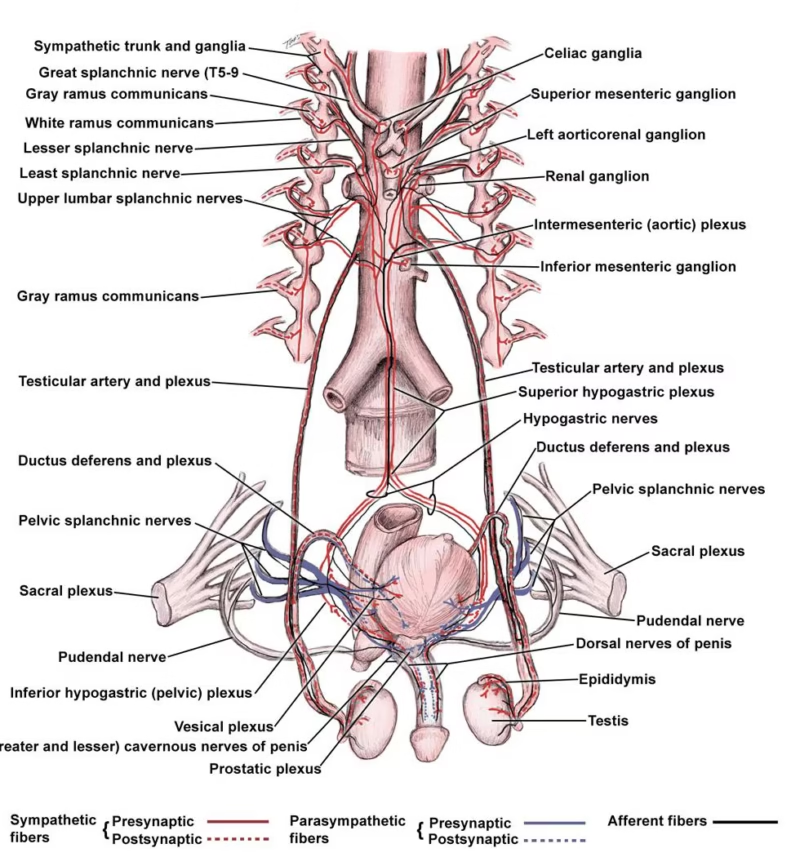
Nerves
The innervation of the scrotum derives from the branches of the following four nerves: genitofemoral, pudendal, posterior femoral cutaneous, and ilioinguinal nerves.
Anterior Innervation:
The cremaster muscle and anterior scrotum receive their innervation by the genital branch of the genitofemoral nerve. This nerve arises from the L1-L2 segments of the lumbosacral plexus and then travels through the inguinal canal to supply the anterior skin of the scrotum.
Posterior Innervation:
The posterior scrotum is innervated by branches of the pudendal nerve and by the posterior femoral cutaneous nerve.
The ilioinguinal nerve also aids the genitofemoral nerve in the innervation of the cremasteric muscle.
Cremasteric Reflex:
Both the ilioinguinal and the genitofemoral nerves provide a sensory synapse that activates the motor neurons responsible for the cremasteric reflex.[rx] This physiologic reflex has both protective and thermoregulatory testicular functions.[rx]
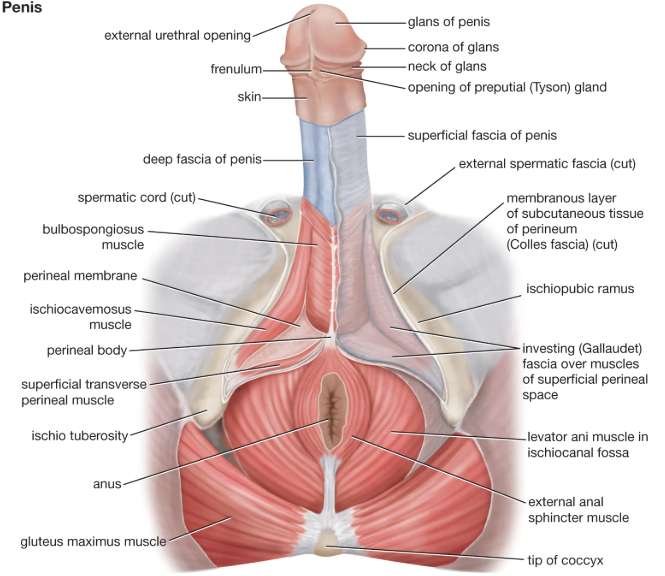
Muscles
The scrotum is a fibromuscular structure. The muscle fibers contained in the scrotum are the dartos muscle and the cremasteric muscle. The dartos muscle is a smooth muscle sheet located underneath the skin of the scrotum. The cremasteric muscle is a paired muscle that has many protective functions. This paired muscle is composed of two parts, a medial cremaster portion originating from the pubic tubercle and the lateral cremaster portion originating from the internal oblique muscle.
Development and anatomy
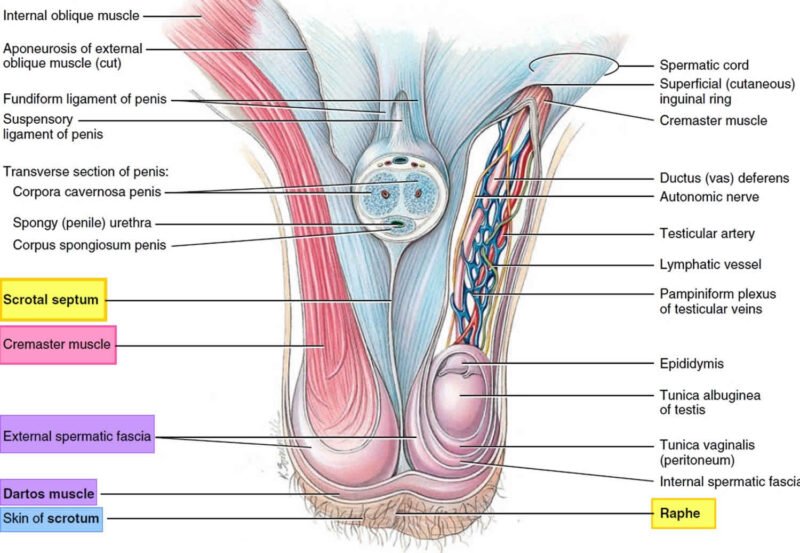
In the embryo, the scrotum develops from a pair of ridges or elevations, that form on either side of the embryonic genital tubercle. The tubercle will later develop into the penis in the male, or the clitoris in the female. The elevations on either side of the tubercle are known as labioscrotal swellings, as they will later develop into either the scrotum in males, or into the labia majora in females. As the embryo continues to develop and become a fetus, the separated pair of labioscrotal swellings will fuse at the midline, creating one continuous sac, the scrotum. Towards the end of pregnancy, approximately 32 weeks, both testes have completed their descent from the posterior abdominal wall, through the inguinal canal, to finally reach the scrotum.
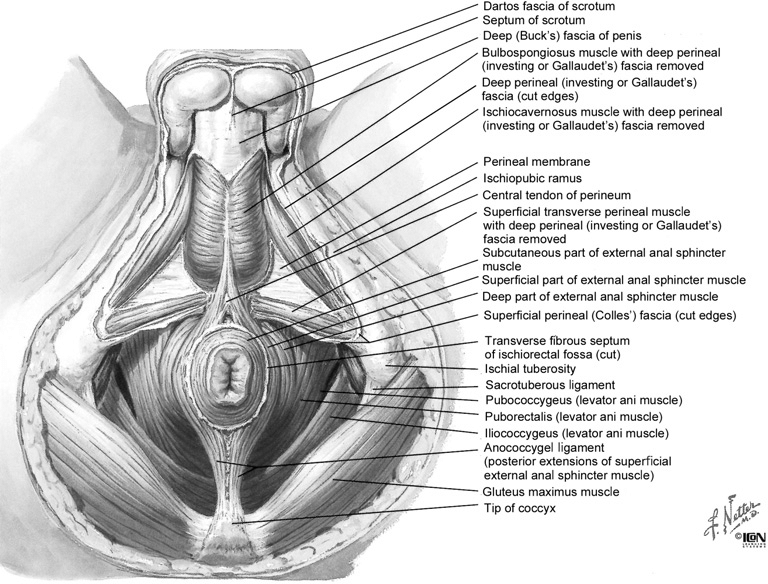
Because of the pathway of descent through the anterior abdominal wall, the testes will be covered by the layers of fascia and muscles (external and internal obliques, and transversus abdominis) associated with the abdominal region. The scrotum however, has only two layers, because it develops separately from the testes. Externally is the skin, and below the skin a layer of fascia known as dartos fascia. This fascial layer is devoid of fat but does include smooth muscle fibers collectively known as the dartos muscle. Since the fascial layer, including its muscle fibers, attaches to the overlying skin, when the dartos muscle contracts it gives the scrotum its wrinkled appearance.
Contents
As mentioned previously, the scrotum contains the testes and parts of the spermatic cord. The testes are the site of sperm production, and as such, form the essential component of the male reproductive system. Sperm leaves the testes via the epididymis, which then drains into the ductus deferens. The epididymis and lower portions of the ductus deferens are located within the scrotum. The ductus deferens is joined by blood vessels supplying the testes, creating the contents of the spermatic cord.
Layer
The layers of the scrotum are continuation of the abdominal wall layers. From superficial to deep, scrotal layers include: skin, superficial “Dartos” fascia, external spermatic fascia, cremaster muscle, internal spermatic fascia, and tunica vaginalis. Dartos fascia is contiguous with Scarpa’s fascia in the abdomen and Colles’ fascia in the perineum.
Abdominal wall and its corresponding scrotal wall layers.
| Abdominal wall | Scrotum |
|---|---|
| Skin | Skin |
| Scarpa’s fascia | Dartos & smooth muscle |
| External oblique fascia | External spermatic fascia |
| Internal oblique muscle & aponeurosis | Cremasteric fascia & muscle |
| Transversus abdominis muscle & aponeurosis | Cremasteric fascia & muscle |
| Transversalis fascia | Internal spermatic fascia |
| Peritoneum | Tunica vaginalis |
The testis, epididymis, and spermatic cord are housed within the scrotum. Other than being attached to the base of the scrotum by the gubernaculum to prevent torsion, the testes are free to move around. The right testicle in most cases rests at a higher level than the left. The epididymis has three parts—head, body and tail. Only the epididymal head is fixed to the upper part of the testis; relationship of the body and tail to the testis is often variable . Blood and nerve supply for the epididymis and testis are generally found on the posterior side (rx). The spermatic cord is a connective tissue matrix that contains the vas deferens, three arteries, three veins, lymphatics, and two nerves. A third nerve, the ilioinguinal, lies just lateral to the cord







