Degeneration Disc means abnormality of bone and joint particularly in the moving sections of the spine (cervical and lumbar levels) is a natural process of aging. This dehydration or desiccation of the disc material reduces the flexibility and typically the height of the disc. In most patients, the mere presence of degenerative discs is not a problem leading to pain, neurological compression, or other symptoms. However, in a certain number of patients, the disc degeneration leads to spinal “instability,” the condition in which the spine is unable to bear the patient’s weight or perform its normal functions without disabling pain. In these circumstances, treatments are available to try to reduce the patient’s pain.
Degenerative disc disease of the cervical spine typically develops in the aging population equally in terms of patient sex. Patients are most commonly present with pain. Pain, or in combination with other neurological symptoms, may require surgical intervention. Treatment options range from nonoperative measures to decompression, instrumented fusion, or a combination of both laminoplasty or instrumentation or a combination of both. This chapter will examine the anatomy, natural history, etiology, pathophysiology, evaluation, and treatment options.
Pathophysiology
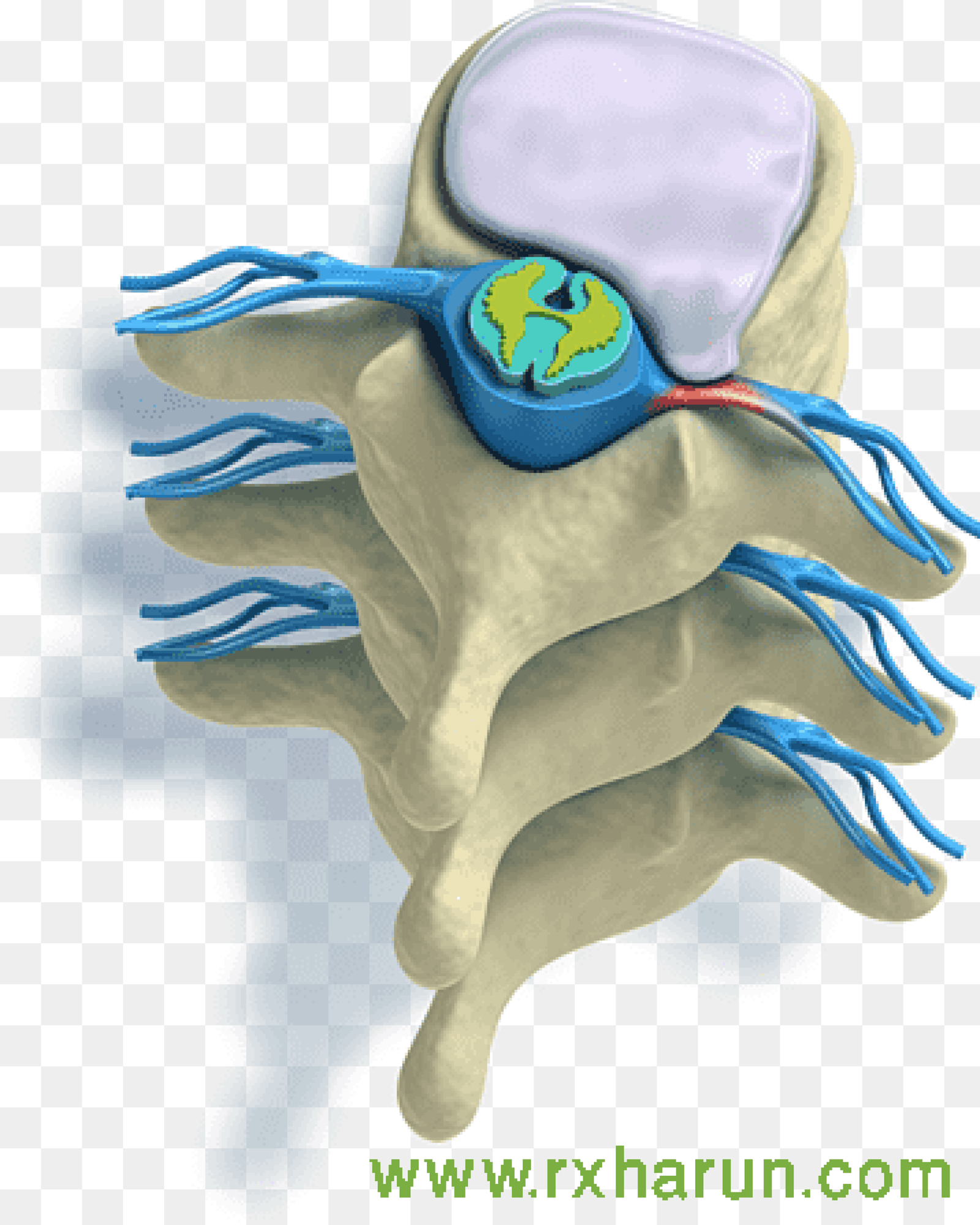
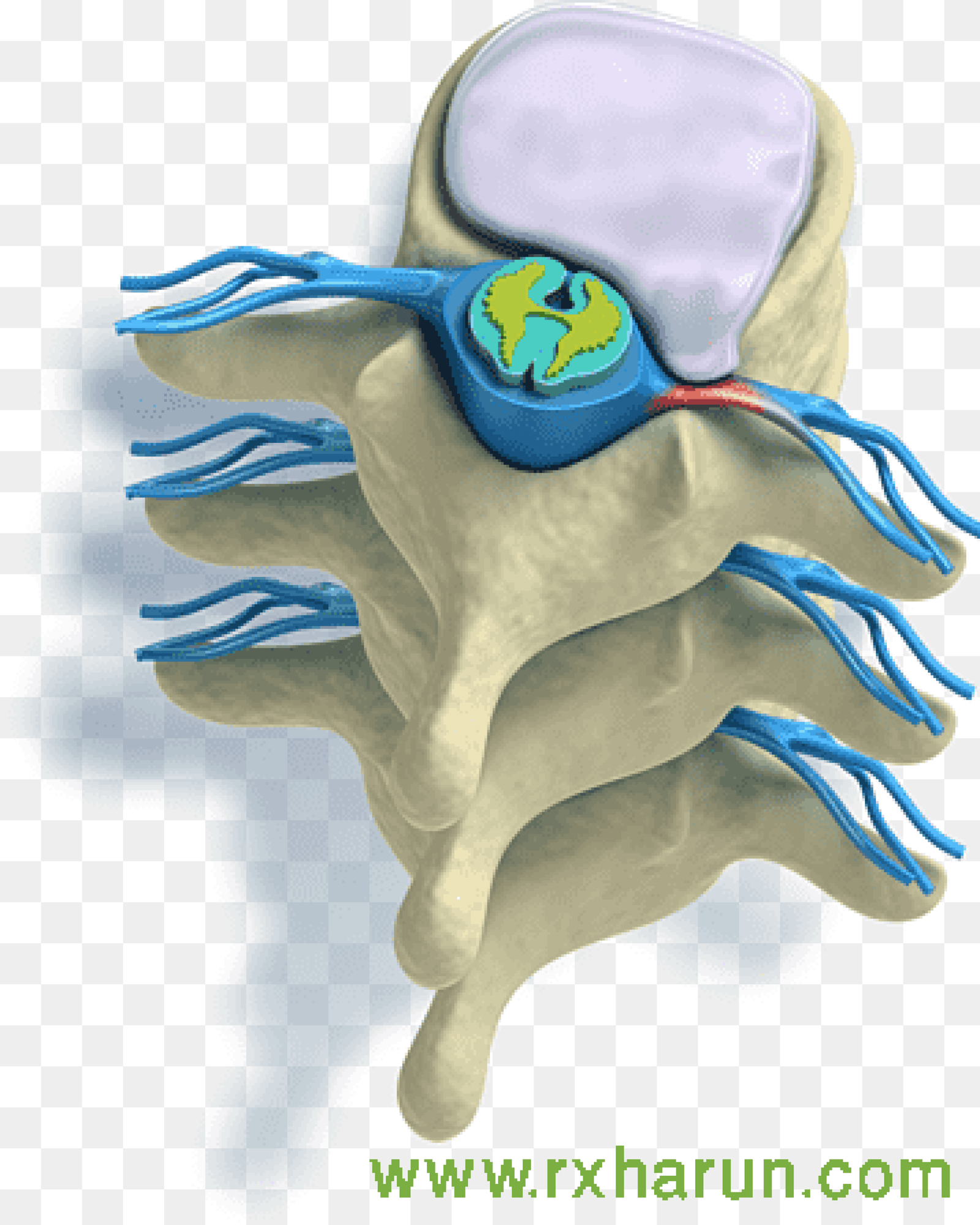
The radiation of back pain associated with disc disease is thought to be due to the compression of the nerve roots in the spinal canal from either one or a combination of, the following elements
Disc herniation material (i.e. herniated nucleus pulposus, HNP)
-
Varying degrees of HNP is recognized, from disc protrusion (annulus remains intact), extrusion (annular compromise, but herniated material remains continuous with disc space), to sequestered (free) fragments
-
HNP material predictably is resorbed over time, with the sequestered fragment demonstrating the highest degree of resorption potential
-
In general, 90% of patients will have a symptomatic improvement in radicular symptoms within 3 months following nonoperative protocols alone
Hypertrophy/expansion of degenerative tissues
-
Common sources include ligamentum flavum and the facet joint. The facet joint itself undergoes degenerative changes (just like any other joint in the body) and synovial hypertrophy and/or associated cysts can compromise surrounding nerve roots.
In a 2010 study by Suri et al. 662% of 154 consecutive patients presenting with new lumbar disk herniation noted spontaneous symptoms compared to just 26% who reported the symptoms starting after a specific household task or seemingly common non-lifting activity. Contrary to popular belief, fewer than 8% reported acute sciatica after heavy lifting or physical trauma.[rx]
The many tiny blood vessels surrounding the spinal cord and nerve roots are paramount to delivering nutrition, oxygen, and chemomodulators. The compression of these structures limits the ability of these vessels to deliver vital nutrients, resulting in an ischemic effect of the structure. The subsequent inflammation from intervertebral disc compression results in (ischemic) pain along the path of this nerve root. This nerve compression from the disc causes an increase in cytokines, TNF-alpha, and the recruitment of macrophages. Interestingly, the extent of the histologic changes within the intervertebral disc has a positive correlation with body mass index, indicating that those with obesity may be more prone to degeneration.

Causes of Degenerative Disc
Disc degeneration is directly correlated with increasing patient age. Interestingly, while it is thought that men likely start this degeneration almost ten years earlier than women, women with disc degeneration are likely to be more susceptible to the effects (e.g., malalignment, instability).[rx][rx][rx]
Traditionally, dating back to the traditional views regarding the etiologies of disc degeneration focused on environmental exposures such as smoking, vehicular vibration, and occupation. More recent research has highlighted the genetic components associated with disc disease and shifted the paradigm away from the aforementioned social, occupational, and environmental factors.
The contemporary general consensus advocates the importance of these genetic factors as the most important predictors of disc degeneration, and the environmental factors are recognized as additional, minor contributors to disease onset. The effects of smoking also have been questioned with more recent research only finding weak correlations with cigarette use and disc disease. Similarly, while occupational aspects (e.g., heavy lifting, forceful bending) may have some contributions to lumbar degeneration, it is now thought that socioeconomic factors likely confound these studies, and occupational exposure is, at most, a minor contributor to disc disease.
- Disc herniation and disc degeneration – are associated terms, being nucleus pulposus herniation a possible evolution from a degenerative disc. Disc degeneration is usually associated with the loss of proteoglycans.[rx] Multiple factors influence the degenerative process such as genetic, mechanical, and behavioral.[rx][rx]
- Mechanical load – is important in maintaining a healthy IVD by generating signals to cells that regulate proper matrix homeostasis.[rx][rx] On the other hand, prolonged exposure to hypo- or hyper-loading correlates with disc degeneration induction.[rx][rx]
- Repetitive trauma – such as poor posture, poor ergonomics, or repetitive heavy work can lead to disc degeneration and a bulging disc. These long term injuries are often also associated with poor muscle strength, obesity, and other factors such as smoking.
- An Injury caused – by sudden forces or load on the disc such as a car accident or an awkward heavy lift. This sudden increase in pressure on the disc can cause damage and tears to the annulus that causes a bulging disc.
- Spinal Degeneration – While some degeneration is a normal part of the aging process, poor spinal function and posture will dramatically speed up disc degeneration with a bulging disc.
- People who have led a sedentary lifestyle or those who smoke – increase the chances for bulging discs.
- Continuous strain on the disc from injury or heavy lifting – and strain can wear them down throughout the years.
- Weakened back muscles – can accelerate the process and may lead to a sudden herniation of the weakened disc. Although bulging discs occur over time, herniated discs may occur quickly by trauma.
- Bad posture – including improper body positioning during sleep, sitting, standing, or exercise are all risk factors that may contribute to the development of a bulging disc.
- Obesity
- High contact sports or activities – are also risk factors.
- Runners who fail to use shoes that provide orthopedic support – may also develop bulging discs.
- Activities that place stress and strain on the spine – can lead to the weakening of the discs.

Symptoms of Degenerative Disc
Evidence of a bulging disc may range from mild tingling and numbness to moderate or severe pain, depending on the severity. In most cases, when a bulging disc has reached this stage it is near or at herniation.
- Tingling or pain in the fingers, hands, arms, neck or shoulders – This could indicate a bulging disc in the cervical area.
- Pain in the feet, thighs, lower spine and buttocks – This is the most common symptom and could indicate an issue in the lumbar region.
- Difficulty walking or feeling of impairment while lifting or holding things.
- Loss of Bladder or Bowel Function – There are some bulging disc cases where professional care is essential. In some cases, such as when you lose bowel or bladder control, it is deemed an emergency, and you may require immediate surgery. These bulges usually are very significant and affect your nerve control involving your bladder or bowels. You should go straight to your nearest emergency department in these instances.
- Weakness in your limb muscles – is a significant concern. If you experience arm, hand, leg or foot weakness, please seek prompt medical assessment.
- The reduced or altered sensation – is your next priority. Mild disc bulges can reduce your ability to feel things touching you, e.g. numbness or pins and needles. If you experience any of the above symptoms, you should seek professional assistance.
- Referred Pain – Pain in your limbs, e.g. legs (sciatica) or arms (brachialgia) is usually a more significant injury than when experiencing only spinal pain. We recommend that you seek the professional advice of your trusted spinal care practitioner.
- Spinal Pain – Interestingly, if you are only experiencing spinal pain, bulging discs are generally mild injuries and the most likely to rehabilitate quickly. Please adhere to low disc pressure postures and exercise accordingly. If in doubt, please seek professional advice.
- Intermittent or continuous back pain. This may be made worse by movement, coughing, sneezing, or standing for long periods of time.
- Spasm of the back muscles
- Sciatica. Pain that starts near the back or buttock and travels down the leg to the calf or into the foot.
- Muscle weakness in the legs
- Numbness in the leg or foot
- Decreased reflexes at the knee or ankle
- Changes in bladder or bowel function
Associate clinical feature is
- Severe back pain
- Saddle anesthesia i.e., anesthesia or paraesthesia involving S3 to S5 dermatomes, including the perineum, external genitalia, and anus; or more descriptively, numbness or “pins-and-needles” sensations of the groin and inner thighs which would contact a saddle when riding a horse.
- Bladder and bowel dysfunction, caused by a decreased tone of the urinary and anal sphincters.
- Detrusor weaknesses causing urinary retention and post-void residual incontinence as assessed by bladder scanning the patient after the patient has urinated.
- Sciatica type pain on one side or both sides, although pain may be wholly absent
- The weakness of the muscles of the lower legs (often paraplegia)
- Pain in one leg (unilateral) or both legs (bilateral) that starts in the buttocks and travels down the back of the thighs and legs (sciatica)
- Numbness in the groin or area of contact if sitting on a saddle (perineal or saddle paresthesia)
- Bowel and bladder disturbances
- Lower extremity muscle weakness and loss of sensations
- Inability to urinate (urinary retention)
- Difficulty initiating urination (urinary hesitancy)
- The decreased sensation when urinating (decreased urethral sensation)
- Inability to stop or control urination (incontinence)
- Reduced or absent lower extremity reflexes
- Local pain is generally a deep, aching pain resulting from soft tissue and vertebral body irritation.
- Leg pain (radicular pain) is generally a sharp, stabbing pain resulting from compression of the nerve roots.
- Radicular pain projects along with the specific areas controlled by the compressed nerve (known as a dermatomal distribution).
- Inability to stop or feel a bowel movement (incontinence)
- Constipation
- Loss of anal tone and sensation
- Achilles (ankle) reflex absent on both sides.
- Sexual dysfunction
- Absent anal reflex and bulbocavernosus reflex
- Gait disturbance
These symptoms require immediate medical evaluation as they may be a sign of a potentially life-threatening condition.
Diagnosis of Degenerative Disc
History
Patient history should focus on the timeline of pain, radiation of pain, and inciting events. Careful attention to prior episodes of trauma should be noted. Classically, patients complain of pain radiating down both buttocks and lower extremities. It is helpful to determine if the pain is localized to the lower back or if there is radiation into the leg(s). A presentation of radiating pain correlates with canal stenosis. Radiating pain as the main issue has a much more predictable surgical outcome compared to a presentation of non-specific lower back pain that likely is related to muscle fatigue and strain. A mechanical component to the back pain (i.e., the pain only with certain movements) may indicate instability or a degenerative pars fracture. It also is important in any evaluation of extremity issues to inspect circulation, as vascular claudication may mirror or mimic the neurogenic issues.[rx]
Physical Examination
All physical examinations will include the evaluation of the neurologic function of the arms, legs, bladder, and bowels. The keys to a thorough exam are organization and patience. One should not only evaluate strength, but also sensation and reflexes. It is also important to inspect the skin along the back and document the presence of tenderness to compression or any prior surgical scars.
A physical exam for diagnosing disc pain may include one or more of the following tests:
- Palpation – Palpating (feeling by hand) certain structures can help identify the pain source. For example, worsened pain when pressure is applied to the spine may indicate sensitivity caused by a damaged disc.
- Movement tests – Tests that assess the spine’s range of motion may include bending the neck or torso forward, backward, or to the side. Additionally, if raising one leg in front of the body worsens leg pain, it can indicate a lumbar herniated disc (straight leg raise test).
- Muscle strength – A neurological exam may be conducted to assess muscle strength and determine if a nerve root is compressed by a herniated disc. A muscle strength test may include holding the arms or legs out to the side or front of the body to check for tremors, muscle atrophy, or other abnormal movements.
- Reflex test – Nerve root irritation can dampen reflexes in the arms or legs. A reflex test involves tapping specific areas with a reflex hammer. If there is little or no reaction, it may indicate a compressed nerve root in the spine.
- The straight leg raise test – The straight leg raise (SLR) test consists of a supine patient having his/her fully extended leg passively stretched from 0 to about 80 degrees. The onset of radiating back pain in either leg supports a diagnosis of a stenotic canal. A herniation compressing the L5 nerve root will present as a weakness of ankle dorsiflexion and an extension of the great toe. This deficit also may diminish the Achilles tendon reflex. L4 radiculopathy may present with weakness at the quadriceps and a decreased patellar tendon reflex.
- The contralateral (crossed) straight leg raise test – As in the straight leg raise test, the patient is lying supine, and the examiner elevates the asymptomatic leg. The test is positive if the maneuver reproduces the patient’s typical pain and paresthesia. The test has a specificity higher than 90%.
- Wadell Signs – A comprehensive examination should also include ruling out non-organic causes of low back pain/symptoms. When the clinician suspects potential malingering, consideration should be given to the following: Nonspecific description of symptoms or inconsistency, including superficial/non-anatomic sites of tenderness on exam. Pain with axial load/rotational movements. Negative SLR with patient distraction (one approach includes having the patient sitting in a chair and reproducing the SLR “environment”). Non-dermatomal patterns of distribution of symptoms. Pain out of proportion on the exam

Lab Test
- A medical history – in which you answer questions about your health, symptoms, and activity.
- Erythrocyte sedimentation rate and C-reactive protein – are inflammatory markers, and they are requested if suspicious for a chronic inflammatory condition or infectious cause as the etiology. A complete blood count is useful when suspecting infection or malignancy.
- A physical exam to assess your strength – reflexes, sensation, stability, alignment, and motion. You may also need blood tests.
- Laboratory testing – may include white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).
- Elevated ESR – could indicate infection, malignancy, chronic disease, inflammation, trauma, or tissue ischemia.
- Elevated CRP – levels are associated with infection.
Imaging
- X-rays – X-ray is the initial workup study when there is a strong suspicion of a specific cause of cervical or back pain (fracture, infection, tumor) or in the presence of red flags (fever, age more than 50, recent trauma, pain at night or rest, unexplained weight loss, progressive motor or sensory deficit, saddle anesthesia, history of cancer or osteoporosis, failure to improve after six weeks of conservative treatment). Anteroposterior and lateral x-ray is helpful to assess fracture, bony deformity, decreased intervertebral height, osteophytes, spondylolisthesis, and facet joint osteoarthritis.
- Magnetic Resonance Imaging (MRI) scan – MRI is the recommended diagnostic imaging in cases of severe or progressive neurologic deficits, suspicion of an underlying condition such as infection, fracture, cauda equina syndrome, spinal cord compression. In cases of radiculopathy, most of the cases improve with conservative treatment and MRI is indicated in those cases with significant pain or neurologic deficits.[rx]
- A myelogram – is a specialized X-ray where dye is injected into the spinal canal through a spinal tap. An X-ray fluoroscope then records the images formed by the dye. The dye used in a myelogram shows up white on the X-ray, allowing the doctor to view the spinal cord and canal, a bulging disc in detail. Myelograms can show a nerve being pinched and a bulging disc by a herniated disc, bony overgrowth, spinal cord tumors, and abscesses. A CT scan may follow this test.
- Computed Tomography (CT) scan – is a noninvasive test that uses an X-ray beam and a computer to make 2-dimensional images of your spine. It may or may not be performed with a dye (contrast agent) injected into your bloodstream. This test is especially useful for confirming which bulging disc is damaged. CT scan is not usually requested in nucleus pulposus herniation. However, it can be helpful in some cases when there is a suspicion of calcified disc herniation (thoracic disc herniation has a 30 to 70% rate of calcification) which is more challenging especially when surgery is a consideration.
- Electromyography (EMG) & Nerve Conduction Studies (NCS) – EMG tests measure the electrical activity of your muscles. Small needles are placed in your muscles, and the results are recorded on a special machine. NCS is similar, but it measures how well your nerves pass an electrical signal from one end of the nerve to another. These tests can detect nerve damage and muscle weakness and a bulging disc.
- Discogram – A discogram may be recommended to confirm which bulging disc is painful if surgical treatment is considered. In this test, the radiographic dye is injected into the disc to recreate disc pain from the dye’s added pressure.
In the presence of low back pain without symptoms of radiculopathy, there is no need to request studies as most of the patients improve in a couple of weeks, a 4-week follow-up is a usual timeframe.[rx]
Treatment of Degenerative Disc
In the setting of “red-flags,” aggressive diagnosis and likely surgical options should be explored. Examples of these red flags include:
-
Cauda equina syndrome (issues controlling bowel/bladder, difficulty starting urination)
-
Infection (high suspicion in IV drug user, history of fever, nighttime chills)
-
Tumor suspected (known history of cancer; new-onset weight loss)
Non-Surgical
- Spine-Specialized physical therapy – typically includes a combination of stretching, strengthening, and aerobic exercise to provide better stability and support for the spine.
- Massage therapy – can help reduce muscle tension and muscle spasms, which may add to back or neck pain. Muscle tension is especially common around an unstable spinal segment where a disc is unable to provide the necessary support
- Ice & Moist Heat Application – Ice application where the ice is wrapped in a towel or an ice pack for about 20 minutes to the affected region, thrice a day, helps in relieving the symptoms of a disc bulge. Heat application in the later stages of treatment also provides the same benefit.
- Hot Bath – Taking a hot bath or shower also helps in dulling the pain from a disc bulge. Epsom salts or essential oils can be added to a hot bath. They will help in soothing the inflamed region.
- Traction – traction is the best essential treatment for bulging discs, pinched nerve, radiating pain management. It can be done in a manual and dynamic way to relieves pain in bulging discs.
- Massage therapy – may give short-term pain relief, but not functional improvement, for those with acute lower back pain. It may also give short-term pain relief and functional improvement for those with long-term (chronic) and sub-acute lower back pain, but this benefit does not appear to be sustained after 6 months of treatment. There does not appear to be any serious adverse effects associated with massage.
- Acupuncture – may provide some relief for back pain. However, further research with stronger evidence needs to be done.
- Spinal manipulation – is a widely-used method of treating back pain, although there is no evidence of long-term benefits.
- Back school – is an intervention that consists of both education and physical exercises. A 2016 Cochrane review found the evidence concerning back school to be very low quality and was not able to make generalizations as to whether the back school is effective or not.
- Patient education – on proper body mechanics (to help decrease the chance of worsening pain or damage to the disk)
- Physical therapy – which may include ultrasound, massage, conditioning, and exercise. The goal of physical therapy is to help you return to full activity as soon as possible and prevent re-injury. Physical therapists can instruct you on proper posture, lifting, and walking techniques, and they’ll work with you to strengthen your lower back, leg, and stomach muscles. They’ll also encourage you to stretch and increase the flexibility of your spine and legs. Exercise and strengthening exercises are key elements to your treatment and should become part of your life-long fitness.
- Over the Door Traction – This is a very effective treatment for a disc bulge. It helps in relieving muscle spasms and pain. Typically a 5 to 10-pound weight is used and it is important that patients do this under medical guidance.
- Weight control – By keto diet or maintaining or changing the food habit to reduce the weight not any movement during the time of acute pain.
- Use of a lumbosacral back support
- Typically – conservative therapy is the first line of treatment to manage lumbar disk disease. Approach for Treating and Reversing a Disc Bulge about half of the disc bulges heal within six months and only about 10% of the disc bulges require surgery. So, the good news is that conservative treatment for a disc bulge helps in treating as well as reversing the disc bulges.
- Eat Nutritiously During Your Recovery – All bones and tissues in the body need certain nutrients in order to heal properly and in a timely manner. Eating a nutritious and balanced diet that includes lots of minerals and vitamins are proven to help heal back pain of all types. Therefore focus on eating lots of fresh produce (fruits and veggies), whole grains, lean meats, and fish to give your body the building blocks needed to properly healing PLID. In addition, drink plenty of purified water, milk, and other dairy-based beverages to augment what you eat.
- In bulging disc needs ample minerals (calcium, phosphorus, magnesium, boron) and protein to become strong and healthy again.
- Excellent sources of minerals/protein include dairy products, tofu, beans, broccoli, nuts and seeds, sardines and salmon.
- Important vitamins that are needed for bone healing include vitamin C (needed to make collagen), vitamin D (crucial for mineral absorption), and vitamin K (binds calcium to bones and triggers collagen formation).
- Conversely, don’t consume food or drink that is known to impair bone/tissue healing, such as alcoholic beverages, sodas, most fast food items and foods made with lots of refined sugars and preservatives.
Medications
- Analgesics – Such as paracetamol and prescription-strength drugs that relieve pain but not inflammation.
- Muscle Relaxants – These medications provide relief from spinal muscle spasms. Muscle relaxants, such as baclofen, tolperisone, eperisone, methocarbamol, carisoprodol, and cyclobenzaprine, may be prescribed to control muscle spasms.
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include mainly or first choice etodolac, then aceclofenac, etoricoxib, ibuprofen, and naproxen.
- Calcium & vitamin D3 – To improve bone health and healing fracture. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tightening the loose tendon, cartilage, ligament, and cartilage, ligament regenerates cartilage or inhabits the further degeneration of cartilage, ligament.
- Dietary supplement – to remove general weakness & improved health.
- Vitamin B1, B6, and B12 – It is essential for neuropathic pain management, pernicious anemia, with vitamin b complex deficiency pain, paresthesia, numbness, itching with diabetic neuropathy pain, myalgia, etc.
- Antidepressants – A drug that blocks pain messages from your brain and boosts the effects of endorphins (your body’s natural painkillers).
- Corticosteroid – to healing the nerve inflammation and clotted blood in the joints. Steroids may be prescribed to reduce the swelling and inflammation of the nerves. They are taken orally (as a Medrol dose pack) in a tapering dosage over a five-day period. It has the advantage of providing almost immediate pain relief within a 24-hour period.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation throughout the skin.
- Steroid injections The procedure is performed under x-ray fluoroscopy and involves an injection of corticosteroids and a numbing agent into the epidural space of the spine. The medicine is delivered next to the painful area to reduce the swelling and inflammation of the nerves (Fig. 3). About 50% of patients will notice relief after an epidural injection, although the results tend to be temporary. Repeat injections may be given to achieve the full effect. Duration of pain relief varies, lasting for weeks or years. Injections are done in conjunction with a physical therapy and/or home exercise program.
Surgery
- Microdiscectomy – for a herniated disc, a minimally-invasive procedure in which the herniated portion of the disc is removed.
- Artificial disc replacement – for degenerative disc disease and herniated discs is a minimally invasive procedure that replaces a damaged disc with a specialized implant that mimics the normal function of the disc, maintaining mobility.
- Spinal fusion – fusion for degenerative disc disease, in which the disc space is fused together to remove motion at the spinal segment. Spinal fusion involves setting up a bone graft, as well as possible implanted instruments, to facilitate bone growth across the facet joints. Fusion occurs after the surgery.
- Open Back Surgery – Traditionally, bulging discs are treated with an open back procedure, meaning the surgeon makes a large incision into the skin and cuts muscle and surrounding tissue to gain access to the problematic disc. This traditional surgical option is invasive, requires overnight hospitalization, general anesthesia, and requires a lengthy recovery coupled with strong pain medication.
- Endoscopic Surgery – Fortunately, you have a second option with endoscopic spine surgery. Thanks to the advancement of surgical technology at bulged disc surgery can be performed using endoscopic procedures, meaning the surgeon makes a small incision to insert special surgical tools. During an endoscopic bulging disc operation, the surgeon uses a tiny camera to visualize and gain access to your damaged disc. This minimally invasive new approach offers shorter recovery, easier rehabilitation, and a much higher success rate than open back or neck surgery. A local anesthetic is all that is usually required.
- Total Disc Replacement (TDR) and Anterior Cervical Discectomy and Fusion (ACDF) – Surgical exposure of the desired vertebral level is achieved through an anterior cervical incision. Subcutaneous dissection is performed to allow for adequate mobilization to tissue incision. The discectomy is performed with pituitary rongeurs, curette, and a burr drill to remove the affected disc. The posterior longitudinal ligament can be left in situ depending on the severity of the herniation. The center of the disc is identified. A keel is made using the burr after which the disc is removed and disc replacement performed. A similar surgical method is used for anterior cervical discectomy and fusion, the difference is the type of implant, which can be an interbody cage with an anterior cervical plate or a standalone cage. Although complications are rare, patients experience dysphagia, hoarseness, and transient sore throat. Adjacent segment disease or pseudoarthrosis can occur depending on severity and number of levels operated. The majority of patients get symptomatic relief and can resume full activity after six months.
- Laminectomy – Cervical laminectomy removes the lamina on one or both sides to increase the axial space available for the spinal cord. Clinically indicated for spinal stenosis or cervical disc disease involving more than three levels of disc degeneration with anterior spinal cord compression. Single-level cervical disc herniation is usually managed with the anterior approach. The complications of the posterior approach include instability resulting in kyphosis, recalcitrant myofascial pain, and occipital headaches.
- Laminoplasty – The kyphotic deformity is a well-known complication of laminectomy. To preserve the posterior wall of the spinal canal while decompressing the spinal canal a Z-plasty technique for the lamina was developed. The variant of the procedure uses a hinged door for the lamina. Laminoplasty is commonly indicated for multilevel spondylotic myelopathy. Nerve root injury is seen in about 11% of the surgeries. This complication is unique to laminoplasty, and the suggested etiology is traction on the nerve root with the posterior migration of the spinal cord.
Some patients will not benefit from conservative treatment and will require surgery to decompress the nerve involved. Classical surgical indications are motor deficit, cauda equina syndrome, and persistent pain after conservative treatment.[rx]
References






