Spinal cord injury (SCI) is a multidimensional disorder arising from direct or indirect spinal cord damage and is a disabling condition that disrupts motor, sensory, and autonomic functions.. The most common SCI cause is acute trauma from motor vehicular crashes (MVCs), although the condition may also arise from insidious etiologies such as malignancies and chronic tuberculous infection. Spinal cord lesions may lead to permanent disability, significant morbidity, and even mortality. High spinal injuries often impair cardiorespiratory function, requiring emergent interventions.
Nerve axon disruption results in motor and sensory function loss below the SCI level.[rx] SCIs disproportionately affect people younger than 30, leading to significant lifelong functional impairment and possibly causing numerous health, financial, and psychosocial complications.rx] SCIs are estimated to have a lifetime economic impact of $2 to 4 billion.[rx][rx] The interventions range from initial emergency stabilization to stem cell therapies requiring long-term investment. The therapeutic approach is, therefore, important for clinicians along a vast medical care spectrum.

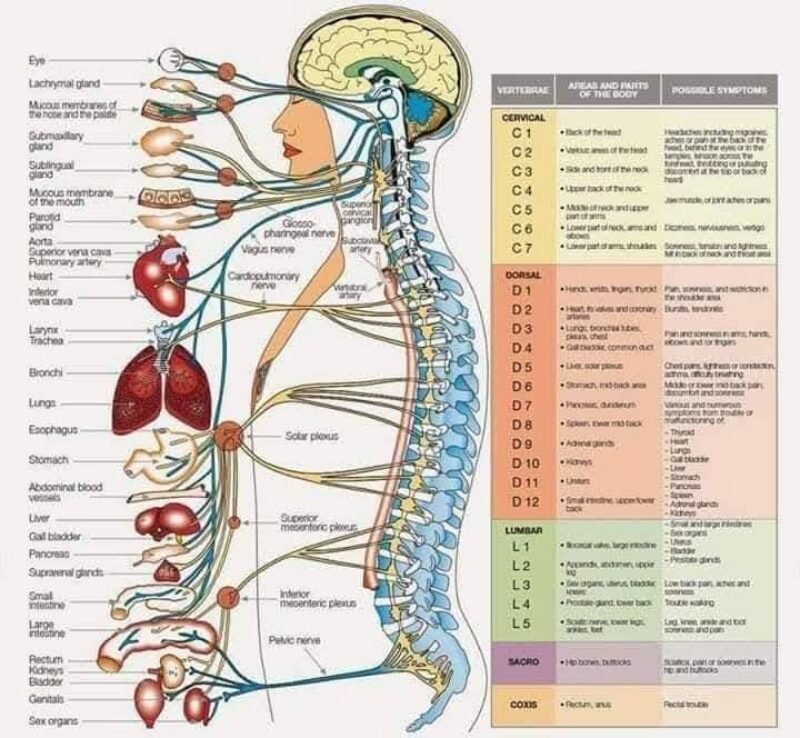
Spinal Cord Anatomy
The spinal cord contains several distinct regions based on the vertebral segment levels. Cervical nerves C1 to C8 supply the neck, shoulders, arms, and hands. Thoracic nerves T1 to T12 innervate the upper limb’s ulnar side and the trunk and abdominal muscles. Lumbar nerves L1 to L5 supply the lower back, buttocks, and lower limbs. Sacral nerves S1 to S5 innervate the pelvic organs, buttocks, genitals, and lower limbs. The coccygeal nerve C0 provides sensory innervation to the skin overlying the coccyx and surrounding areas and contributes to the pelvic floor muscles’ motor function. Spinal nerve distributions are best represented by dermatomal maps.
The cauda equina consists of spinal nerve roots L2 to S5, extending from the spinal cord’s lower end. The conus medullaris represents the spinal cord’s terminal portion, typically located at the L1 to L2 levels. The filum terminale anchors the spinal cord and dural sac to the coccyx and extends from the conus medullaris, providing structural support to the cord.
The spinal cord is a cylindrical nerve fiber bundle extending from the brain’s base down through the vertebral column. The cord transmits sensory and motor signals between the brain and the rest of the body. The spinal cord is divided into segments corresponding to the vertebral levels. Each segment gives rise to spinal nerves supplying specific body regions. The key structures within the spinal cord include the corticospinal (CST) and spinothalamic (STT) tracts and the dorsal columns (DC)—nerve pathways through which information exchange between the brain and body occurs.
The CST is a major motor pathway responsible for voluntary movement. This nerve tract originates from the cerebral cortex’s motor areas and descends through the brainstem and spinal cord. About 90% of the CST fibers travel on the spinal cord’s lateral side, forming the lateral CST (LCST). The LCST nerves travel throughout the cord. The rest of the fibers transit ventrally or anteriorly, forming the ventral CST (VCST). However, VCST fibers do not reach levels below the superior thoracic spinal segments.
The STT is a sensory pathway that relays pain and temperature information from the body to the brain. This nerve tract ascends through the anterolateral spinal cord and synapses in the thalamus before projecting to the somatosensory cortex.
The DC, also known as the posterior columns or dorsal funiculi, carry proprioceptive and tactile sensations (ie, touch, pressure, vibration) from the body to the brain. DC fibers ascend in the spinal cord’s posterior area and consist of the fasciculus gracilis (medial) and the fasciculus cuneatus (lateral).
SCIs give rise to a myriad of clinical manifestations, requiring different management strategies. Understanding the anatomy and organization of the spinal cord, including the locations of important nerve pathways, is essential for diagnosing and managing neurological conditions affecting motor and sensory function.
The spinal cord is a soft, cylindrical column of tightly bundled cells (nerve cells and glia), nerve fibers that transmit nerve signals (called axons), and blood vessels. It sends and receives information between the brain and the rest of the body. Millions of nerve cells in the spinal cord coordinate complex patterns of movements, such as rhythmic breathing and walking.
The spinal cord extends from the brain to the lower back through a canal in the center of the vertebrae. Like the brain, the spinal cord has three layers of tissue for protection—and cerebrospinal fluid (CSF) surrounds it to act as a cushion against shock or injury.
Other types of nerve cells sit just outside the spinal cord and send information to and from the brain. Doctors refer to these nerve cells based on their location:
- Cervical spinal nerves (known as C1 to C7) in the neck control signals to the back of the head, the neck and shoulders, the arms and hands, and the diaphragm.
- Thoracic spinal nerves (known as T1 to T12) in the upper mid-back control signals to the chest muscles, some muscles of the back, and many organ systems.
- Lumbar spinal nerves (known as L1 to L5) in the lower mid-back control signals to the lower parts of the abdomen and the back, the buttocks, some parts of the external genital organs, and parts of the legs.
- Sacral spinal nerves (known as S1 to S5) in the lower back control signals to the thighs and lower parts of the legs, the feet, most of the external genital organs, and the area around the anus.
| Level | Motor Function | Respiratory function |
|---|---|---|
| C1–C4 | Full paralysis of the limbs | Cannot breathe without mechanical ventilation |
| C5 | Paralysis of the wrists, hands, and triceps | Difficulty coughing; may need help clearing secretions |
| C6 | Paralysis of the wrist flexors, triceps, and hands | |
| C7–C8 | Some hand muscle weakness, difficulty grasping and releasing |
Spinal Cord Neurons
The central nervous system contains more than 100 billion neurons. Neurons are the simplest units that make up the nervous system and are similar to the makeup of any other cell within the body except for their vast potential to relay information through chemical and electrical signals. Through nerve impulses, neurons can communicate messages as far as several feet!
There are four types of neurons:
- Motor neurons: Neurons that relay messages between muscles, organs, and glands.
- Sensory neurons: Neurons that send signals to the brain and spinal cord from external stimuli and internal organs.
- Interneurons: Neurons that relay signals between sensory and motor neurons.
- Receptors: Neurons that collect information from the environment and communicate messages through the sensory neurons.
Every nerve has a specific job for feeling, sensation, and movement and varies in size and responsibility. The nerves communicate to each part of the body how and when to move, and send messages back to the brain about the current environment. Patients can experience debilitating effects when this signal is compromised. In the case of a spinal cord injury in which a portion of the tissue is severed, these neurons are unable to function properly, resulting in permanent or temporary loss of sensation and movement and/or paralysis.
Types of spinal cord injury
SCI Mechanisms
SCIs arise from complex mechanisms, producing varying degrees of neurologic deficits depending on the injury’s location and extent. The processes driving SCIs are classified as either primary or secondary. The spinal cord lesions may give rise to unique, clinically identifiable syndromes. These concepts are further explained below.
Primary injury
A primary SCI develops from mechanical forces directly damaging the cord. The most common primary SCI mechanism is direct cord trauma, followed by persistent compression from space-occupying pathologies like vertebral fractures, malignancies, hematomas, and abscesses. Hyperextension injuries typically result from transient compression rather than impact alone, unlike fracture-dislocations.
Other common primary SCI mechanisms include distraction injuries and lacerations. A distraction injury arises from a spinal cord stretch and tear in its axial plane, typically when 2 adjacent vertebrae are pulled apart. A laceration or transection injury may come from sources such as sharp bone fragments, severe dislocations, and missile penetration.
Secondary injury
A secondary SCI emerges from a series of biological phenomena that begin within minutes of a primary injury and continue for weeks or months. The acute secondary injury phase encompasses vascular damage, ionic imbalances, free-radical formation, the initial inflammatory response, and neurotransmitter accumulation (excitotoxicity).[5]
SCI Phases
The phases of an SCI are summarized in the table below.
Post-SCI Immune Response
Post-SCI neuroinflammation exhibits a dual nature, potentially causing both beneficial and deleterious outcomes, depending on the timing and immune cells present at the injury site. In the initial 3 days post-injury, blood-born neutrophils, resident microglia, and astrocytes are recruited to the injury site, initiating the inflammatory response. A second phase ensues around 3 days postinjury, attracting macrophages, and B and T lymphocytes. Antigen-presenting cells activate CD4+ helper T cells to release cytokines, stimulating B cells to produce antibodies and intensifying neuroinflammation and tissue destruction. Notably, neuroinflammation is most pronounced during the acute SCI phase.
Inflammation is protracted in the subacute and chronic phases. The inflammatory cell composition and phenotype vary with the inflammation stage and signal molecules within the injury microenvironment. T and B cells and microglia or macrophages can gain a pro-inflammatory or anti-inflammatory pro-regenerative phenotype. Spinal cord disruption leads to motor and sensory function deficits below the injury level. Disability patterns depend on the injury level and extent of spinal tract involvement.[rx][rx]
STT damage results in contralateral pain and temperature sensation loss. CST disruption leads to ipsilateral weakness or paralysis. In the cervical spine, CST fibers supplying the upper extremities are proximal to the center of the spinal cord. In contrast, CST nerves to the lower extremities are located distally. DC injury leads to ipsilateral loss of tactile, proprioceptive, and vibratory sensations.
Spinal Cord Syndromes
Several SCI patterns are well described. The origins and manifestations of these different spinal cord syndromes are explained below.[rx][rx][rx]
Complete spinal cord transection
Complete spinal cord transections typically demonstrate total bilateral loss of motor function and pain, temperature, proprioceptive, vibratory, and tactile perception below the injury level. Lumbosacral injuries present with lower extremity sensorimotor deficits and bowel, bladder, and sexual dysfunction. Thoracic injuries lead to the same deficits as lumbosacral injuries and, in addition, may result in torso motor weakness, producing postural difficulties. Cervical injuries lead to the same deficits as thoracic injuries but with added upper limb function loss, leading to tetraplegia. High-spinal injuries above C5 may also cause respiratory compromise due to loss of diaphragm innervation.[10]
Central cord syndrome
Central cord syndrome is the most frequently occurring incomplete SCI. This type of injury develops from neck hyperextension, thus compressing the cervical spinal cord and damaging the cord’s center. This injury more often produces upper extremity than lower extremity weakness. This pattern emerges due to the CST’s arrangement, where axons supplying the upper extremities are positioned closer to the spinal cord’s center, while those serving the lower extremities are nearer the periphery. Pain and temperature sensation loss may be noted below the level of injury.
Anterior cord syndrome
This condition is classically due to compromised blood flow in the anterior spinal artery. Bilateral STT injuries lead to bilateral pain and temperature perception loss below the level of injury. Bilateral CST injuries paralyze the muscles below the injury level. Tactile and vibration sensations and proprioception remain intact, as dorsal columns are unaffected.
Posterior cord syndrome
This injury pattern occurs more frequently from infectious, toxic, or metabolic than traumatic causes. DC damage weakens tactile, vibratory, and proprioceptive perception. Pain and temperature sensory and motor function are preserved owing to the lack of STT and CST involvement.
Brown-Séquard syndrome
This condition results from right- or left-sided spinal cord hemisection. CST and DC transection lead to ipsilateral loss of motor function, proprioception, and tactile and vibratory sensations below the injury level. STT disruption produces contralateral pain and temperature perception deficits below the level of injury.[11]
Conus medullaris syndrome
This injury pattern develops from terminal spinal cord damage at an area proximal to the cauda equina. Conus medullary syndrome characteristically presents with sacral nerve dysfunction, manifesting as the loss of Achilles tendon reflexes and bowel, bladder, and sexual function.
Neurogenic shock
High cervical injuries can damage the cervical ganglia. These injuries lead to a loss of sympathetic tone, producing neurogenic shock—a state characterized by hypotension and bradycardia.[rx]
An SCI can be either complete or incomplete:
- An incomplete injury means the spinal cord is still able to send some messages to or from the brain. People still have some feeling, function, and muscle control below the site of their injury.
- A complete injury means that there is no nerve communication below the injury site. People lose muscle control, feeling, or function below the injury.
Causes
pinal cord injuries are most often caused by physical trauma.[rx] Forces involved can be hyperflexion (forward movement of the head); hyperextension (backward movement); lateral stress (sideways movement); rotation (twisting of the head); compression (force along the axis of the spine downward from the head or upward from the pelvis); or distraction (pulling apart of the vertebrae).[rx] Traumatic SCI can result in contusion, compression, or stretch injury.[rx] It is a major risk of many types of vertebral fracture.[rx] Pre-existing asymptomatic congenital anomalies can cause major neurological deficits, such as hemiparesis, to result from otherwise minor trauma.[rx]
Causes of Spinal Cord Injury
-
Motor vehicle accidents: Leading cause of traumatic SCI in many countries Mayo Clinic
-
Falls: Especially in older adults, can fracture vertebrae and injure the cord Mayo Clinic
-
Sports and recreational injuries: Diving, football, gymnastics accidents Mayo Clinic
-
Violence (gunshot, stabbing): Penetrating trauma damaging cord tissue Mayo Clinic
-
Tumors: Primary or metastatic spinal cord compression Verywell Health
-
Infections: Epidural abscess, meningitis Verywell Health
-
Vascular disorders: Spinal cord infarction, arteriovenous malformations Verywell Health
-
Degenerative diseases: Spinal stenosis from osteoarthritis Verywell Health
-
Herniated discs: Acute compression of cord or nerve roots Mayo Clinic
-
Osteoarthritis: Bone spurs narrowing the canal Verywell Health
-
Rheumatoid arthritis: Inflammatory destruction leading to instability Verywell Health
-
Multiple sclerosis: Demyelinating lesions within cord Verywell Health
-
Transverse myelitis: Inflammatory injury of spinal cord segments Verywell Health
-
Syringomyelia: Fluid-filled cavity in cord compressing tissue Verywell Health
-
Cauda equina syndrome: Nerve root compression by tumors or herniation Verywell Health
-
Epidural hematoma: Bleeding into epidural space compressing cord Mayo Clinic
-
Spina bifida and other congenital defects: Malformations leading to cord tethering Verywell Health
-
Radiation injury: Post-radiotherapy damage to neural tissue Verywell Health
-
Iatrogenic injuries: Surgical complications injuring cord or roots Mayo Clinic
-
Metabolic disorders: Vitamin B₁₂ deficiency causing subacute combined degeneration Verywell Health
- Soldier, armies on the battlefield – With the increasing technology of nuclear weapons on the battlefield, one country is involved in the war from one country to another country. On the battlefield, millions of armies and general people are falling into injury.
- Have osteoporosis – a disease of your bone that weakens your bones gradually due to inadequate intake of calcium or vitamin D, less exposure to sunlight may lead to fracture of the bone in older age.
- Weak low muscle mass or poor muscle strength – Lack of agility or older age muscle strength, mass, power, endurance becomes weak, and poor balance conditions make you more likely to fall and cause a fracture.
- Walk or do other activities in the snow or on the ice – Especially north region of the world maximum time is low temperature. That frequent water turns into snow and activities that require a lot of forwarding momenta, such as in-line skating and skiing, snowboarding, in-line skating, Jumping, and playing lead to fracture of the bone in the upper limb.
- Insufficient vitamin D and sunlight – Insufficient vitamin D and sunlight decrease the intestinal absorption of calcium, leading to abnormal regulation of parathyroid hormone (PTH). Vitamin D also works to upregulate the transcription of genes involved in neovascularization in areas of endochondral ossification, such as a healing fracture site. Vitamin D deficiency is typically characterized as a serum level of 25-hydroxyvitamin D3 of less than 20 ng/mL, and sufficiency is between 20 and 31 ng/mL.[rx]

Symptoms
The symptoms of spinal cord injuries depend on the part of the spinal cord that is damaged and how much damage there is. SCIs to upper parts of the spinal cord affect more of the body than injuries lower down. An injury to the upper part of the spinal cord can cause paralysis in most of the body and affect all limbs (tetraplegia or quadriplegia).
An injury that happens lower down the spinal cord may only affect a person’s lower body and legs (paraplegia). Paralysis can happen immediately upon injury (primary damage) or develop over time from bleeding and swelling in the spinal cord and cell death (secondary damage).
An SCI can damage a few, many, or almost all of the nerve fibers that cross the site of injury. If the injury causes little or no nerve cell death, a person can make an almost complete recovery.
An SCI can cause one or more symptoms, including:
- Numbness, tingling, or a loss of (or changes in) sensation in hands and feet
- Paralysis (loss of movement)
- Pain or pressure in the head, neck, or back
- Weakness in any part of the body
- Unnatural or uncomfortable positions of the spine or head
- Loss of bladder and bowel control
- Problems with walking
- Difficulty breathing
- Changes in sexual function
- partial or complete loss of sensory and/or motor functions (including respiratory muscle functions)
- bowel, bladder and sexual dysfunction
- dysregulation of blood pressure, heart rate, and/or body temperature.
The symptoms of an SCI depend on the affected signals. There are three types of signals that an SCI can affect: sensory, motor and autonomic.
Sensory symptoms
Sensory signals carry information to your brain. They tell your brain about the world around you and what’s happening to your body.
Your spinal cord mainly handles tactile (touch-based) signals. Examples include temperature, pressure, vibration, texture, etc. It also handles your self-positioning sense (proprioception). If you move your hand toward your face in a totally dark room but can stop your hand before it touches your nose, that’s an example of proprioception.
Examples of sensory symptoms include:
- Pain.
- Numbness.
- Tingling or “pins-and-needles” (paresthesia).
Motor symptoms
Motor signals travel from your brain to your muscles. They’re how your brain moves parts of your body.
Motor symptoms can include:
- Weakness (reduced strength).
- Paralysis (lack of muscle control).
- Spasticity (muscles that remain flexed uncontrollably).
Autonomic symptoms
Autonomic signals run processes you don’t have to think about (“autonomic” sounds like “automatic,” and autonomic signals handle automatic processes).
Autonomic symptoms can include:
- Heart rate disruptions, especially slow heart rate (bradycardia).
- Blood pressure disruptions, especially low blood pressure (hypotension).
- Body temperature disruptions, especially low body temperature (hypothermia).
- Urinary incontinence or fecal incontinence.
- Erectile dysfunction.
SCI is often associated with a risk of developing complications, including debilitating and potentially life-threatening secondary conditions, such as
- spasticity
- (chronic) pain
- urinary tract infections
- pressure ulcers
- respiratory complications
- autonomic dysreflexia
- deep vein thrombosis
- osteoporosis.
| Level | Motor Function |
|---|---|
| C1–C6 | Neck flexors |
| C1–T1 | Neck extensors |
| C3, C4, C5 | Supply diaphragm (mostly C4) |
| C5, C6 | Move shoulder, raise arm (deltoid); flex elbow (biceps) |
| C6 | externally rotate (supinate) the arm |
| C6, C7 | Extend elbow and wrist (triceps and wrist extensors); pronate wrist |
| C7, T1 | Flex wrist; supply small muscles of the hand |
| T1–T6 | Intercostals and trunk above the waist |
| T7–L1 | Abdominal muscles |
| L1–L4 | Flex thigh |
| L2, L3, L4 | Adduct thigh; Extend leg at the knee (quadriceps femoris) |
| L4, L5, S1 | abduct thigh; Flex leg at the knee (hamstrings); Dorsiflex foot (tibialis anterior); Extend toes |
| L5, S1, S2 | Extend leg at the hip (gluteus maximus); Plantar flex foot and flex toes |
Motor vehicle accidents and serious falls are the most common causes of SCI in the U.S. Other causes include:
- Acts of violence (mostly gunshot wounds and assaults)
- Sports injuries
- Medical or surgical injuries
- Industrial or workplace accidents
- Diseases
- Conditions that can damage the spinal cord
Risk factors for an SCI include age (either being between ages 16 and 30, or after age 65 for dangerous falls), alcohol use, or not wearing proper gear—such as a seat belt or protective sports equipment.

Diagnosing spinal cord injuries
After an injury or accident, an emergency room doctor will check for movement or sensation at or below a suspected SCI. They will also check for proper breathing, responsiveness, and weakness.
- A physical exam. Your provider does this to look for clues or evidence of the injury’s extent.
- A neurological exam. Your provider will do this to test specific abilities of your nervous system. This involves seeing if you can move your limbs by testing your strength and checking your sensation and reflexes.
Severity of injury is often conveyed through the 5-level American Spinal Injury Association (ASIA) impairment scale as described below:
- Grade A: Complete; No sensory or motor function preserved in the sacral segments S4 – S5 (near the tailbone)
- Grade B: Incomplete; Sensory but no motor function preserved below the neurological level and extending through the sacral segment S4 – S5
- Grade C: Incomplete; Motor function preserved below the neurological level; Most key muscles have a grade < 3 (cannot raise muscles against gravity)
- Grade D: Incomplete; Motor function preserved below the neurological level; Most key muscles have a grade > 3 (can raise muscles against gravity)
- Grade E: Normal motor and sensory function
What happens during a neurological examination?
Next, the provider will do specific tests to check how different parts of your nervous system are working. The tests you have will depend on your symptoms. The examination may include tools such as a tuning fork (to test for hearing loss and as part of a sensory exam), flashlight, or a reflex hammer. The tests may check your:
- Mental status. This includes your memory, problem-solving ability, alertness, and mood. During a mental status exam, you may answer questions about the date, time, and where you are. You may also be asked to remember a list of items, name objects, repeat words, and/or draw specific shapes.
- Cranial nerves. These 12 nerves connect your brain with your eyes, ears, nose, face, tongue, throat, shoulders, and certain organs. The provider will test the nerves that may be involved with your symptoms. For example, to test your sight, you may be asked to read a letter chart. To test the muscles in your face, you may be asked to smile or close your eyes tightly.
- Movement and strength. Muscles respond to signals from the brain and nervous system and can help doctors identify problems with the brain and spinal cord. During a neurological examination, doctors will test the strength and flexibility of your muscles. You may be asked to keep your fingers spread apart while the provider gently pushes them together, or to relax your arm while they move it back and forth.
- Coordination, balance, and walking. These tests check how well your nervous system controls your muscle movements. You may be asked to walk in a straight line placing one foot directly in front of the other. Other tests include checking your handwriting and having you touch your finger to your nose with your eyes closed.
- Reflexes. A reflex is your body’s automatic movement in response to certain triggers. For example, if your knee is tapped with a rubber hammer, your lower leg will jerk on its own. There are many types of reflexes that are tested in different ways. Reflex tests show how well nerves that send signals between your spinal cord and muscles are working.
- Sensory nerves. The doctor may test how well you can feel touch, hot and cold temperatures, vibrations, and pain. These tests involve gently touching parts of your skin with different objects, such as a sharp object or a cotton swab. You will be asked to describe what you can feel.
- Autonomic nervous system. A neurological exam tests the part of your nervous system that controls your breathing, heart rate, digestion, and other processes that happen without thinking. Examples of these tests include checking your blood pressure and heartbeat.
In infants and young children, many of these parts of the exam are based on observation or engagement in play activities.
The results of the neurological examination and the person’s history help determine a list of possibilities, known as the differential diagnosis, that determine if more diagnostic tests and procedures are needed.
If the results of any part of your neurological exam are not normal, your doctor will probably order more tests to help make a diagnosis. These screening tests will depend on what type of condition your doctor thinks you may have.
Laboratory tests
Laboratory tests of blood, urine, or other body fluids may help doctors diagnose disease or understand disease severity. These tests can also help monitor levels of medications in the body to help determine if the person is taking the right dose. Certain tests, ordered by the physician as part of a regular checkup, give general information, while others can identify specific health concerns:
- Blood tests can detect infections, toxins, clotting disorders, or antibodies that show the presence of an autoimmune disease. They can also monitor levels of drugs that treat epilepsy and other neurological disorders in the body.
- Genetic testing of DNA extracted from cells in the blood or saliva can help diagnose hereditary disorders
- Analysis of cerebrospinal fluid (the fluid that surrounds the brain and spinal cord) can detect meningitis, encephalitis, acute and chronic inflammation, viral infections, multiple sclerosis, and certain neurodegenerative disorders
- Chemical and metabolic testing of the blood can point to some muscle disorders, protein or fat-related disorders that affect the brain, and metabolic problems
- Urine tests can reveal toxins, abnormal metabolic substances, proteins that cause disease, or signs of certain infections
Genetic testing
Genetic testing of people with or without a family history of a neurological disease can determine if they are carrying one of the genes known to cause the disorder. Genetic counseling may help people understand the purpose of the tests and what the results could mean. Genetic testing for diagnosis or treatment should be done in a laboratory that has been certified for clinical testing. Clinical testing can look for disease-causing mutations in specific genes or in regions of several genes. This testing may use a panel of genes for a specific type of disease (for example, infant-onset epilepsy) or a test known as whole exome sequencing. Exomes are the parts of the genome formed by exons, which code for proteins. Whole genome sequencing is also now used in certain cases. Exome and genome sequencing may take several months to analyze. Clinicians and researchers also sequence whole exomes or whole genomes to discover new genes that cause neurological disorders.
Prenatal genetic testing for neurological disorders
Prenatal genetic testing can identify many neurological disorders and genetic abnormalities before birth.
- A pregnant person’s blood can be screened for abnormalities that suggest a risk for a genetic disorder.
- A type of blood test called a quadruple or quad screen may help identify some genetic disorders, including trisomies (which cause disorders such as Down syndrome) in a fetus. A blood sample measures the levels of four substances: alpha-fetoprotein, human chorionic gonadotropin, estriol, and inhibin-A. The test is done between 15 and 20 weeks of pregnancy. It usually takes several days to receive results from a quad screen. Abnormal results of a quad screen may point to spina bifida or a chromosome abnormality. However, false positive results are not uncommon, so more testing may be needed.
- Amniocentesis is usually done at 14-16 weeks of pregnancy if there is a suspected problem with the fetus. It tests a sample of the amniotic fluid in the womb for genetic defects. Under local anesthesia (anesthesia that is given while you are awake for a short time to stop pain in one part of the body), a thin needle is inserted through the abdomen and into the womb. About 20 milliliters of fluid (roughly 4 teaspoons) is withdrawn and sent to a lab for evaluation. Test results often take 1-2 weeks.
- Chorionic villus sampling is done at 10-13 weeks of pregnancy. The procedure removes and tests a very small sample of the placenta. The sample, which contains the same DNA as the fetus, is taken out by catheter or fine needle inserted through the cervix or by a fine needle inserted through the abdomen. Chorionic villus sampling is usually only done if there is a high risk of a genetic abnormality, for example, if the mother is age 35 or older or one of the parents has a family history of a genetic condition. Results are usually available within 2 weeks.
Brain scans
Brain scans include several types of imaging techniques that diagnose tumors, blood vessel malformations, stroke, inflammation, injuries, scars, abnormal brain development, and hemorrhage in the brain. Types of brain scans include CT (computed tomography), MRI (magnetic resonance imaging), PET (positron emission tomography), and SPECT (single proton emission CT). The type of scan that will be recommended depends on the results of the neurological exam and the person’s symptoms. Brain scans are done by skilled technicians in a hospital or at an outpatient testing facility.
Computed tomography (CT scan)
Computed tomography (CT scan) uses X-rays to produce two- and three-dimensional images of organs, bones, and tissues. A CT scan can aid in proper diagnosis by showing the area of the brain that is affected. CT scans can quickly detect bleeding in the brain and determine if someone who has had a stroke can safely receive IV treatment to dissolve clots. CT scans can also help detect bone and blood vessel irregularities, brain tumors and cysts, hydrocephalus (build-up of cerebrospinal fluid in the brain), or brain damage from an injury. A CT of the spine can show herniated discs, spine fractures, or spinal stenosis.
CT scans are especially useful in people who can’t have an MRI. Because CT uses X-rays, pregnant people have them only under limited circumstances (typically, emergencies) because of potential harm to the fetus.
During a CT scan:
- CT scanning takes about 20 minutes and is usually done at an outpatient imaging center or in a hospital.
- The person lies on a special table that slides into a narrow, doughnut-shaped chamber.
- A sound system built into the chamber allows the person to communicate with the physician or technician. X-rays (ionizing radiation) are passed through the body at various angles and are detected by a computerized scanner.
- The data is processed and displayed as cross-sectional images, or “slices,” of the internal structure of the body or organ.
- Occasionally, a light sedative may be given if the person is unable to lie still. Pillows can support and stabilize the head and body.
- Sometimes, a contrast dye is injected into the bloodstream to highlight the different tissues in the brain. If a contrast dye is injected into a vein, the person being scanned may feel a warm or cool sensation as the dye circulates through the bloodstream or may experience a slight metallic taste.
Magnetic resonance imaging (MRI)
Magnetic resonance imaging (MRI) uses computer-generated radio waves and a powerful magnetic field to produce detailed images of body tissues. Using different sequences of magnetic pulses, MRI can show images of the brain or spinal cord, measure blood flow, or reveal deposits of minerals such as iron. MRI can help diagnose stroke, traumatic brain injury, brain and spinal cord tumors, inflammation, infection, vascular problems, scars, abnormally developed brain regions, and some neurodegenerative disorders. MRI can also help diagnose and monitor multiple sclerosis.
The test is painless and risk-free, although people with obesity or people who are claustrophobic may find it somewhat uncomfortable—the machine can also be noisy. Some centers use open MRI machines that do not completely surround the person being tested and are less confining. However, open MRI does not currently provide the same picture quality as standard MRI.
During an MRI:
- A contrast dye may be injected into the vein to better show certain areas or tissues. If intravenous contrast is required, people may first need a blood test to check kidney function because the contrast agent, called gadolinium, can increase the risk of a rare disease in people with advanced kidney disease.
- An MRI scanner has a tube surrounded by a very large cylinder-shaped magnet.
- The person lies on a special table that slides into the tube and will be asked to remove jewelry, eyeglasses, removable dental devices, clothing with metal, and other items that might interfere with the magnetic imaging. Because people must remain still during the MRI, very young children (or those with certain medical conditions) may need to be sedated to be scanned.
- For brain MRI scans, a detector is placed over the head.
- The person may hear grating or knocking noises when the magnetic field direction is flipped. Earphones or earplugs can help block out the sounds.
- MRI scanners create a magnetic field around the body that’s strong enough to temporarily realign water molecules in the tissues. Radio waves are then passed through the body to detect the shifting of molecules back to a random order.
- A computer then reconstructs a three-dimensional picture or a two-dimensional “slice” of the tissue being scanned.
- MRI can tell the difference between bone, soft tissues, and fluid-filled spaces because of differences in water content and tissue properties.
- Depending on the part(s) of the body to be scanned, MRI can take up to an hour to complete.
Due to the incredibly strong magnetic field generated by an MRI, people with implanted medical devices such as a pacemaker or infusion device generally should not have MRIs. In certain situations, facilities may have equipment to temporarily stop and reset the implanted device’s programming to allow the person to receive an MRI. A fetal MRI may be ordered when prenatal ultrasound reveals a possible problem. Fetal MRI is considered safe for the fetus because it doesn’t use radiation or contrast dye.
Functional MRI (fMRI)
Functional MRI (fMRI) uses the blood’s magnetic properties to create real-time images of blood flow to specific areas of the brain. fMRI can pinpoint areas of the brain that become active and show how long they stay active. This imaging process can help identify brain regions that are critical for language, motor function, or sensation before surgery for epilepsy. Researchers use fMRI to study head injury and degenerative disorders such as Alzheimer’s disease.
Positron emission tomography (PET)
Positron emission tomography (PET) scans create two- and three-dimensional pictures of brain activity by measuring radioactive isotopes that are injected into the bloodstream. PET scans of the brain can detect or highlight tumors and diseased tissue, show blood flow, and measure cellular and/or tissue metabolism. PET scans can evaluate people who have epilepsy or certain memory disorders and show brain changes following injury. PET may be ordered as a follow-up to a CT or MRI scan to give the physician a greater understanding of activity in specific areas of the brain.
During a PET scan:
- A low-level radioactive isotope, also called a tracer, is injected into the bloodstream. The PET scan measures where tracer goes in the brain.
- The person lies still while overhead sensors detect gamma rays in the body’s tissues.
- A computer processes the information and displays it on a video monitor or on film.
- Using tracers, more than one brain function can be traced at the same time.
- PET is painless and uses small amounts of radioactivity.
- The length of test time depends on the part of the body to be scanned.
Single photon emission computed tomography (SPECT)
Single photon emission computed tomography (SPECT) is a nuclear imaging test that can evaluate certain brain functions. As with a PET scan, a tracer is injected into the body. A SPECT scan may be ordered as a follow-up to an MRI to diagnose tumors, infections, brain regions involved in seizures, degenerative spine disease, and stress fractures.
During a SPECT scan:
- The person lies on a table while a gamma camera rotates around the head and records where the tracer has traveled.
- That information is converted by computer into cross-sectional slices that are stacked to produce a detailed three-dimensional image of the tracer within the brain.
A person who experiences a seizure can get two scans after they’re medically stable—one as an initial baseline scan and after a tracer is injected.
A dopamine transport single-photon emission computed tomography scan (DaTscan) can help diagnose Parkinson’s disease.
Lisa’s Story
Lisa, age 30, had been feeling some stiffness in her muscles and dizziness. She often found it difficult to stay balanced while walking. Lisa scheduled an appointment with her doctor, who performed a physical exam. The doctor referred her to a neurologist for an MRI (magnetic resonance imaging) scan based on her symptoms. The MRI results showed signs of multiple sclerosis. They prescribed Lisa medicines to help with her symptoms and recommended lifestyle changes.
Angiography
Angiography involves injecting dye into the arteries or veins to detect blockage or narrowing. A cerebral angiogram can show narrowing or obstruction of an artery or blood vessel in the brain, head, or neck. It can determine the location and size of an aneurysm or vascular malformation. Angiograms are used in certain strokes where there is a possibility of unblocking the artery using a clot retriever. A spinal angiogram can help detect problems in the spinal cord blood vessels—such as malformations or blockages in arteries. Angiograms can also show the blood supply of a tumor before an operation and are usually done in a hospital or at an outpatient testing facility.
During an angiogram:
- The person lies on a table that is wheeled into the imaging area.
- A physician numbs a small area of the leg near the groin and then inserts a catheter into a major artery located there.
- They then thread the catheter through the body and into an artery in the neck.
- The technician injects a dye that travels through the bloodstream into the head and neck and takes a series of X-rays. The person may feel a warm to hot sensation or slight discomfort as the dye is released.
- This may take up to 3 hours, followed by a 6- to 8-hour resting period.
In many situations, brain angiograms have been replaced by specialized MRI scans, called MR angiograms (MRA), or CT angiograms.
Biopsy
Biopsy involves the removal and examination of a small piece of tissue from the body. Muscle or nerve biopsies can help diagnose neuromuscular disorders. A skin biopsy can measure small nerve fibers or test for certain metabolic disorders. They are usually done in an outpatient testing facility.
During a biopsy:
- A small sample of the muscle, skin, or nerve is removed under local anesthetic.
- The muscle sample may be removed either surgically, through a slit made in the skin, or by needle biopsy, in which a thin hollow needle is inserted through the skin and into the muscle. A nerve may be removed through a small surgical incision near the ankle, or occasionally near the wrist.
A brain biopsy, which can help determine the type of tumor a person has and identify certain infections, requires surgery to remove a small piece of the brain or tumor. It is an invasive procedure that carries some risks.
Cerebrospinal fluid analysis
Cerebrospinal fluid analysis involves the removal of a small amount of the fluid that surrounds the brain and spinal cord. The procedure commonly requires a lumbar puncture or spinal tap, which may be done as an inpatient or outpatient procedure. The fluid is tested to detect evidence of brain hemorrhage (bleeding), infection, multiple sclerosis, metabolic diseases, or other neurological conditions.
During a cerebrospinal fluid analysis:
- The person will either lie on one side with their knees pulled up to their chest or lean forward while sitting on a table, bed, or chair.
- The person’s back is cleaned and injected with a local anesthetic.
- The injection may cause a slight stinging sensation.
- Once the anesthetic has taken effect, a special needle is inserted between the vertebrae into the spinal cord and a small amount of fluid (usually about three teaspoons) is withdrawn for testing.
- Most people will only feel a sensation of pressure as the needle is inserted.
- Generally, people are asked to lie flat for 1-2 hours after the procedure to reduce the likelihood that they will get a headache, which can happen after a lumbar puncture due to low spinal fluid levels.
There is a small risk of nerve root injury or infection from a lumbar puncture. The procedure takes about 45 minutes.
Electroencephalography
Electroencephalography, or EEG, monitors the brain’s electrical activity through the skull. EEG helps diagnose seizure disorders and other disorders that affect the brain’s activity. EEGs also evaluate sleep disorders and monitor brain activity when a person has been fully anesthetized or loses consciousness. EEG is a painless, low-risk test that can be done in a doctor’s office or at a hospital or testing facility.
During an EEG:
- The person being tested usually reclines in a chair or on a bed.
- A series of small cup-like electrodes are attached to the scalp with a special conducting paste. The electrodes are attached to wires that carry the electrical signals of the brain to a machine.
- During an EEG, a variety of external stimuli, including bright or flashing lights or certain drugs may be given.
- People may be asked to open and close their eyes, or to change their breathing patterns.
- Changes in brain wave patterns are transmitted from the electrodes to an EEG machine or computer.
- An EEG test usually takes about an hour (including set-up time).
Testing for certain disorders, such as seizure or sleep disorders, may require doing a much longer EEG during sleep, which takes about 4 hours.
In people undergoing evaluation for epilepsy surgery:
- Electrodes may be inserted through a surgical opening in the skull to reduce signal interference. This is called an intracranial electrocorticography (ECoG).
- People stay in a hospital epilepsy monitoring unit while implanted electrodes are in place.
- During this time, the brain is monitored for seizures to figure out where they originate.
- People may also be asked to do certain types of tasks (e.g., reading, speaking, or certain movements) so the ECoG can help identify brain regions that are important for normal function and that should be avoided during the surgery.
Electromyography
Electromyography, or EMG, can diagnose nerve and muscle disorders, spinal nerve root compression, and motor neuron disorders such as amyotrophic lateral sclerosis (ALS). EMG records the electrical activity in the muscles. Testing may take place in a doctor’s office or clinic.
During an EMG:
- Very fine needles or wires are inserted into a muscle to analyze changes in electrical signals at rest and during movement, which can point to nerve or muscle damage.
- The needles are attached to an EMG machine.
- Testing usually lasts an hour or longer, depending on the number of muscles and nerves to be tested.
- Because of a slight risk of bruising or bleeding, people will be asked if they are on aspirin or blood thinners before they are given EMG.
- Most people find this test to be somewhat uncomfortable.
Nerve conduction study
An EMG is usually done in conjunction with a nerve conduction study (NCS). An NCS measures the nerve’s ability to send a signal, as well as the speed (nerve conduction velocity) and size of the nerve signal.
During an NCS:
- A set of electrodes is taped to the skin over the muscles.
- Wires connect the electrodes to an EMG machine.
- A small electrical pulse (like the sensation of static electricity) is given on the skin a short distance away to stimulate the nerve.
- The electrical signal is viewed on the EMG machine as it travels along the nerve.
- The physician then reviews the nerves’ response to verify any nerve damage or muscle disease.
- There is minimal discomfort and no risk associated with this test.
Electronystagmography
Electronystagmography (ENG) describes a group of tests to diagnose involuntary eye movement, dizziness, and balance disorders. The test is done at a clinic or imaging center.
During an ENG:
- Small electrodes are taped on the skin around the eyes to record eye movements.
- If infrared photography is used instead of electrodes, the person being tested wears special goggles that help record the information.
- Both versions of the test are painless and carry little or no risk.
Evoked potentials
Evoked potentials, also called evoked responses, include three tests that measure the electrical signals to the brain generated by sound, touch, or sight. Evoked potentials test sight and hearing (especially in infants and young children) and can help diagnose multiple sclerosis, spinal cord injury, and acoustic neuroma (small tumors of the acoustic nerve). Evoked potentials also monitor brain activity in coma patients and confirm brain death. Testing may take place in a doctor’s office or hospital setting.
During the procedure:
- One set of electrodes is attached to the person’s scalp with conducting paste. Electrodes may also be attached to other parts of the body, such as the ears, arms, or legs.
- The electrodes measure the brain’s electrical response to auditory, visual, and electrical stimuli.
- A machine records how much time it takes for impulses generated by stimuli to reach the brain.
- Auditory evoked potentials (also called brain stem auditory evoked response) can assess hearing loss and damage to the acoustic nerve and auditory pathways in the brain stem. They can also detect acoustic neuromas. The person being tested sits in a soundproof room and wears headphones. Clicking sounds are delivered one at a time to one ear while a masking sound is sent to the other ear. Each ear is usually tested twice, and the entire procedure takes about 45 minutes.
- Visual evoked potentials detect loss of vision from optic nerve damage (for example from multiple sclerosis). The person sits close to a screen and is asked to focus on the center of a shifting checkerboard pattern. One eye is tested at a time. Each eye is usually tested twice. Testing takes 30-45 minutes.
- Somatosensory evoked potentials (SSEPs) measure responses from electrical stimuli to the nerves. In addition to electrodes on the scalp, electrodes are pasted to the arms, legs, and back to measure the signal as it travels from the peripheral nerves to the brain. Tiny electrical shocks are delivered by electrodes pasted to the skin over a nerve in an arm or leg. SSEPs may help diagnose multiple sclerosis, spinal cord compression or injury, and certain metabolic or degenerative diseases. SSEP tests usually take longer than an hour.
Myelography
Myelography involves the injection of a contrast dye into the spinal canal to enhance imaging of the spine by CT or X-ray. If you have chronic back pain, a doctor will likely suggest a CT scan or MRI first. But if these don’t explain what is causing the pain, a myelogram can show certain issues that a doctor can’t see with a CT scan or MRI. For example, myelograms can identify cysts (fluid filled sacs) in the brain and tears in the brain’s dura mater, which can be a complication of surgery or can follow an injury. Myelography can be done as an outpatient procedure at a hospital or medical center.
During myelography:
- Local anesthesia is injected into a site between two vertebrae in the lower back and a small amount of the cerebrospinal fluid is removed by spinal tap.
- Contrast dye is injected into the spinal column and a CT scan or a series of X-rays is taken.
- People may experience some pain during the spinal tap as well as headache following the procedure.
- There is a slight risk of fluid leakage or allergic reaction to the dye.
- The procedure takes about one hour.
Polysomnogram
A polysomnogram, also known as a sleep study, measures brain and body activity during sleep. Sleep studies can help diagnose sleep disorders, including restless legs syndrome, periodic limb movement disorder, and insomnia, as well as breathing disorders such as sleep apnea. Polysomnograms are done over one or more nights at a sleep center.
During a polysomnogram:
- Electrodes are attached to the person’s scalp, eyelids, leg, and/or chin.
- Throughout the night and during the various wake/sleep cycles, the electrodes record brain waves, eye movement, breathing, leg and skeletal muscle activity, blood pressure, and heart rate.
- The person may be video recorded to note any movement during sleep.
- Polysomnograms are noninvasive and painless. The most common side effect is skin irritation caused by the adhesive used to attach sensors.
Ultrasound imaging
Ultrasound, also called ultrasonography, uses high-frequency sound waves to create images that show inside the body. It can assess changes in the anatomy of soft tissues, including muscle and nerve tissues. It is more effective than an X-ray in showing soft tissue changes, such as tears in ligaments or soft tissue masses. Ultrasounds can be done in a clinic or doctor’s office.
During an ultrasound:
- The person lies on a table or reclines in an examination chair.
- A jelly-like lubricant is applied to the bare skin and a transducer, which sends and receives high-frequency sound waves, is passed over the body.
- The sound wave echoes are recorded and displayed as a real-time visual image of the structure or tissue being examined.
- Ultrasound is painless, noninvasive, and carries little or no risk.
- The test takes 15-30 minutes to complete.
There are many types of ultrasounds relevant to neurological disorders. These include:
- Carotid Doppler ultrasound, which measures blood flow in arteries and blood vessels in the neck.
- Transcranial Doppler ultrasound, which shows blood flow in certain arteries and blood vessels inside the skull. Carotid dopplers and transcranial dopplers can help assess a person’s risk of stroke.
- Duplex ultrasound, which uses two types of ultrasound to see and hear the blood flow in the major arteries and veins in the arms and legs.
X-rays
X-rays of a person’s chest and skull may be taken as part of a neurological evaluation. X-rays can show any part of the body, such as a joint or major organ system. Tissue masses such as injured ligaments or a bulging disc are not visible on conventional X-rays. X-rays can be done in a doctor’s office or clinic and are fast and noninvasive.
In a conventional X-ray:
- A concentrated burst of low-dose ionized radiation passes through the body and onto a photographic plate.
- Since calcium in bones absorbs X-rays more easily than soft tissue or muscle, the bony structure appears white on the film.
- Vertebral misalignment or fractures can be seen within minutes.
Fluoroscopy
Fluoroscopy is a type of X-ray that uses a continuous or pulsed beam of low-dose radiation to produce continuous images of a body part in motion. The fluoroscope (X-ray tube) is focused on the area of interest and pictures are either recorded or sent to a monitor for viewing. Fluoroscopy evaluates swallowing and can be part of other procedures, such as a lumbar puncture, angiogram for clot removal, or myelogram.

Treating spinal cord injuries
At an accident scene, if SCI is suspected, emergency personnel will place a rigid collar around the neck and carefully place the person on a backboard to prevent further damage to the spinal cord. They may use sedatives to relax the person and prevent movement. Emergency responders may also insert a breathing tube if there are problems breathing and the body isn’t receiving enough oxygen from the lungs.
Doctors are now able to predict with reasonable accuracy the likely long-term outcome of an SCI. This helps people experiencing spinal cord injuries to set achievable goals for themselves and gives families and loved ones a realistic set of expectations for the future.
Immediate treatment at the trauma center or emergency room may include:
Treatment begins at the site of injury. Paramedics and emergency medical services staff are crucial in stabilizing and transferring the patient to an appropriate facility. Immobilization can help prevent complicating existing injuries. Life threats or concurrent traumatic injuries in severe trauma cases must be addressed immediately. Hypotension and shock can aggravate the SCI and reduce the likelihood of neurologic recovery. Immediate measures are necessary to stabilize cardiorespiratory function. Emergent surgical decompression, if warranted and feasible, may lessen the injury’s extent.[rx][rx] This procedure helps stabilize the spine, prevent pain, reduce deformity, and relieve compression from a herniated disc, blood clot, or foreign body.
- Realigning the spine using a rigid brace or mechanical force, which is usually done as soon as possible to stabilize the spine and prevent additional damage.
- Surgery to remove any fractured bones or other objects that are pressing on the spinal column. Spinal decompression surgery to relieve pressure within the spinal column may also be necessary in the days after injury. Results of neurosurgical studies show that, in some cases, earlier surgery is connected to better functional recovery.
An SCI may result in the following problems, which require treatment:
- Breathing problems. About one-third of people with an SCI will need temporary or permanent help with breathing and may require a breathing tube. Any injury to the spinal cord between the C1-C4 segments can stop breathing as the nerves in this region cause the diaphragm to move and the lungs to expand. People with an SCI may need special training with breathing and swallowing. Their caregivers may need training as well.
- Pneumonia. Breathing complications are the leading cause of death in people with an SCI, commonly as a result of pneumonia. People using a ventilator to help with breathing, are at increased risk of developing pneumonia. The person will need careful monitoring and antibiotic treatment if symptoms of pneumonia appear. Ways to prevent pneumonia include clearing the throat and taking precautions to avoid food and liquids being sucked into the lungs (aspiration).
- Circulatory (blood flow) problems. Changes in circulation can lead to unstable blood pressure, abnormal heart rhythms (arrhythmias), and blood clots that may appear days after injury. The injured person will need careful monitoring for each of these common issues after an SCI. People with spinal cord injuries are at increased risk for blood clots because blood flow can slow or stop in the large veins in the legs. Anticoagulant drugs and compression stockings to increase blood flow in the lower legs and feet can reduce the risk for blood clots.
- Stiffness and changes in muscle tone. Reflexes may become exaggerated over time, causing muscle stiffness and an increase in muscle tone (spasticity) that may require special treatment. Muscles below the injury site may weaken when people don’t use them.
- Autonomic dysreflexia. Autonomic dysreflexia is a life-threatening reflex action that primarily affects those with injuries to the neck or upper back. Symptoms may include flushing or sweating, a pounding headache, anxiety, sudden increase in blood pressure, vision changes, or goose bumps on the arms and legs. If possible, the person needs to stay in a sitting position to keep blood flowing to the legs and feet, which helps reduce blood pressure.
- Pressure sores (also known as pressure ulcers). Pressure sores are areas of skin that have broken down because of continuous pressure on the skin and reduced blood flow to the area. People with paraplegia and tetraplegia are at risk for pressure sores. To prevent pressure sores, they change their position regularly, either on their own or with the help of assistive devices or a caregiver.Maintaining a systolic blood pressure at or greater than 90 mm Hg and a mean arterial pressure around 85 mm Hg to 90 mm Hg has been recommended by the 2002 and 2013 American Association of Neurological Surgeons and Congress of Neurological Surgeons’ (AANS/CNS) guidelines. Thus, despite little evidence supporting the practice, a MAP greater than 85 mm Hg is currently targeted as part of SCI management. The most recent AANS/CNS recommendations advise maintaining MAP goals for a week.
- Pain. Some people with an SCI develop neurogenic pain—an intense burning or stinging sensation. This pain may be constant or may come and go. Many things can trigger it—and some people may even feel pain in parts of the body that have otherwise lost sensation. Treatments for chronic pain include medicines, spinal or brain electrical stimulation, and surgery. But none of these treatments are completely effective at relieving neurogenic pain long term.
- Bladder and bowel problems. People may need to use a catheter to empty their bladder and learn new ways to empty their bowels. The person may need to change their diet.
- Sexual function. Depending on the severity and location of the injury, and the person’s recovery after the injury, their sexual function and fertility may be affected. A urologist and other specialists can suggest different options to support sexual functioning and health.
- Depression. Many people living with an SCI may develop depression due to lifestyle changes after the injury. Therapy and medicine can help treat depression and other mental health conditions.
Medication
Steroid administration is still debatable in SCI treatment. Steroids were initially thought to enhance anti-inflammatory mechanisms, reduce secondary SCI, and increase cell viability. Initial studies suggested potential benefits from steroid administration, yet subsequent research has failed to substantiate any such advantage.
Indications for early intubation include higher SCI levels (above C5), total paralysis, low lung volumes on chest radiographs, and the presence of concomitant injuries, especially chest wall or intrathoracic lesions. Tracheostomy may be advantageous for patients who may require mechanical ventilation longer than 2 weeks following injury.[rx]
Patients with acute urinary retention should have a urinary or suprapubic catheter inserted to relieve lower tract discomfort caused by a full bladder. The urethral catheter, which should be 16 to 18 French in size, may be inserted as a first line of treatment. Clean intermittent catheterization results in fewer problems, a higher spontaneous voiding rate, and a lower incidence of urinary tract infections (UTIs). Patients can develop greater tolerance to clean intermittent catheterization if the nursing team focuses on thorough training and precise catheter placement. Additional outpatient support services may be useful. Patients typically welcome education.[rx]
The Neurocritical Care Society recommends starting deep vein thrombosis (DVT) prophylaxis as soon as possible and no later than 72 hours after the SCI. The Consortium of Spinal Cord Injury does not define a specific timing but proposes using low-molecular-weight heparin in the acute care period to avoid DVT. Daily bleeding risk assessment must be performed to avoid delays due to bleeding concerns. Enoxaparin is superior to unfractionated heparin in preventing pulmonary embolism in patients with SCIs.
Patients with SCIs are best managed in neurological intensive care units, where personnel are proficient in managing SCIs. Dedicated trauma units must be identified for smooth patient transfer and care transition. Patients have optimum outcomes with intense rehabilitation therapy under physiatrists, physical therapists, and occupational therapists’ guidance. Rehabilitation is continued on an outpatient basis after hospital discharge.
Trials involving the administration of nimodipine, gacyclidine, thyrotropin-releasing hormone, riluzole, gangliosides, minocycline, magnesium, and acidic fibroblast growth factor in patients with spinal cord injuries have not shown significant benefits, though further studies are ongoing.[rx][rx][rx] Presently, high-dose steroids remain the cornerstone of acute SCI treatment.
Stem Cell Therapy
Stem cell treatments for spinal cord injuries can be categorized into supportive and loading therapies. Supportive stem cell therapy utilizes nonneural stem cells like bone marrow, umbilical cord, and adipose tissue-derived mesenchymal stem cells (MSCs). These cells are administered intravenously or intrathecally due to limited migration to the target area and differentiation into neural cells. MSCs release neurotrophic factors that can repair the injured area, yet their ability to replenish the nervous system is constrained. Most clinical trials focus on this therapy due to easier MSC preparation and regulatory compliance.
In contrast, loading therapy employs stem cells capable of producing neural cells, such as olfactory ensheathing and neural progenitor and stem cells derived from embryonic stem cells. Engraftment of these cells has a greater likelihood of replacing lost nerve cells in terms of functionality, though the procedure requires invasive transplantation methods and complex cell preparation processes.[rx]
Chronic SCI Treatment
Chronic SCI management depends on the underlying etiology. The treatment should address the neurologic deficits and primary disorder. Complications such as pressure ulcers, secondary bacterial infection, and urinary dysfunction must also be addressed. Rehabilitation and supportive care are essential in optimizing quality of life and functional outcomes for people with chronic SCI, regardless of the underlying etiology. Combined modalities and seamless interprofessional collaboration are thus often necessary in treating chronic SCIs.

Spinal cord injury rehabilitation
Rehabilitation programs for people with an SCI combine physical therapies with skill-building activities. They also have counseling designed to provide social and emotional support and increase the person’s independence and quality of life.
A doctor specializing in physical medicine and rehabilitation usually leads the rehabilitation team. The team may include social workers, physical and occupational therapists, recreational therapists, rehabilitation nurses, rehabilitation psychologists, vocational counselors, nutritionists, a case worker, and other specialists.
The first phase of rehabilitation after injury usually focuses on regaining communication skills and leg and arm strength. Adaptive or assistive devices may help people with an SCI to regain independence and improve mobility and quality of life. They can also help with communication skills, such as writing, typing, and using the telephone.
Depending on how serious the injury is, the person may need:
- Braces
- A wheelchair
- Electronic stimulators
- Assisted training with walking
- Neural prosthetics (assistive devices that may stimulate the nerves to restore lost functions)
- Computer adaptations and other computer-assisted technology
Rehabilitation for an SCI can include:
- Physical therapy, which are exercise programs that strengthen muscles.
- Occupational therapy, which helps redevelop fine motor skills. People with an SCI may need help regaining skills to perform activities for daily living—such as getting in and out of a bed, personal hygiene, eating, and using the toilet. The person may learn how to cope with spasticity, autonomic dysreflexia, and neurogenic pain as part of their occupational therapy.
- Vocational rehabilitation, which is identifying basic work skills and physical and cognitive capabilities that can support paid work. Through this process, the person and their team can identify potential, accessible workplaces and any assistive equipment they will need..
- Educational training, which can help the person develop skills for a new line of work that may be less dependent upon a person’s physical abilities. People with an SCI are encouraged to participate in activities that provide a sense of satisfaction and self-esteem, such as educational classes, hobbies, special interest groups, and family and community events.
- Recreation therapy, which encourages people with an SCI to participate in sports, arts, or other leisure activities that they can do with their new level of mobility. This can help people achieve a balanced lifestyle that provides opportunities for socialization and self-expression.
- Modern wheelchairs. Improved, lighter weight wheelchairs are making people with spinal cord injuries more mobile and more comfortable. Some people need an electric wheelchair. Some wheelchairs can even climb stairs, travel over rough ground and elevate a user to reach high places without help.
- Computer adaptations. Computers can be hard to use if you have limited hand function. Computer adaptations range from simple to complex, such as key guards and voice recognition.
- Electronic aids to daily living. Any device that uses electricity can be controlled with an electronic aid to daily living. Devices can be turned on or off by switch or voice-controlled and computer-based remotes.
- Electrical stimulation devices. Often called functional electrical stimulation systems, these devices use electrical stimulators. The stimulators help control arm and leg muscles to allow people with spinal cord injuries to stand, walk, reach and grip.
Acute recovery
The rehabilitation process following a spinal cord injury typically begins in the acute care setting. Occupational therapy plays an important role in the management of SCI.[rx] Recent studies emphasize the importance of early occupational therapy, started immediately after the client is stable. This process includes teaching of coping skills, and physical therapy.[rx] Physical therapists, occupational therapists, social workers, psychologists and other health care professionals typically work as a team under the coordination of a physiatrist to decide on goals with the patient and develop a plan of discharge that is appropriate for the patient’s condition. In the first step, the focus is on support and prevention. Interventions aim to give the individual a sense of control over a situation in which the patient likely feels little independence.[rx]
As the patient becomes more stable, they may move to a rehabilitation facility or remain in the acute care setting. The patient begins to take more of an active role in their rehabilitation at this stage and works with the team to develop reasonable functional goals.[rx]
Respiration
In the acute phase physical and occupational therapists focus on the patient’s respiratory status, prevention of indirect complications (such as pressure sores), maintaining range of motion, and keeping available musculature active.[rx]
Depending on the Neurological Level of Impairment (NLI), the muscles responsible for expanding the thorax, which facilitate inhalation, may be affected. If the NLI is such that it affects some of the ventilatory muscles, more emphasis will then be placed on the muscles with intact function. For example, the intercostal muscles receive their innervation from T1–T11, and if any are damaged, more emphasis will need to be placed on the unaffected muscles which are innervated from higher levels of the CNS. As SCI patients have reduced total lung capacity and tidal volume[rx] it is pertinent that physical therapists teach SCI patients accessory breathing techniques (e.g. apical breathing, glossopharyngeal breathing, etc.) that typically are not taught to healthy individuals.
Functional electrical stimulation
Physical therapists can assist immobilized patients with effective cough techniques, secretion clearance, stretching of the thoracic wall, and suggest abdominal support belts when necessary. The amount of time a patient is immobilized may depend on the level of the spinal cord injury. Physical therapists work with the patient to prevent any complications that may arise due to this immobilization. Other complications that arise from immobilization include muscle atrophy and osteoporosis, especially to the lower limbs, increasing the risk of fractures to the femur and tibia.[rx] While passive weight bearing of paralyzed lower extremities appears to be ineffective, stressing the bones through muscular contractions initiated by functional electrical stimulation (FES) has yielded positive results in some cases.[rx] The intensity, frequency, and duration of stress to the bones appear to be important determinants of improved bone parameters.[rx] Generally, the frequency is effective with three or more weekly exercise sessions. Studies of duration suggest that several months to one or more years of FES are necessary.[rx]
Improving locomotor function
Improvement of locomotor function is one of the primary goals for people with a spinal cord injury. SCI treatments may focus on specific goals such as to restore walking or locomotion to an optimal level for the individual. The most effective way to restore locomotion is by complete repair, but techniques are not yet developed for regeneration. Treadmill training, over groundtraining, and functional electrical stimulation can all be used to improve walking or locomotor activity. These activities work if neurons of the central pattern generator (CPG) circuits,[rx][rx] which generate rhythmic movements of the body, are still functioning. With inactivity, the neurons of CPG degenerate. Therefore, the above activities are important for keeping neurons active until regeneration activities are developed.[rx] A 2012 systematic review found insufficient evidence to conclude which locomotor training strategy improves walking function most for people with spinal cord injury.[rx] This suggests that it is not the type of training used, but the goals and the routines that have the biggest impact.[rx] Applying spinal cord stimulation (transcutaneous or epidurally) during weight supported walking have been shown to improve locomotor output.[rx]
Provision
In the English NHS a serious shortage of specialist beds was identified by a review in December 2016. There were 393 and 54 additional beds were required. Patients waited an average of 52 days for a bed on a specialist ward in 2015–16. This meant patients were “inappropriately” occupying beds at major trauma centres. It was suggested that NHS England‘s specialised commissioning division would be unable to fund the recommendations. According to the Spinal Injuries Association, of 2,494 referrals in 2017–18 to specialist spinal cord injury centres, only 800 were admitted and many more patients were not referred at all.[rx]
Regenerative Medicine
New consortium to restore lost function—Researchers are pursuing new methods to repair damage to the spinal cord and restore function after SCI. In 2010, VA and several academic partners established a consortium, now named the Gordon Mansfield SCI Consortium, to pursue high-risk, high-return ideas that might otherwise be unlikely candidates for funding.
The consortium hopes to advance the field of regenerative rehabilitation. Scientists in the consortium have already generated promising early findings highlighting cell transplantation as a potential way to repair the nervous system. They have demonstrated in animal models that cell transplants can survive and integrate with a chronically injured spinal cord and form connections with host tissue.
Cellular therapies to restore spinal cord function include stem cell transplantation, tissue engineering, the use of biomaterials, and genetically manipulated cells to repair damaged or diseased tissues. Researchers are using tissue engineering to manufacture temporary scaffolds (a framework or structural element used to hold cells together) that contribute to the formation of new functional tissue.
Transplanting neural cells in the spinal cord—In 2019, researchers from the VA San Diego Healthcare System and the University of California San Diego found that neural stem cells (immature stem cells in the brain that can become more specialized) act like the cells of normal spinal cords when they are grafted into the locations of spinal cord injuries in rats.
As the stem cells develop, they spontaneously segregate themselves into cell clusters, some supporting movement and others supporting feeling. In addition, they reproduce into a variety of cells found in normal spinal cords and find appropriate places to locate within the graft. The study demonstrates that it may be possible to use stem cells to form a “bridge” around an injury to restore both movement and feeling in people with SCIs.
3D printed spinal cord—Another 2019 study from the VA San Diego Healthcare System and the University of California San Diego describes how researchers used rapid 3D-printing technologies to create a spinal cord facsimile. The team loaded the scaffold with neural stem cells and successfully implanted it into sites of severe SCI in rats.
The 3D-printed scaffolds reproduce the slender, bundled arrays of axons (a portion of the nerve cell that conducts electrical impulses) in the spinal cord, helping stem cells to replicate the anatomy of the spinal cord before it was injured. The scaffolding keeps axons in order, guiding them to grow in the right direction to complete a spinal cord connection.
The use of 3D printing allows clinicians to quickly print out an implant that will match the injured site of a host spinal cord, regardless of its size and shape. Rats treated in this way regained significant function in their hind legs after a few months—and new spinal cord tissue grew across the injury and connected the severed ends of the host spinal cord.
Helping nerve fibers regenerate—Boosting energy levels within damaged nerve fibers (axons) may help them regenerate and aid in the recovery of function, according to a 2020 study by a team of researchers from the Richard L. Roudebush VA Medical Center in Indianapolis and Indiana University. Cells produce energy through the action of tiny power plants called mitochondria, which convert nutrients and oxygen into fuel.
In mouse models, injured axons do not regenerate because of energy deficits and mitochondrial dysfunction. The team found that increasing function and energy metabolism within the mitochondria is key to enabling axons to regenerate and improve recovery of function after SCI.
In three mouse model experiments, the team stimulated mitochondria by deleting a protein anchor called syntaphilin and increased energy metabolism through creatine treatment. This strategy, the team believes, can be translated into future SCI treatments.
Bioengineered spinal discs—In 2018, researchers at the Corporal Michael J. Crescenz VA Medical Center in Philadelphia and the University of Pennsylvania successfully implanted bioengineered spinal discs into goats.
The treatment combined an animal’s stem cells with biomaterial to generate a composite structure that was implanted into its spine to act as a replacement spinal disc. Goats were chosen because their cervical spinal disc dimensions are similar to humans and they have a semi-upright stature. Researchers found the implanted discs’ mechanical properties either matched or exceeded those of native goat cervical discs, eight weeks after the procedure.
The success of the study offers “compelling” evidence that tissue-engineered analogs might soon be used to replace a deteriorated spinal disc in humans. The team is optimistic they can achieve the same level of success in human trials.
Bone Mass Density
Denosumab is a monoclonal antibody drug that is used to treat osteoporosis, bone loss, and problems related to bone cancer. Researchers at the James J. Peters VA Medical Center in New York found it can be used to preserve bone density in patients with SCIs, according to a 2020 study.
Patients with SCIs are at high risk of osteoporosis and bone fractures because of sluggish blood flow, hormonal alterations, and other factors. Without strong bones to support the body, patients can have difficulties using exoskeletal devices or spinal cord stimulation to help them walk, which could result in fractures.
The research team found SCI patients who received denosumab maintained higher bone mineral density at the knee 18 months after treatment than those who received a placebo.
Acute Intermittent Hypoxia
Brief exposures to hypoxic air (air that contains reduced oxygen levels), interspersed with periods of breathing room air, can improve motor function in people with SCI, found a 2020 article by researchers at the Edward Hines Jr. VA Hospital in Illinois and the University of Miami.
The team found that acute intermittent hypoxia (AIH) paired with transcranial magnetic stimulation increased electrical activity in muscles within the hand, leading to improved motor output in patients with intact spinal cords. The researchers concluded the treatment’s ability to induce temporary changes in neuron excitability can help patients with SCI recover lost motor function. The group is continuing its efforts to understand how AIH supports human motor systems.
Electronic Stimulation Devices
Implanted neuroprosthetic devices—In 2018, researchers at VA’s Advanced Platform Technology (APT) Center and Case Western Reserve University published the results of a 10-year clinical trial to test a surgically implanted electrical stimulation system in people with SCI. During the surgery, electrodes were implanted in muscles located in the subjects’ trunk and legs. Electrical leads were then connected to a neurostimulator. The team found that implanted lower-limb neuroprostheses can provide lasting benefits for recipients.
By stimulating muscles, neuroprostheses promote improved standing, balance, and the capability for exercise. Patients are given functional training on how to use the stimulation system and are prescribed a course of exercise. Lab tests focus on strength, balance, and function with and without the system.
In 2019, researchers at the Cleveland FES Center announced they had developed a method to activate abdominal and lower rib cage muscles to produce an effective cough, using minimally invasive techniques. Electrodes were inserted under the skin and then advanced to the dorsal spinal cord. Research participants used a stimulator to produce several different cough efforts ranging from light to strong. It is the first method in the world that can restore cough to SCI patients.
Preventing falls from wheelchairs—To improve wheelchair safety, researchers with the APT Center developed an algorithm to detect sudden stops during wheelchair use. Sudden stops can often cause falls from the wheelchair, especially for users who are paralyzed. The team paired the algorithm with a neurostimulation device that increases trunk stability, reducing the likelihood that the user will be dislodged from the wheelchair during a sudden stop.
Researchers tested the system on three volunteers with SCI, who reported feeling safer. The study, published in 2020, suggests that neurostimulation systems can improve wheelchair safety for paralyzed users.
Electronic stimulation safety—APT Center researchers showed, in a 2020 study, that nerve health is maintained after implanting an electrode stimulation device in a patient with SCI. A patient with leg paralysis was given an implanted electrode device to stimulate his leg muscles and help him to stand.
The researchers examined physiologic changes to the patient’s nerves pre-surgery, post-surgery, and at one-year follow up. They found minimal nerve irritation during surgery that resolved after the procedure. Diagnostic testing found preserved nerve health with strengthened responses following stimulated exercise, demonstrating that implanted electrodes to restore function after SCI can be both safe and effective.
Transcranial direct current stimulation—In a pilot study published in 2018, a team of researchers from the APT Center and the Cleveland Clinic found that transcranial direct current stimulation (tDCS) holds promise to restore function in SCI patients.
The team investigated the combined effects of tDCS and rehabilitation on Veterans with long-term, incomplete SCI that affected upper-limb function. In tDCS, electrical currents are applied directly to the brain. The technique is similar to transcranial magnetic stimulation (TMS), a non-invasive procedure used to treat major depressive disorder and other conditions.
Study participants who received tDCS and rehabilitation for two weeks had increased muscle strength in their hand, wrist, and proximal arm muscles that lasted for three months, compared to a group that received a sham treatment.
Testosterone Release Therapy
Low-dose testosterone replacement therapy paired with resistance training can lead to improved muscle mass and health in SCI patients, according to a 2019 study by researchers at the Hunter Holmes McGuire VA Medical Center in Richmond, Virginia.
Patients who took part in the study underwent twice-weekly resistance training paired with electrical stimulation for 16 weeks, to activate paralyzed muscles in their legs. They were also given testosterone replacement therapy through a patch. Patients who received both testosterone and resistance training had improved body lean mass, muscle mass, and knee extensor strength. They also had, overall, less body fat, an increased metabolic rate, better ability to process glucose, and a stronger inflammatory response.
The researchers concluded that low-dose testosterone replacement therapy can ease the negative muscle and metabolic effects of SCI.
Pressure Injury Treatment
Smart bandage technology—Researchers at the APT Center have developed a “smart bandage” that makes use of electrical stimulation to treat chronic wounds that will not heal on their own. Chronic pressure injuries frequently occur in people with SCI. The layered smart bandage includes an absorbent material to protect the wound, a mechanism to deliver electrical stimulation, temperature sensors, and a smart chip.
Electrical stimulation provides energy to promote healing in a chronic wound. The temperature sensor helps clinicians monitor wound healing without having to remove the bandage. The bandage can last for up to seven days. If needed, a new bandage can be affixed to the existing electronics for another seven days, or for as long as the patient requires.
Pressure injuries can be expensive to manage, both for the individual and the health care system. The new bandage could change that dynamic, making it possible for clinicians to remotely monitor wound healing from the patient’s home, reducing clinic visits. The research team is working with VA’s Technology Transfer Program and outside entrepreneurs to bring the invention to market.
New pressure injury measurement tool—An innovative computer-based system to more accurately measure pressure injuries is being tested by researchers at the James A. Haley Veterans Hospital in Tampa, Florida.
The system captures 3D-images with a camera mounted to a tablet. An algorithm uses the color, geometry, and formation of the wound to assess its length, width, and depth. The research team believes the new tool is more reliable than the current pressure ulcer monitoring tool.
Accurate pressure injury measurement is vital to allow clinicians to accurately assess the severity of the wound and the degree of tissue damage, and to determine whether current treatment strategies are effective. Intervening early to prevent injuries from worsening is critical for improving patient outcomes and reducing costs. Following the completion of a preliminary trial in 2018, the team hopes to assess the effectiveness of the new system compared with manual pressure injury measurements.
Brain-Computer Interfaces
BrainGate—VA has played a major role in supporting the establishment of BrainGate, a collaborative research enterprise that seeks to develop new neurotechnologies. Researchers at the Providence VA Medical Center in Rhode Island, Brown University, and other institutions spearheaded the development of brain-computer interfaces that rely on microelectrodes implanted in the brain. The electrodes send signals to an external decoder that translates them into commands for robotic devices, helping users to restore lost function and control over their environment.
Among other projects, the BrainGate team is now studying whether the system can be effective as a means of intuitive control of prosthetic limbs or as a way to help patients move their own paralyzed limbs.
A 2011 study found the BrainGate system continued to control a computer cursor accurately through brain activity for more than 1,000 days after it was initially implanted. In 2012, in a widely publicized study, the team showed that people with tetraplegia (paralysis that affects the upper and lower body) could use the system successfully to control a robotic arm to reach and grasp for items.
ReHAB—The FES Center and the consortium are currently working on a system called ReHAB (Reconnecting the Hand and Arm to the Brain). The system uses an array of sensors surgically implanted into different areas of the brain along with electrodes placed directly on nerves in the hand, arm, and shoulder. The device detects paralyzed users’ thoughts and then stimulates nerves in the upper limbs to initiate movement. An early feasibility study of this system is scheduled to be completed in 2024.
Restoring lost nervous system function—The VA Center for Neurorestoration and Neurotechnology (CfNN), located in Providence, Rhode Island, aims to advance and translate neurotechnology to restore lost function. Through multiple areas of focus, CfNN seeks to develop, test, and implement new therapies and technologies that restore function for Veterans with disorders affecting the nervous system.
In 2018, a team that included researchers from the CfNN showed that “local field potentials”— the total electrical current flowing to a small section of nervous tissue in the brain—may be a more robust, stable signal for brain-computer systems than neuronal action potentials, which represent the activity of individual brain cells.
Chronic Pain in SCI
The VA Rehabilitation Research and Development Center for the Restoration of Nervous System Function (CRNF) in West Haven, Connecticut, is dedicated to making clinical, molecular and cell-based discoveries to alleviate pain and restore nervous system function in Veterans whose nerves have been damaged by injury or illness such as SCI, multiple sclerosis, and diabetes.
Studies at the CRNF center focus on the role of sodium channels in mediating chronic neuropathic pain in various diseases. Sodium channels are proteins that conduct sodium ions through a cell’s plasma membrane. By transmitting impulses quickly throughout cells and cell networks, sodium channels enable coordination of higher processes ranging from movement to cognition.
In 2019, a group of researchers from the CRNF and other institutions identified a mutation in α-subunits of voltage-gated sodium channels that is responsible for chronic neuropathic pain in diabetes patients.
ReWalk Exoskeleton
VA’s Center on the Medical Consequences of Spinal Cord Injury is located at the James J. Peters VA Medical Center in New York. The center’s mission is to improve Veterans’ quality of life and increase their lifespan by preventing consequences from an SCI. These secondary injuries can include bone and muscle loss, as well as metabolic and cardiovascular changes.
Researchers at the center continue to study an Israeli technology that allows paraplegics to stand, walk, and climb stairs, called ReWalk. ReWalk is a wearable robotic exoskeleton that provides powered hip and knee motion to enable individuals with SCI to stand upright, walk, and turn. On their first day using the device, most people can stand and take a few steps, although it takes practice and training to use it properly. The FDA approved the ReWalk exoskeleton for sale in the United States in 2014, and VA now purchases the apparatus for eligible Veterans with SCIs.
VA is currently conducting a four-year clinical trial to evaluate the impact of exoskeleton use in home or daily life settings. The 160-person trial is scheduled to be completed in 2021.
Assistive Technology
The Human Research Engineering Laboratories (HERL), operated jointly by the VA Pittsburgh Healthcare System and the University of Pittsburgh, aims to improve mobility and function in people with disabilities through advanced engineering.
HERL is responsible for multiple innovations in wheelchair design and other assistive technologies that have changed the way hundreds of thousands of Veterans interact with their environment and approach daily living.
The team has 25 patents in wheelchair design and technology to its credit. Examples of their cutting-edge innovations include a waterproof wheelchair that runs on compressed air; a robotic wheelchair called MEBot; a powered wheelchair fitted with robotic arms to help users with limited hand function; and a SmartWheel device that evaluates manual wheelchair use by measuring push forces, smoothness, and speed.
In 2020, researchers from HERL and the University of Pittsburgh published findings on new designs for an adjustable wheelchair that allows users to participate in para-table tennis events. The team found that specific support, movements, and posture needed to competitively participate in table tennis are different than general day-to-day mobility requirements.
Complications
A spinal cord injury can lead to many complications. Your rehabilitation team helps you develop tools to address these complications. The team also recommends equipment and resources to promote your quality of life and independence. Areas often affected include:
- Bladder control. The bladder continues to store urine from the kidneys after a spinal cord injury. But the injury may interfere with the brain receiving the messages it needs to control the bladder.Changes in bladder control increase the risk of urinary tract infections. The changes also may cause kidney infections and kidney or bladder stones. During rehabilitation, you learn ways to help empty your bladder.
- Bowel control. The stomach and intestines work much like they did before the injury, but control of bowel movements is often altered. A high-fiber diet might help regulate the bowels. You also can learn ways to help control your bowel.
- Pressure injuries. Below the neurological level of your injury, you might have lost some or all skin sensations. Therefore, your skin can’t send a message to your brain when it’s injured by certain things such as prolonged pressure. This can increase the risk of getting pressure sores. Changing positions often — with help, if needed — can help prevent the sores. Proper skin care also can help prevent pressure sores.
- Circulatory control. People with a spinal cord injury may have low blood pressure when they rise, known as orthostatic hypotension. They also may have swelling in the arms and legs. This can increase the risk of developing blood clots, such as deep vein thrombosis or a pulmonary embolus.Another issue with circulatory control is a potentially life-threatening rise in blood pressure, known as autonomic dysreflexia. Your rehabilitation team can teach you how to address these issues if they affect you.
- Respiratory system. If the injury affects the stomach and chest muscles, it may be hard to breathe and cough.The neurological level of injury determines what kind of breathing problems you may have. If the injury affects your neck and chest, you might have an increased risk of pneumonia or other lung conditions. Medicines and therapy can be helpful for treatment and prevention.
- Bone density. A spinal cord injury increases the risk of osteoporosis and fractures below the level of injury.
- Muscle tone. Some people with spinal cord injuries have a tightening or motion in the muscles, known as spasticity. Other people may have soft and limp muscles lacking muscle tone, known as flaccidity.
- Fitness and wellness. Weight loss and muscle thinning are common soon after a spinal cord injury. Because limited mobility can lead to a more sedentary lifestyle, there is a risk of weight gain, cardiovascular disease and diabetes.A dietitian can help you eat a nutritious diet to sustain a healthy weight. Physical and occupational therapists can help you develop a fitness and exercise program.
- Sexual health. A spinal cord injury may lead to changes in erection and ejaculation, or in changes in lubrication. Healthcare professionals specializing in urology or fertility can offer options for sexual functioning and fertility.
- Pain. Some people have pain, such as muscle or joint pain, from overuse of particular muscle groups. Nerve pain can occur after a spinal cord injury, especially in someone with an incomplete injury.
- Depression. Pain and the changes a spinal cord injury brings can cause depression in some people.
Prevention
Following this advice might reduce your risk of a spinal cord injury:
- Drive safely. Car crashes are one of the most common causes of spinal cord injuries. Wear a seat belt every time you are in a moving vehicle. Make sure that your children wear a seat belt or use an age- and weight-appropriate child safety seat. To protect them from air bag injuries, children under age 12 should always ride in the back seat.
- Check water depth before diving. Don’t dive into a pool unless it’s at least 9 feet (about 2.74 meters) deep and clearly marked safe for diving. Competition diving requires a deeper depth. And don’t dive into an aboveground pool or into water if you don’t know how deep it is.
- Prevent falls. Use a step stool with a grab bar to reach high-up objects. Add handrails along stairways. Put nonslip mats on tile floors and in the tub or shower. For young children, use safety gates to block stairs and consider installing window guards.
- Take precautions when playing sports. Always wear recommended safety gear. Avoid leading with your head in sports. For example, don’t slide headfirst in baseball. In American football, don’t tackle using the top of your helmet. Use a spotter for new moves in gymnastics.
- Don’t drink and drive. Don’t drive after drinking alcohol or while under the influence of drugs. Don’t ride with a driver who has been drinking.
Secondary Conditions Due to Spinal Cord Injury
Besides a loss of sensation or motor function, injury to the spinal cord leads to other changes in the body. Your body is still working below the level of injury. It is just that messages to and from your brain are not being communicated through the site of injury. You will have to provide your body with the necessary care manually. Complications of spinal cord injury are possibly preventable with good healthcare, diet and physical activity although sometimes they occur even with the best of intentions. The chart below indicates the secondary complications of spinal cord injury and ideas about how to combat them.
| Body System | Secondary Complication | Paralysis Effects | Suggestions for Treatment |
|---|---|---|---|
| Musculoskeletal | Calcium loss | Calcium loss from lack of movement through long bones of the legs, fractures | Keep track of bone density though regular bone density testing and treat as recommended by your healthcare professional.
Use of a standing frame (with gliders if able to use) to put movement through the legs. |
| Heterotrophic Ossification (H.O.) | Overgrowth of bone into soft tissue (muscle) | Perform range of motion exercise to joint to keep them pliable.
Medication: etidronate disodium (Didronel) to reduce bone growth. Surgical removal. |
|
| Loss of muscle tissue | Replacement of muscle with fat, stomach pouch, scoliosis, skin breakdown | Exercise as able. Move all body joints several times a day. Use resistance bands if possible
Some drugs can decrease muscle tone but have significant side effects, discuss with healthcare professional when appropriate. |
|
| Upper extremity pain | Shoulder pain from propelling wheelchair, rotator cuff injury, bursitis, capsulitis | Work with therapist to learn techniques for strengthening.
Don’t reach back so far to propel manual wheelchair. Add power assist to your wheels |
|
| Poor muscle tone | Scoliosis or curvature of the back | Strengthening exercises for the back.
Sit up, use excellent posture. Utilize positioning equipment when sitting or lying. Monitor equipment for wear and damage. |
|
| Tone (spasticity) | Spasms of muscles of the extremities and inside the body in individuals with cervical and thoracic injuries. Can be painful or prevent correct positioning of body. | Move and stretch muscles frequently during the day. Fatiguing the muscle can reduce tone.
Use medication as needed to reduce tone and pain, if necessary. Some tone can be effective for assisting with transfers. Use advanced therapies to exercise muscles to reduce tone. |
|
| Flaccidity | Lack of muscle tone in the lower extremities and the body in lumbar and sacral injuries. | Provide manual movement to the lower extremities to keep muscles pliable. | |
| Nervous | Slowing rate of information processing | Complicated by injury to the brain | Exercise your brain as well as your body. Examples: play word and math games, expand hobbies or new interests.
Engage in conversation and socialization. |
| Decreased balance and coordination | Spasticity | Stretching for all parts of your body on a regular basis. | |
| Muscular pain and Neuropathic pain | Nerve pain from inefficient nerve transmissions | Discuss option with your healthcare specialists for non-narcotic treatment options.
Exercise and stretch muscles which fatigues them making spasms less frequent and less severe. |
|
| Depression | Due to chronic illness/disability | Discuss your mental health with a professional for a checkup and/or treatment.
Become active in the SCI community to exchange ideas and opportunities. |
|
| Cardiovascular | Autonomic Dysreflexia (A.D.) | Misinterpretation of nerve impulses | Know the warning signs and treatments. https://www.christopherreeve.org/living-with-paralysis/free-resources-and-downloads/wallet-cards |
| Orthostatic hypotension-low blood pressure, fainting | Poor return of blood through the veins | Keep up with drinking fluids.
Use elastic blood return flow garments especially full leg and abdomen. |
|
| Deep Vein Thrombosis (DVT)
Pulmonary Embolis (PE) |
Pressure on blood vessels from external forces
Poor circulation |
Don’t cross your legs or ‘hook’ your arm.
Wear prevention elastic stocking on legs or arms. Use blood thinning medication, only if prescribed. |
|
| Edema | Poor return of fluid from the legs and arms | Elevate affected body part higher than the heart.
Use elastic blood return flow garments. Diuretic medication if indicated. |
|
| Exercise intolerance | Ineffective distribution of oxygen in the blood | If unable to perform the exercise routine that you did earlier, modify but stick with a plan. | |
| Increased cardiac risk | Develops over time. | Control factors such as diet, exercise, weight gain, cholesterol, blood pressure | |
| Respiratory | Decreased lung capacity | Restriction of breathing, poor posture | Breathe in deeply and exhale completely at regular intervals throughout the day.
Cough. Strengthen chest muscles with therapy. |
| Pneumonia | Infection in the lungs | Deep breath and cough to keep passages clear.
Keep mouth clean to avoid aspiration of food particles. Suction as needed. Antibiotics for infection. |
|
| Mechanical Ventilation | In individuals with injury above C3 | Use mechanical ventilation as required.
Strengthen muscles through respiratory therapy. Suction as needed or opt for an insufflator. |
|
| Gastric | Slower bowel absorption, Neurogenic bowel | Slowing bowel leading to constipation, enlarged colon, hemorrhoids, colorectal cancer | Increase roughage in your diet through food or bulk formers.
Use stool softener as needed. Very slowly, increase fluid. Generous use of lubricant during bowel program. With spastic bowel (cervical and thoracic injuries) performs digital stimulation slowly to relax sphincter. |
| Changes in ability to control cholesterol | Low HDL-good cholesterol | Use medication as prescribed.
Exercise either actively or passively. |
|
| Urinary | Kidney stones | Less ability to filter urine | Know your body so you can report a change to recognize there might be a problem, so this diagnosis can be made without delay. |
| Neurogenic Bladder | Failure to empty bladder at the appropriate time | Management with intermittent bladder catheterization, external catheter for men, indwelling catheter, suprapubic catheter, Mitrofanoff procedure or a combination of methods depending on individual needs. | |
| Urinary Tract Infection (UTI) | Bacteria in urine | Maintain hydration.
Remove soap residual or sanitizer after catheterization. Liberal use of lubricant. Maintain hygiene of bladder opening and hands. Antibiotics as needed. |
|
| Endocrine | Low testosterone | Reduction in hormones | Discuss treatment options with your healthcare provider to see if you want treatment for this condition. |
| Higher incidence of Type II Diabetes | Decreased metabolism of insulin | Perform exercises as you are able either actively or passively.
Medication as necessary. |
|
| Immune | Slowing of the immune system reactions | Increased chance of infection | Wash your hands frequently.
Use strict cleanliness with catheterizations. Avoid individuals with respiratory infections. |
| Septicemia | A massive infection that affects key body organs. | Follow up with treatment for any infection to avoid spreading.
Know the signs and symptoms for sepsis medical emergency: https://www.christopherreeve.org/living-with-paralysis/free-resources-and-downloads/wallet-cards |
|
| Skin | Increase in skin breakdown or pressure injury | Decreased elasticity, pressure from bones, lack of movement | Perform pressure releases.
Skin checks. Know what your skin looks like. |
| Groin rash | From moisture in damp, closed areas. | Frequent hygiene.
Air groin area daily. Apply rash protection when needed. |
|
| Nail care | Fragile nails or nail fungus | Maintain hygiene.
Trim nails carefully to avoid cuts. Allow air to circulate to toes with natural fiber socks and shoes. |
|
| Dry skin and callouses | Immobility | Gently and slowly remove skin with dry washcloth for friction.
Apply lanolin moisturizer. Maintain hydration. |
|
| Digestive | Lower calorie needs | Obesity, stomach pouch | Follow a nutritious but portion-controlled diet. |
| Feeling full all the time | Slowing moving bowel | Increase fiber
Eat small portions but at closer intervals. |
|
| Reproductive | Sexual dysfunction | Erectile dysfunction in males, lubrication dysfunction in females | Males have options of erectile dysfunction medication, penile injections and implants.
Some females respond with Viagra. Both might need to alter sexual function with different positions and strategies. |
Disclaimer: Each person’s journey is unique, treatment plan, life style, food habit, hormonal condition, immune system, chronic disease condition, geological location, weather and previous medical history is also unique. So always seek the best advice from a qualified medical professional or health care provider before trying any treatments to ensure to find out the best plan for you. This guide is for general information and educational purposes only. Regular check-ups and awareness can help to manage and prevent complications associated with these diseases conditions. If you or someone are suffering from this disease condition bookmark this website or share with someone who might find it useful! Boost your knowledge and stay ahead in your health journey. We always try to ensure that the content is regularly updated to reflect the latest medical research and treatment options. Thank you for giving your valuable time to read the article.
The article is written by Team Rxharun and reviewed by the Rx Editorial Board Members
Last Updated: May 02, 2025.







