The immune system is complex and is divided in two categories: i) the innate or nonspecific immunity, which consists of the activation and participation of preexistent mechanisms including the natural barriers (skin and mucosa) and secretions; and ii) the adaptive or specific immunity, which is targeted against a previously recognized specific microorganism or antigen. Thus, when a given pathogen is new to the host, it is initially recognized by the innate immune system and then the adaptive immune response is activated (2). Innate immunity is the host’s first line of defense and is intended to prevent infection and attack the invading pathogens.This nonspecific mechanism is fast (minutes to hours) while the adaptive response takes longer (days to weeks).
The Immune response is the body’s ability to stay safe by affording protection against harmful agents and involves lines of defense against most microbes as well as specialized and highly specific response to a particular offender. This immune response classifies as either innate which is non-specific and adaptive acquired which is highly specific. The innate response, often our first line of defense against anything foreign, defends the body against a pathogen in a similar fashion at all times. These natural mechanisms include the skin barrier, saliva, tears, various cytokines, complement proteins, lysozyme, bacterial flora, and numerous cells including neutrophils, basophils, eosinophils, monocytes, macrophages, reticuloendothelial system, natural killer cells (NK cells), epithelial cells, endothelial cells, red blood cells, and platelets.
The adaptive acquired immune response will utilize the ability of specific lymphocytes and their products (immunoglobulins, and cytokines) to generate a response against the invading microbes and its typical features are[1][2][3]:
-
Specificity: as the triggering mechanism is a particular pathogen, immunogen or antigen.
-
Heterogeneity: signifies the production of millions of different effectors of the immune response (antibodies) against millions of intruders.
-
Memory: The immune system has the ability not only to recognize the pathogen on its second contact but to generate a faster and stronger response.
The inflammatory immune response is an example of innate immunity as it blocks the entry of invading pathogens through the skin, respiratory or gastrointestinal tract. If pathogens can breach the epithelial surfaces, they encounter macrophages in the subepithelial tissues that will not only attempt to engulf them but also produce cytokines to amplify the inflammatory response.
Active immunity results from the immune system’s response to an antigen and therefore is acquired. Immunity resulting from the transfer of immune cells or antibodies from an immunized individual is passive immunity.
The immune system has evolved for the maintenance of homeostasis, as it can discriminate between foreign antigens and self; however, when this specificity is affected an autoimmune reaction or disease develops.
Issues of Concern
While the immune system is meant to protect the individual against threats, at times an exaggerated immune response generates a reaction against self-antigens leading to autoimmunity. Also, the immune system is not able to defend against all threats at all times.
-
Transplantation rejections are immune-mediated responses, represent a hindrance to transplantation
-
The etiology of many autoimmune disorders is obscure – the reality is that the prevalence of these disorders increases and manifests more aggressively
-
Type-I hypersensitivity disorders are immune-mediated and include allergic bronchial asthma, food allergy, and anaphylactic shock
-
Immunodeficiency disorders are rare, but they affect some children
Vaccination is required to induce an adequate active immune response to specific pathogens:
-
Live attenuated vaccines: Induce both humoral and cellular response. Contraindicated in pregnancy and immunocompromised states. Examples include adenovirus, Polio (Sabin), Varicella, Smallpox, BCG, Yellow fever, Influenza (intranasal), MMR, Rotavirus, etc
-
Killed or inactivated vaccines: Induce only humoral response. Examples include rabies, influenza (injection), Polio (Salk), Hepatitis A, etc
-
Subunit vaccines: Examples include HBV, HPV (types 6,11,16 and 18), acellular pertussis, Neisseria meningitides, Streptococcus pneumoniae, Hemophilus influenza type b, etc
-
Toxoid vaccine: Examples include Clostridium tetani, Corynebacterium diphtheria, etc.
Cellular Level
Cells of the innate immunity are:
-
Phagocytes (monocytes, macrophages, neutrophils, and dendritic cells)
-
Natural killer (NK) cells
Cells of the adaptive response are:
-
T Lymphocytes classified as CD4+T cells and CD8+T cells
-
B Lymphocytes differentiate into plasma cells, which produce specific antibodies
Development
Mesoderm cells are induced to form hemangioblasts, a common precursor for vessels and blood cell formation. The definitive hematopoietic stem cells derive from mesoderm surrounding the aorta called aorta-gonad-mesonephros region. These stem cells colonize the liver and after that are actively produced by the bone marrow by the seventh month of gestation.[4]
Organ Systems Involved
The organ systems involved in the immune response are primarily lymphoid organs which include, spleen, thymus, bone marrow, lymph nodes, tonsils, and liver. The lymphoid organ system classifies according to the following:
-
Primary lymphoid organs (thymus and bone marrow), where T and B cells first express antigen receptors and become mature functionally.
-
Secondary lymphoid organs like the spleen, tonsils, lymph nodes, the cutaneous and mucosal immune system; this is where B and T lymphocytes recognize foreign antigens and develop appropriate immune responses.
T lymphocytes mature in the thymus, where these cells reach a stage of functional competence while B lymphocytes mature in the bone marrow the site of generation of all circulating blood cells. Excessive release of cytokines stimulated by these organisms can cause tissue damage, such as endotoxin shock syndrome.
Anatomy
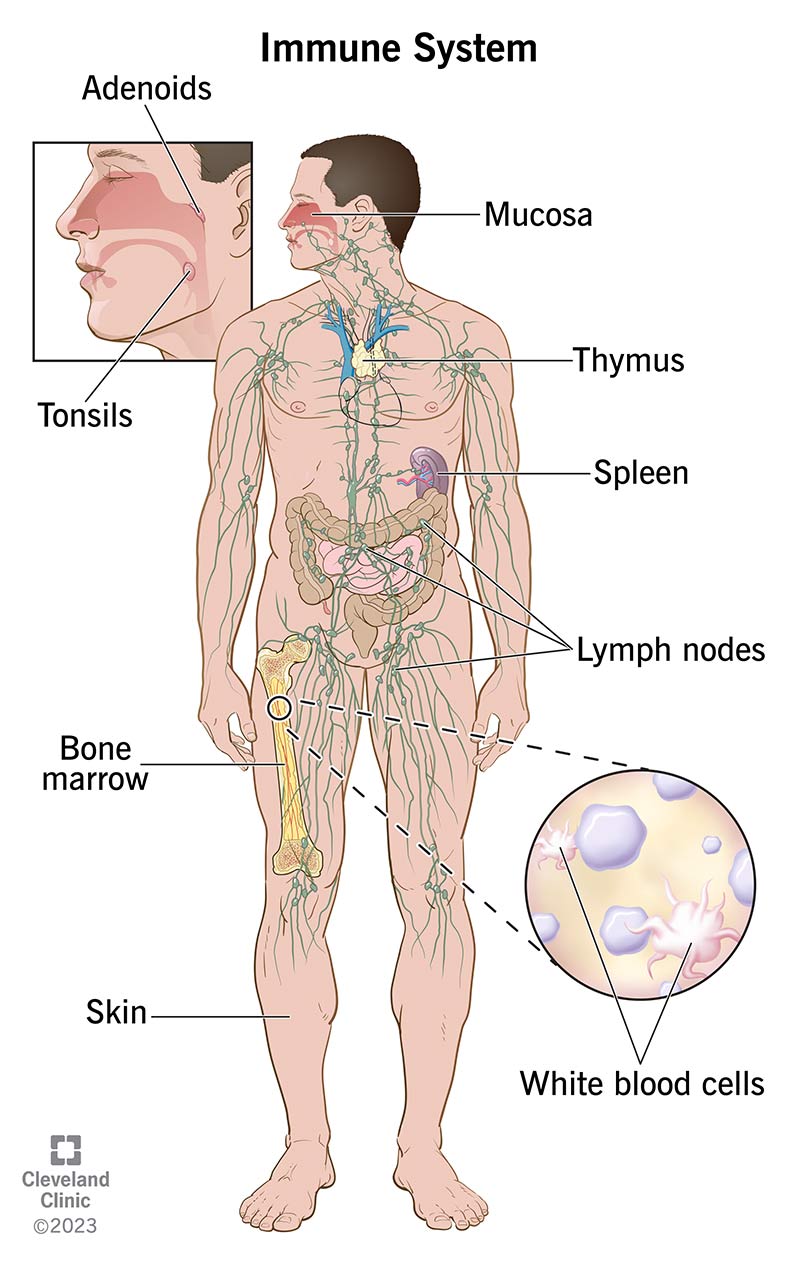
What parts of your body make up the immune system?
Many parts of your body, including immune system organs and cells, work together to keep you healthy. The main components of your immune system are:
- White blood cells. These immune system cells attack and eliminate harmful germs to keep you healthy. There are many types of white blood cells, and each type has a specific mission in your body’s defense system. Each type also has a different way of recognizing a problem, communicating with other cells and getting their job done.
- Antibodies. These proteins protect you from invaders by binding to them and initiating their destruction.
- Cytokines. These proteins serve as chemical messengers that tell your immune cells where to go and what to do. Different types of cytokines do different specific tasks, like regulating inflammation. Inflammation happens when your immune cells are warding off invaders or healing damage to your tissues.
- Complement system. This is a group of proteins that teams up with other cells in your body to defend against invaders and promote healing from an injury or infection.
- Lymph nodes. These small, bean-shaped organs are like colanders you use to drain pasta. They filter waste products from the fluid that drains from your tissues and cells (lymph) while keeping the good components, like nutrients. You have hundreds of lymph nodes throughout your body, and they’re a vital part of your lymphatic system.
- Spleen. This organ stores white blood cells that defend your body from invaders. It also filters your blood, recycling old and damaged cells to make new ones.
- Tonsils and adenoids. Located in your throat and nasal passage, tonsils and adenoids can trap invaders (like bacteria or viruses) as soon as they enter your body.
- Thymus. This small organ helps T-cells (a specific type of white blood cell) mature before they travel elsewhere in your body to protect you.
- Bone marrow. This soft, fatty tissue inside your bones is like a factory for your blood cells. It makes the blood cells your body needs to survive, including white blood cells that support your immune system.
- Skin. Your skin is a protective barrier that helps stop germs from entering your body. It produces oils and releases other protective immune system cells.
- Mucosa. This three-layered membrane lines cavities and organs throughout your body. It secretes mucus that captures invaders, like germs, for your body to then clear out.
Innate immunity vs. acquired immunity
Innate immunity is protection that you’re born with. Your innate immune system is part of your body’s first-line defense. It responds to invaders right away by attacking any organism that shouldn’t be in your body. It doesn’t need prior training to tell the difference between cells that belong in your body and those that don’t.
The white blood cells involved in innate immunity don’t learn to recognize certain invaders. They also have no memory of attacking invaders and don’t offer protection against specific germs (or the infections they cause) in the future.
That’s where acquired immunity comes into play. Acquired immunity, also called adaptive or specific immunity, is protection your body gains (acquires) over time from exposure to germs. Certain white blood cells called lymphocytes remember specific invaders and can tell when they don’t belong in your body. So, if those invaders try to get in again, the lymphocytes can quickly spring into action and work with other cells to eliminate the threat.
Vaccines support your acquired immunity by training its cells to identify and destroy invaders before they make you sick.
Function
The immune system responds variedly to different microorganisms often determined by the features of the microorganism. These are some different ways in which the immune system acts
Immune Response to Bacteria
Response often depends on the pathogenicity of the bacteria[5]:
-
Neutralizing antibodies are synthesized if the bacterial pathogenicity is due to a toxin
-
Opsonizing antibodies – produced as they are essential in destroying extracellular bacteria
-
The complement system is activated especially by gram-negative bacterial lipid layers
-
Phagocytes kill most bacteria utilizing positive chemotaxis, attachment, uptake and finally engulfing the bacteria
-
CD8+ T cells can kill cells infected by bacteria
Immune Response to Fungi [6]
-
The innate immunity to fungi includes defensins and phagocytes
-
CD4+ T helper cells are responsible for the adaptive immune response against fungi
-
Dendritic cells secrete IL-12 after ingesting fungi, and IL-12 activates the synthesis of gamma interferon which activates the cell-mediated immunity
Immune Response to Viruses [7]
-
Interferon, NK cells, and phagocytes prevent the spread of viruses in the early stage
-
Specific antibodies and complement proteins participate in viral neutralization and can limit spread and reinfection
-
The adaptive immunity is of foremost importance in the protection against viruses – these include CD8+ T cells that kill them and CD4+ T cells as the dominant effector cell population in response to many virus infections
Immune response to parasites[8]:
-
Parasitic infection stimulates various mechanisms of immunity due to their complex life cycle
-
Both CD4+ and CD8+ Cells protect against parasites
-
Macrophages, eosinophils, neutrophils, and platelets can kill protozoa and worms by releasing reactive oxygen radicals and nitric oxide
-
Increased eosinophil number and the stimulation of IgE by Th-2 CD4+ T cells are necessary for the killing of intestinal worms
-
Inflammatory responses also combat parasitic infections
Despite Immune response(s) generated by intact and functional Immune system we still fall sick, and this is often due to evasive mechanisms employed by these microbes. Here are some of those.
What does the immune system do
Your immune system works hard to keep you healthy. It does this by:
- Keeping invaders (like germs) out of your body.
- Destroying invaders.
- Limiting how much harm the invaders can do if they’re inside your body.
- Healing damage to your body.
- Adapting to new challenges and threats.
Invaders your immune system protects you against include:
- Bacteria.
- Viruses.
- Fungi that can cause infections.
- Parasites.
- Cancer cells.
How does the immune system work?
When your immune system is working properly, it:
- Tells the difference between cells that are yours and those that don’t belong in your body.
- Activates and mobilizes to kill germs that may harm you.
- Ends an attack once the threat is gone.
- Learns about germs after you’ve had contact with them and develops antibodies against them.
- Sends out antibodies to destroy germs that try to enter your body in the future.
But things don’t always go this smoothly. Sometimes, your immune system doesn’t work properly. For example, it may be too weak to fight off invaders, or it may launch too strong of a response.
Weak immune system
Many different conditions can weaken your immune system and make you more susceptible to infection. Conditions at birth are less common than those that develop later in life, like Type 2 diabetes and cancer.
Overactive immune system
At the other end of the spectrum, your immune system may react too strongly to invaders (real or perceived). It may mount an attack when there’s no invader. Or it may keep attacking after getting rid of an invader. An overactive immune system can lead to problems like autoimmune diseases or allergic reactions.
Strategies of Viruses to Evade the Immune System
Antigenic variation: It is a mutation in proteins that are typically recognized by antibodies and lymphocytes. HIV continually mutates, thus making it difficult for either the immune system to protect against it and also hinders the development of a vaccine.
By disrupting 2′,5′-oligoadenylate synthetase activity or by the production of soluble interferon receptors viruses disrupt the Interferon response.
By several mechanisms, Viruses affects the expression of MHC molecules.
A virus can infect immune cells: Normal T and B cells are also sites of virus persistence. HIV hides in CD4+T cells and EBV in B cells.
Strategies of Bacteria to Evade the Immune System
Intracellular pathogens may hide in cells: Bacteria can live inside metabolically damaged host leukocytes, and escaping from phagolysosomes (Shigella spp).
Other mechanisms:
-
Production of toxins that inhibit the phagocytosis
-
They are preventing killing by encapsulation
-
The release of catalase inactivates hydrogen peroxide
-
They infect cells and then cause impaired antigenic presentation
-
The organism may kill the phagocyte by apoptosis or necrosis
Strategies of Fungi to Evade the Immune System
-
Fungi produce a polysaccharide capsule, which inhibits the process of phagocytosis and overcoming opsonization, complement, and antibodies
-
Some fungi inhibit the activities of host T cells from delaying cell-mediated killing
-
Other organisms (e.g., Histoplasma capsulatum) evade macrophage killing by entering the cells via CR3 and them escape from phagosome formation
Strategies of Parasites to Evade the Immune System
-
Parasites can resist destruction by complement
-
Intracellular parasites can avoid being killed by lysosomal enzymes and oxygen metabolites
-
Parasites disguise themselves as a protection mechanism
-
Antigenic variation (e.g., African trypanosome) is an essential mechanism to evade the immune system
-
Parasites release molecules that interfere with immune system normal function
What disorders and diseases can affect the immune system?
Conditions that can interfere with the normal workings of your immune system include:
- Allergies. An allergy is your body’s reaction to a substance that’s normally harmless. Your immune system overreacts to the presence of that substance, leading to a range of symptoms from mild to severe.
- Autoimmune diseases. These conditions occur when your immune system attacks its own healthy cells by mistake. Lupus and rheumatoid arthritis are examples of common autoimmune diseases.
- Primary immunodeficiency diseases. These inherited conditions prevent your immune system from working properly. They make you more vulnerable to infections and certain diseases.
- Infectious diseases. Infectious diseases happen when germs enter your body, replicate and cause damage. HIV and mononucleosis (mono) are examples of infectious diseases that weaken your immune system and can lead to serious illness.
- Cancer. Certain types of cancer, like leukemia and lymphoma, can weaken your immune system. That’s because cancer cells may grow in your bone marrow or spread there from somewhere else. Cancer cells in your bone marrow interfere with the normal production of blood cells you need to fight infection.
- Sepsis. Sepsis is an extreme immune response to infection. Your immune system starts damaging healthy tissues and organs. This causes potentially life-threatening inflammation throughout your body.
Signs and symptoms of immune system disorders
Signs and symptoms vary depending on the condition and may include:
- Always feeling tired (fatigue).
- Unexplained fever.
- Unexplained weight loss.
- Drenching night sweats.
- Itchy skin.
- Sore, aching muscles.
- Fingers or toes that tingle or are numb.
- Trouble concentrating or paying attention.
- Hair loss.
- Inflammation, rashes or redness anywhere on your body.
- Swollen lymph nodes in your neck, armpits or groin.
Common tests that check the health of your immune system
Healthcare providers often use blood tests to check how well your immune system is working. Specific blood tests your provider may order include:
- Antibody test.
- Complete blood count.
- Complement blood test to check levels of specific types of protein in your blood, such as C3 proteins.
What medications can affect my immune system?
Some medications do important work in your body but in the process, can weaken your immune system. These include:
- Corticosteroids.
- Immunosuppressants.
- Chemotherapy and other forms of cancer treatment.
If you need any of these treatments, talk to your healthcare provider about how you can support your immune system.
Mechanism
The most important mechanisms of the immune system by which it generates immune response include:
Macrophages produce lysosomal enzymes and reactive oxygen species to eliminate the ingested pathogens. These cells produce cytokines that attract other leukocytes to the site of infection to protect the body. The innate response to viruses includes the synthesis and release of interferons and activation of natural killer cells that recognize and destroys the virus-infected cells. The innate immunity against bacterial consist of the activation of neutrophils that ingest pathogens and the movement of monocytes to the inflamed tissue where it becomes in macrophages. They can engulf, and process the antigen and then present it to a group of specialized cells of the acquired immune response. Eosinophils protect against parasitic infections by releasing the content of their granules.[9][10]
Antibody-dependent cell-mediated cytotoxicity (ADCC): A cytotoxic reaction in which Fc-receptor expressing killer cells recognize target cells via specific antibodies.
Affinity maturation: The increase in average antibody affinity mostly seen during a secondary immune response.
Complement system: It is a molecular cascade of serum proteins involved in the control of inflammation, lytic attack on cell membranes, and activation of phagocytes. The system can undergo activation by interaction with IgG or IgM (classical pathway) or by involving factors B, D, H, P, I, and C3, which interact closely with an activator surface to generate an alternative pathway C3 convertase.
Anergy: It is the failure to induce an immune response following stimulation with a potential immunogen.
Antigen processing: Conversion of an antigen into a form that can be recognized by lymphocytes. It is the initial stimulus for the generation of an immune response.
Antigen presentation: It is a process in which specific cells of the immune system express antigenic peptides in their cell membrane along with alleles of the major histocompatibility complex (MHC) which is recognizable by lymphocytes.
Apoptosis: Programmed cell death involving nuclear fragmentation and the formation of apoptotic bodies.
Chemotaxis: Migration of cells in response to concentration gradients of chemotactic factors.
Hypersensitivity reaction: A robust immune response that causes tissue damage more considerable than the one caused by an antigen or pathogen that induced the response. For instance, allergic bronchial asthma and systemic lupus erythematosus are an example of type I and type III hypersensitivity reactions respectively.
Inflammation: Certain reactions that attract cells and molecules of the immune system to the site of infection or damage. It featured increased blood supply, vascular permeability and increased transendothelial migration of blood cells (leukocytes).
Opsonization: A process of facilitated phagocytosis by deposition of opsonins (IgG and C3b) on the antigen.
Phagocytosis: The process by which cells (e.g., macrophages and dendritic cells) take up or engulf an antigenic material or microbe and enclose it within a phagosome in the cytoplasm.
Immunological tolerance: A state of specific immunological unresponsiveness.
Hypersensitivity Reactions
They are overreactive immune responses to antigens that would not normally cause an immune reaction.
Type 1 hypersensitivity reactions: Initial exposure to the antigen causes stimulates Th2 cells. They release IL-4 leading the B cells to switch their production of IgM to IgE antibodies which are antigen-specific. The IgE antibodies bind to mast cells and basophils, sensitizing them to the antigen.
When the body is exposed to the allergen again, it cross-links the IgE bound to the sensitized mast cells and basophils, causing the degranulation and release of preformed mediators including histamine, leukotrienes, and prostaglandins. This causes systemic vasodilation, bronchoconstriction, and increased permeability of vascular endothelium.
The reaction can be divided into two stages – 1) Immediate, in which release of preformed mediators cause the immune response, and 2) Late-phase response 8-12 hours later, in which the cytokines released in the immediate stage stimulate basophils, eosinophils, and neutrophils even though the allergen is removed.
Type 2 hypersensitivity reactions (Antibody dependant cytotoxic hypersensitivity): Immune response against the antigens present on the cell surface. Antibodies binding to the cell surface, activate the complement system and cause the degranulation of neutrophils and destruction of the cell. Such reactions can be targeted at self or non-self antigens. ABO blood group incompatibility leading to acute hemolytic transfusion reactions is an example of Type 2 hypersensitivity.
Type 3 hypersensitivity reactions are also mediated by circulating antigen-antibody complex that may be deposited in and damage tissues. Antigens in type 3 relations are soluble as opposed to cell-bound antigens in type 2.
Type 4 hypersensitivity reactions (delayed-type hypersensitivity reactions): They are mediated by antigen-specific activated T-cells. When the antigen enters the body, it is processed by antigen-presenting cells and presented together with the MHC II to a Th1 cell. If the T-helper cell has already been sensitized to that particular antigen, it will be stimulated to release chemokines to recruit macrophages and cytokines such as interferon-γ to activate them. This causes local tissue damage. The reaction takes longer than all other types, around 24 to 72 hours.
Transplant Rejection
-
Xenografts are grafts between members of different species, triggers the maximal immune response. Rapid rejection.
-
Allografts are grafts between members of the same species.
-
Autografts are grafts from one part of the body to another. No rejection.
-
Isografts are grafts between genetically identical individuals. No rejection.
Hyperacute Rejection: In hyperacute rejection, the transplanted tissue is rejected within minutes to hours because vascularization is rapidly destroyed. Hyperacute rejection is antibody mediated and occurs because the recipient has preexisting antibodies against the graft, which can be due to prior blood transfusions, multiple pregnancies, prior transplantation, or xenografts. Activation of the complement system leads to thrombosis in the vessels peventing the vascularization of the graft.
Acute Rejection: Develops within weeks to months. Involves the activation of T lymphocytes against donor MHCs. May also involve humoral immune response, which antibodies developing after transplant. It manifests as vasculitis of graft vessels with dense interstitial lymphocytic infiltrate.
Chronic Rejection: Chronic rejection develops months to years after acute rejection episodes have subsided. Chronic rejections are both antibody- and cell-mediated. The use of immunosuppressive drugs and tissue-typing methods has increased the survival of allografts in the first year, but chronic rejection is not prevented in most cases. It generally presents as fibrosis and scarring. In heart transplants, chronic rejection manifests as accelerated atherosclerosis. In transplanted lungs, it manifests as bronchiolitis obliterans. In liver transplants, it manifests as vanishing bile duct syndrome. In kidney recipients, it manifests as fibrosis and glomerulopathy.
Graft-versus-host Disease: The onset of the disorder varies. Grafted immunocompetent T cells proliferate in the immunocompromised host and reject host cells which they consider ‘nonself’ leading to severe organ dysfunction. It is a type 4 hypersensitivity reaction and manifests as maculopapular rash, jaundice, diarrhea, hepatosplenomegaly. Usually occurs in the bone marrow and liver transplants, which are rich in lymphocytes.
Related Testing
The immunological investigations for the study of innate and adaptive immunity are listed below and include the assessment of immunoglobulins, B and T-lymphocyte counts, lymphocyte stimulation assays, quantification of components of the complement system and phagocytic activity.[11][12][13][14][15]
Quantitative Serum Immunoglobulins
-
IgG
-
IgM
-
IgA
-
IgE
IgG Sub-Classes
-
IgG1
-
IgG2
-
IgG3
-
IgG4
Antibody Activity
IgG antibodies (post-immunization)
-
Tetanus toxoid
-
Diphtheria toxoid
-
Pneumococcal polysaccharide
-
Polio
IgG antibodies (post-exposure)
-
Rubella
-
Measles
-
Varicella Zoster
Detection of isohemagglutinins (IgM)
-
Anti-type A blood
-
Anti-type B blood
Other assays
-
Test for heterophile antibody
-
Anti-streptolysin O titer
-
Immunodiagnosis of infectious diseases (HIV, hepatitis B, and C, HTLV and dengue)
-
Serum protein electrophoresis
Blood Lymphocyte Subpopulations
-
Total lymphocyte count
-
T lymphocytes (CD3, CD4, and CD8)
-
B lymphocytes (CD19 and CD20)
-
CD4/CD8 ratio
Lymphocyte Stimulation Assays
-
Phorbol ester and ionophore
-
Phytohemagglutinin
-
Antiserum to CD3
Phagocytic Function
Nitroblue tetrazolium (NBT) test (before and after stimulation with endotoxin)
-
Unstimulated
-
Stimulated
Neutrophil mobility
-
In medium alone
-
In the presence of chemoattractant
Complement System Evaluation
Measurement of individuals components by immunoprecipitation tests, ELISA, or Western blotting
-
C3 serum levels
-
C4 serum levels
-
Factor B serum levels
-
C1 inhibitor serum levels
Hemolytic assays
-
CH50
-
CH100
-
AH50
Complement system functional studies
-
Classical pathway assay (using IgM on a microtiter plate)
-
Alternative pathway assay (using LPS on a microtiter plate)
-
Mannose pathway assay (using mannose on a microtiter plate)
Measurement of complement-activating agents
-
Circulating immune complexes
-
Cold agglutinins
Assays for complement-binding
-
C1q autoantibody ELISA
-
C1 inhibitor autoantibody ELISA
Others complement assays
-
LPS activation assay
-
Specific properdin test
-
C1 inhibitor activity test
Autoimmunity Studies
-
Anti-nuclear antibodies (ANA)
-
Detection of specific auto-immune antibodies for systemic disorders (anti-ds DNA, rheumatoid factor, anti-histones, anti-Smith, anti-(SS-A) and anti-(SS-B)
-
Detection of anti-RBC, antiplatelet, and anti-neutrophil
-
Testing for organ-specific auto-immune antibodies
Microbiological Studies
-
Blood (bacterial culture, HIV by PCR, HTLV testing)
-
Urine (testing for cytomegalovirus, sepsis, and proteinuria)
-
Nasopharyngeal swab (testing for Rhinovirus)
-
Stool (testing for viral, bacterial or parasitic infection)
-
Sputum (bacterial culture and pneumocystis PCR)
-
Cerebrospinal fluid (culture, chemistry, and histopathology)
Coagulation Tests
-
Factor V assay
-
Fibrinogen level
-
Prothrombin time
-
Thrombin time
-
Bleeding time
Other Investigations
-
Complete blood cell count
-
Tuberculin test
-
Bone marrow biopsy
-
Histopathological studies
-
Liver function test
-
Blood chemistry
-
Tumoral markers
-
Serum levels of cytokines
-
Chest x-ray
-
Diagnostic ultrasound
-
CT scan
-
Fluorescent in situ hybridization (FISH)
-
DNA testing (for most congenital disorders)
How can I boost my immune system naturally?
No one likes getting sick, and it’s common to wonder how to improve or strengthen your immune system. Because your immune system is complex, there’s no fast and easy answer that works for everyone on how to build it up. That’s why it’s important to talk to a healthcare provider. They can give you individualized advice based on your medical history. They’ll also talk to you about your lifestyle and daily habits to see what changes you can make.
Here are some general tips to keep your immune system running smoothly:
- Fill your plate with healthy foods. Fruits, veggies, lean sources of protein and whole grains are just some examples of foods that bolster immune function. Talk to your provider about how different ways of eating, like the Mediterranean diet, can help give you the vitamins you need for a healthy immune system.
- Build exercise into your daily routine. Exercise helps many aspects of your health, including your immune function. Your provider can help you get started with an exercise plan that fits your medical needs and lifestyle.
- Keep a weight that’s healthy for you. Researchers have linked a body mass index (BMI) greater than 30 (obesity) to poorer immune function. Ask your provider what your target weight range should be, and work together to reach it.
- Catch enough ZZZs. Not getting enough sleep can prevent your immune system from working as it should.
- Stay up-to-date on vaccines. Vaccines train your body to fight off germs that can make you sick. Talk to your provider about which vaccines you need and when.
- Avoid smoking and all tobacco products. Tobacco use raises your risk for conditions that can harm your immune system, like rheumatoid arthritis. If you use tobacco, talk to your provider about effective ways to quit.
Pathophysiology
The immune system protects the body against many diseases including recurrent infections, allergy, tumor, and autoimmunity. The consequences of an altered immunity will manifest in the development of many immunological disorders some of which are listed below:
-
X- linked agammaglobulinemia (Bruton disease)
-
Selective IgA Deficiency
-
Selective IgG deficiency
-
Congenital thymic aplasia (DiGeorge Syndrome)
-
Chronic mucocutaneous candidiasis
-
Hyper-IgM syndrome
-
Interleukin-12 receptor deficiency
-
Severe combined immunodeficiency disease (SCID)
-
ZAP-70 deficiency
-
Janus kinase 3 deficiency
-
RAG1 and RAG2 deficiency
-
Wiskott-Aldrich syndrome
-
Immunodeficiency with ataxia-telangiectasia
-
MHC deficiency (bare leukocyte syndrome)
-
Complement system deficiencies
-
Hereditary angioedema
-
Chronic granulomatous disease (CGD)
-
Leukocyte adhesion deficiency syndrome
-
Job syndrome
-
Chediak Higashi syndrome
-
Acquired immunodeficiency syndrome
-
Anaphylaxis
-
Allergic bronchial asthma
-
Allergic rhinitis
-
Allergic conjunctivitis
-
Food allergy
-
Atopic eczema
-
Drug allergy
-
Immune thrombocytopenia
-
Autoimmune hemolytic anemia
-
Autoimmune neutropenia
-
Systemic lupus erythematosus
-
Rheumatoid arthritis
-
Autoimmune hepatitis
-
Hemolytic disease of the fetus and the newborn (erythroblastosis fetalis)
-
Myasthenia gravis
-
Goodpasture syndrome
-
Pemphigus
-
Tuberculosis
-
Contact dermatitis
-
Leprosy
-
Insulin-dependent diabetes mellitus
-
Schistosomiasis
-
Sarcoidosis
-
Crohn disease
-
Autoimmune lymphoproliferative syndrome
-
X-linked lymphoproliferative disorder
-
Common variable immunodeficiency
-
B-cell chronic lymphocytic leukemia
-
B-cell prolymphocytic leukemia
-
Non-Hodgkin lymphoma (including mantle cell lymphoma) in leukemic phase
-
Hairy cell leukemia
-
Multiple myeloma
-
Splenic lymphoma with villous lymphocytes
-
Sezary syndrome
-
T-cell prolymphocytic leukemia
-
Adult T-cell leukemia-lymphoma
-
Large granulated lymphocyte leukemia
-
Leukocyte adhesion deficiency syndrome
-
Chronic active hepatitis
-
Coccidioidomycosis
-
Behcet disease
-
Aphthous stomatitis
-
Familial keratoacanthoma
-
Autoimmune polyendocrinopathy candidiasis ectodermal dystrophy
-
Idiopathic CD4+ lymphocytopenia
-
Complement system deficiencies
-
ADA-SCID
-
Artemis SCID
-
Newly diagnosed non-germinal center B-cell subtype of diffuse large B-cell lymphoma
-
Melanoma
-
Chagas disease
Clinical Significance
Highly specific and discriminatory immunity is of utmost importance for survival. The immune system has evolved as a collection of protective mechanisms to defend the host against a long list of potential invaders that would take advantage in immunodeficiency disorders, inflammatory diseases, cancers, and autoimmunity. This system has to be sophisticated enough to recognize “self” from “non-self” and provide help in infections, malignant tumors, organ transplantations, and various other situations the immune system encounters.
Disclaimer: Each person’s journey is unique, treatment plan, life style, food habit, hormonal condition, immune system, chronic disease condition, previous medical history is also unique. So always seek the best advice from a qualified medical professional or health care provider before trying any treatments to ensure to find out the best plan for you. This guide is for general information and educational purposes only. If you or someone are suffering from this disease condition bookmark this website or share with someone who might find it useful! Boost your knowledge and stay ahead in your health journey. Thank you for giving your valuable time to read the article.







