Cranial nerve examination frequently appears in OSCEs. You’ll be expected to assess a subset of the twelve cranial nerves and identify abnormalities using your clinical skills. This cranial nerve examination OSCE guide provides a clear step-by-step approach to examining the cranial nerves, with an included video demonstration.
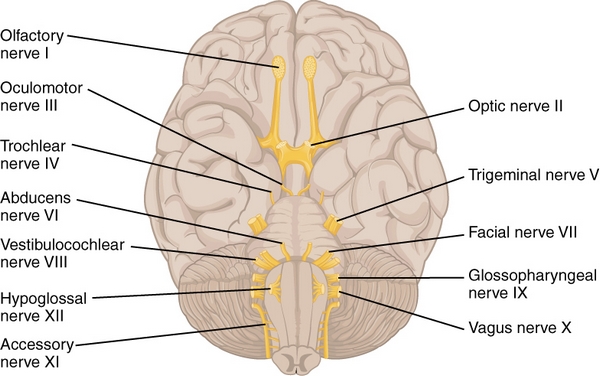
Examination of the 12 Pairs of Cranial Nerves
The diagnosis of a simple neurological disorder without EEG, CT or MRT scans is clear, manageable and cost-effective.
It consists of a light source, a neurological reflex hammer, a tuning fork and resources such as brushes, cotton swabs, and blunt pins with which a patient’s sensitivity can be examined. Test tubes filled with cold and warm water can be used to determine a patient’s sensation of cold and warm temperatures.
Anamnesis is an essential component of any suspected diagnosis, especially in neurology. Using specifically targeted questions, the physician establishes solid medical basis for the patient for further case history and subsequent examination.
Examination of the N. Olfactorius
The olfactory nerve (n. olfactorius) is responsible for the sense of smell and is a complete sensory nerve.
The olfactory test entails individual examination of each nostril and closure of the patient’s eyes because olfactory memory leads to odor recognition. Using scented sticks with characteristic odors such as coffee, cinnamon, or aniseed, the patient is asked to smell and identify them individually, using each nostril.
According to the patient’s age and the number of odors detected, a distinction is drawn between anosmia, hyposmia and normosmia. Loss of smell (anosmia) may be attributed to:
- Severe cranial cerebral trauma caused by an accident
- Altered and abnormal sensory perception
- Infections
- Tumors, especially olfactory meningioma
- Inflammation of the nasopharyngeal space, with infection of olfactory mucosa
In case of gustatory sensation (lat. gustare = taste), especially due to suspected simulation, the patient is explicitly requested to taste pure olfactory irritants (e.g., cinnamon) or mixed irritants comprising smell and taste components (e.g., cocoa with nuts). Upon taste recognition, the patient identifies the odor component, suggesting simulation.
Examination of the N. Opticus
The optic nerve (n.opticus) is the second cranial nerve, which transmits visual information to the occipital visual cortex. It is a complete sensory nerve. Visual acuity and visual fields are important aspects of the optic nerve.
Neurological examination of the optic nerve entails:
- Indicative examination of visual acuity
- Indicative examination of visual fields by confrontation (perimetry)
- Simultaneous examination of the visual fields
- Inspection of the pupils and examination of the pupil size
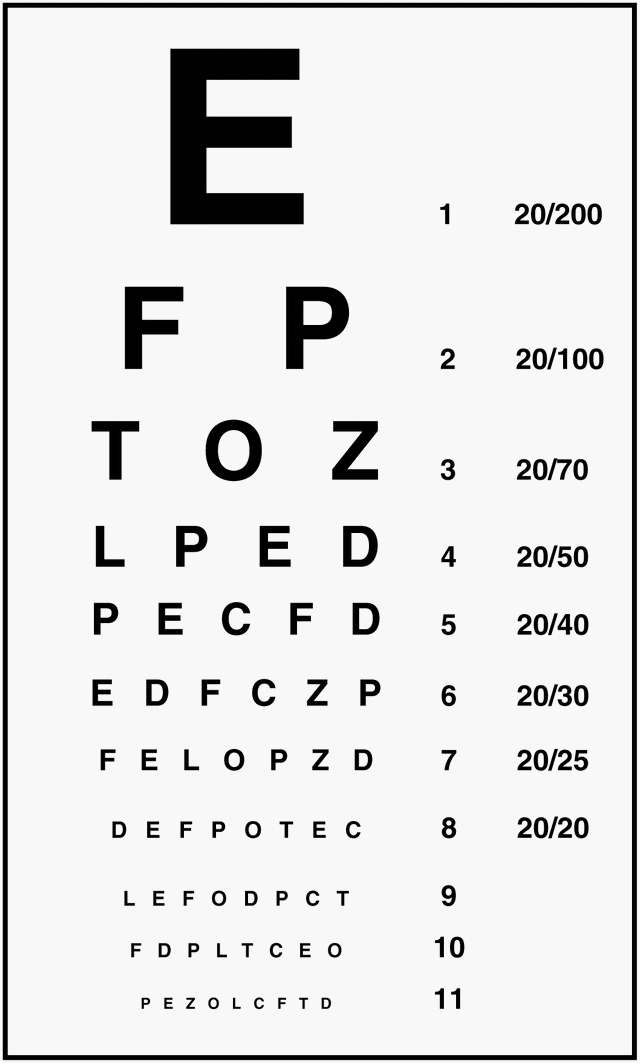
Indicative examination of visual acuity
Visual acuity testing is an integral component of any ophthalmological examination determining the best possible visual acuity.
Visual acuity test is used to evaluate the optical integrity of the eyes, retinal health, and the interpretation of retinal images by the brain.
Basically, the test is carried out monocularly at an approx. distance of 5 m, with the unexamined eye fully but loosely covered. The vision reading charts contain various eye test characters (optotypes) such as numbers, letters, children´s images, landolt rings and e-hooks (for patients where verbal communication is not possible). The process is repeated for both the eyes, with and without distance glasses. Another vision reading chart to determine visual acuity is the “Snellen Chart”:
The visual acuity for proximity is tested using reading samples at a reading distance of about 30 cm.
Indicative examination of visual fields by confrontation (perimetry)
The patient covers one eye while fixing their gaze on the opposite eye of the examiner with the other eye. The examiner moves an extended forefinger in different directions, from the periphery and into the patient’s visual field. The patient signals upon detection of the examiner’s finger.
Simultaneous examination of visual fields

The patient looks at the examiner with both eyes, without covering an eye. The examiner holds his hands peripherally in the right and left visual fields, and moves his fingers randomly on one side, or simultaneously bilaterally. The patient then indicates the side or sides, in which the fingers were moved.
Inspection of the pupils and examination of the pupil size
Before testing pupillary constriction, the examiner should inspect and evaluate the function of the musculus sphincter pupillae. The examiner also tests the sympathetic fibers, which innervate the musculus dilator pupillae, and the afferent (lat. affere = to bring, to lead) pathways related to pupillary function, the retina, the optic nerve and the optic tract (tractus opticus).
When examining pupil size, pupillary constriction is tested under direct lighting using a small light source. This test is used to determine the shape, symmetry and reactivity as well as the size of the pupils. Using a semi-darkened room, the patient looks into the distance, thereby avoiding initiation of a short-range adaptation miosis (Greek miosis = reduction).
The examiner then separates the eyes from each other by placing a flat hand on the bridge of the nose. He/she then illuminates one eye with bright light at a time from a position below the pupil. The reaction of the illuminated eye is initially observed, followed by the reaction of the non-illuminated eye.
A normal result with respect to the pupil suggests symmetrical size and shape, and prompt constriction of the pupil in response to light without any side-related difference.
Examination of the N. Oculomotorius, N. Trochlearis and N. Abducens
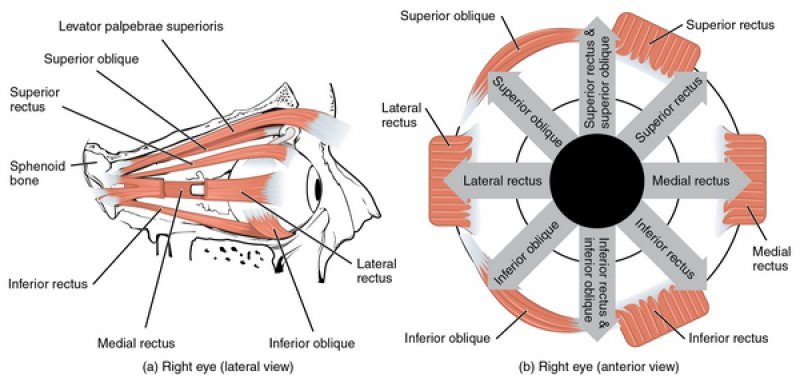
The oculomotor (n. oculomotorius), trochlear (n. trochlearis) and abducens (n. abducens) nerves are cranial nerves with predominantly motor function, which coordinate movement of the eyeball via control of external ocular muscles. The position of the eyeball allows the examiner to determine the damaged nerve.
Each eye is controlled by six external ocular muscles, which control the full range of movement of the eyeball.
The nervus oculomotorius
The oculomotor nerve is the nerve which controls the movement of the eye and innervates the musculus rectus superior (superior rectus muscle), the musculus rectus medialis (medial rectus muscle), the musculus rectus inferior (inferior rectus muscle), and the musculus obliquus inferior (inferior oblique muscle).
To test the eye movement, the patient focuses and follows the examiner’s fingers while maintaining the head stationary in a dark room, followed by bright and dim light to study sympathetic or parasympathetic tone.
Nervus trochlearis

The trochlear nerve is responsible for rotation of the eye; it innervates the superior oblique muscle and can be checked by convergence or tested using a ‘squint test’. The patient is asked to fix their gaze on the index finger of the examiner while moving the finger from a position (approx. 30–50 cm) below the patient’s face, towards the tip of the patient’s nose.
Nervus abducens
The abducens nerve (n. abducens) supplies the lateral rectus muscle. The patient is asked to follow an object or a lamp.
Examination of the N. Trigeminus
The trigeminal nerve (n. trigeminus) is the largest cranial nerve, and has both sensory and motor functions. It provides sensory innervation to the skin of the face, to the facial mucosa, including the teeth, and also to the dura mater (part of the hard cerebral membrane). It also provides motor control to the muscles of mastication (chewing).
Examination of the trigeminal nerve is based on:
- sensory function test
- examination of the nerve exit points
- the corneal reflex
- the masseter reflex
Testing sensory functions
The skin on the patient’s face is touched gently, using a wisp of cotton wool, to test the sense of touch. The pain is evaluated with a blunt object (e.g. a wooden stick). Normal findings are symmetrical touch, and sensation of pain.
Examination of the nerve exit points
The rough tenderness of the three peripheral branches of the nerves can be assessed at their exit points: the supraorbital foramen, the infraorbital foramen and the mental foramen. The examiner presses the foramen using the thumb or middle finger. Slight tenderness is a normal finding.
The corneal reflex
The cornea is touched on one side, using a cotton swab. A normal finding is represented by normal closing of the eyelid (the blink reflex), with respect to each eye. It determines the sensation nerve V and VII.
The masseter reflex
The examiner places the index finger across a slightly open lower jaw, and taps it with a tendon hammer, which should elicit bilateral contraction of the jaw by contracting temporalis. It can be felt as an upward phasic movement of the lower jaw by pterygoids.
Examination of the N. Facialis
The facial nerve (n. facialis) is a mixed cranial nerve. It is responsible for the movement of most of the facial muscles, except the masticatory muscles, and also for the movement of platysma and the stapedius muscle in the middle ear.
Examination of the seventh cranial nerve is based on the patient’s facial expression, whether or not the nasolabial grooves carry equal depth bilaterally, depending on the symmetry of the eyelids in terms of width, and pronounced furrows of the forehead. In addition, the patient is asked to activate the facial muscles innervated by the facial nerve, for example by means of:
-
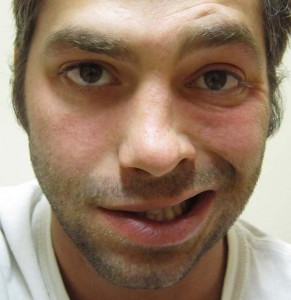
a frown,
- puffing out the cheeks,
- closing the eyes, against resistance,
- firmly shutting of the eyes,
- revealing the teeth or
- whistling
Examination of the N. Vestibulocochlearis
The vestibulocochlear nerve (n. vestibulocochlear) is a cranial nerve with a mainly sensory function, and comprises the vestibular and the cochlear nerves. The vestibular nerve is responsible for innervation of the organ of equilibrium (balance) and the cochlear nerve is responsible for hearing (audition).
Indicative hearing examination
With decreasing distance, and starting at 6 m, words or numbers of four syllables are directed at the patient alternating with natural and whispered speech. The test ear is inclined towards the examiner during the examination.
Note: Whispering or high-frequency tuning fork can be used in this test. The properties of tuning fork can be used to determine nerve deafness or conductive deafness.
Examination of balance
When examining the vestibular nerve, Romberg’s Test and Unterberger’s Stepping Test are two important options available. However, when it comes to testing the auditory nerve, a variety tuning fork tests are used.
With Romberg’s test, the patient stands with feet together, arms stretched forwards and eyes closed. Vestibular disease is indicated by the reproducible tendency to fall towards one side. However, a tendency for the patient to fall towards the front, towards the back or to both sides excludes neurological factors underlying the loss of motor coordination.
Unterberger’s stepping test is similar to Romberg’s test, except that the patient is additionally asked to walk on the spot with eyes closed. A vestibular disorder is present if the patient reproducibly turns more than 60º to one side. This test is used to determine peripheral labyrinthine dysfunction.
In addition to coordination of movement, the examiner evaluates nystagmus (eye movement).
Examination of the N. Glossopharyngeus and the N. Vagus
The glossopharyngeal nerve (n. glossopharyngeus) is a mixed cranial nerve containing both sensory and motor components. It provides sensitivity-related and sensory innervation to the palate and the throat, and also to the back of the tongue, especially with respect to the sensation of bitter tastes.
Examination
When examining the ninth cranial nerve, any hoarseness in the patient is evaluated. The soft palate and the uvula are also inspected. The examiner determines whether or not the soft palate is uniform in height and the uvula appears in the midline.
When clear phonation is used – ask the patient to say “Aaah” – and the finding is normal if the soft palate elevates symmetrically, and the uvula remains in the midline.
The pharyngeal reflex (the gag reflex)
The swallowing reflex is initiated through the respective motor fibers. Using the tip of a cotton swab or a sharp object usually a tongue depressor, the sense of touch is examined. It triggers reflexive elevation of the soft palate or the gag reflex.
The vagus nerve (n. vagus) provides autonomous parasympathetic innervation of the internal organs and innervates the muscles of the larynx and the upper digestive tract triggering the swallow or gag reflex.
If the reflex fails, then both the ninth and the tenth cranial nerves may be damaged, as both cerebral nerves are involved in the gag reflex. The examiner should look for any indications of swallowing disorders or cardiac arrhythmias during the examination of the pharyngeal reflex.
Examination of the N. Accessories
The accessory nerve (n. accessories) is a cranial nerve with predominantly motor function, and it innervates the sternocleidomastoid and the trapezius muscle.
The testing function of the two muscles
This examination tests the strength of the two muscles, on separate sides. The sternocleidomastoid muscle is evaluated by asking the patient to rotate their head to the side, against resistance, or by asking them to raise or shrug their shoulders against resistance, by pressing on the trapezius, using the hands.
Normal finding: Symmetrical, full strength in the innervated muscle. Lower motor nerves induce weakness in both the muscles and the upper motor nerve lesion triggers ipsilateral weakness in the sternomastoid and contralateral weakness in the trapezius muscle.
Examination of the N. Hypoglossus
The hypoglossal nerve (n. hypoglossus) is a cranial nerve with motor function, which innervates the tongue.
While examining the tongue, the examiner should pay attention to:
- the symmetry of the protruded tongue
- any deviation from the paralyzed side
- any atrophy

The patients are also asked to move their protruded tongue back and forth quickly and to lick their lips.
Alternatively, the examiner can ask the patients to press their tongue against the inside of their cheek with all their strength. The examiner applies counter-pressure externally to assess the degree of force on both sides.
In this test, if the protruded tongue is deviated to one side, it indicates hypoglossal lesions.
References