Invasive mechanical ventilation (IMV) is an advanced airway modality used for individuals with immediate or impending respiratory failure and/or in preparation for surgery. The IMV technique involves positive pressure ventilation delivered to the lungs through an endotracheal tube via a ventilator. The ventilator can be set to specific modes that determine how the machine assists with breathing. The modes are tailored to the individual’s needs. The mode refers to the characteristics of mechanical ventilation and mainly includes trigger (how inspiration begins), cycle (how inspiration ends), and limit (when inspiration should be aborted). The most commonly used model is assist-control ventilation, which is usually followed by pressure-support ventilation for weaning.
Invasive mechanical ventilation (IMV) is a form of advanced airway management used to deliver oxygen and/or to regulate ventilation at the level of the trachea through 3 main routes:
- Oropharyngeal intubation
- Nasopharyngeal intubation
- Tracheostomy
Common indications for IMV
- Hypoxemia refractory to noninvasive oxygenation (e.g., ARDS)
- Hypercapnia with altered mental status (e.g., chronic obstructive pulmonary disease (COPD) exacerbation)
- GCS < 8 (e.g., cardiac arrest)
- Inability to protect the airway (e.g., anaphylaxis)
- Surgical procedures (e.g., neuromuscular blockade)
- Progressive neuromuscular disorders (e.g., amyotrophic lateral sclerosis (ALS))
Considerations
There are several modes of IMV that are managed jointly based on:
- Preferences of the intensivist
- Preferences of the respiratory therapist
- The individual’s needs
Invasive mechanical ventilation is not a benign intervention:
- Ventilator-induced lung injury (VILI) is common.
- VILI may compound the specific etiology of respiratory failure.
General Concepts
Background ventilation physiology
Ventilator mode is described based on 3 characteristics, namely, trigger, cycle, and limit:
- Trigger is the type of signal that initiates the inspiratory phase by the ventilator:
- Patient-triggered signal: The individual’s inspiratory effort triggers the inspiratory phase by the ventilator.
- Time-triggered signal: A time interval set by the operator determines when the ventilator initiates the inspiratory phase.
- Cycle: the type of signal that ends the inspiratory phase delivered by the ventilator
- Volume-cycled ventilation: The inspiratory phase ends once a preset volume exits the ventilator.
- Other types include:
- Time-cycled ventilation
- Pressure-cycled ventilation
- Limit: a value (e.g., pressure or time) that should not be exceeded and that is specified by the operator to protect the lungs
Basic settings controlled by the operator
- PEEP:
- Pressure remaining in the distal airways (i.e., the alveolus) of an individual at the end of expiration
- Keeps the alveoli open to participate in oxygenation
- Can be increased to improve oxygenation (↑ PaO₂)
- Can be lowered to decrease oxygenation (↓ PaO₂)
- FiO2 is the percentage of O₂ delivered directly to the individual:
- Increasing FiO2 increases oxygenation and decreasing FiO₂ lowers oxygenation.
- Tidal volume is the volume (in mL) delivered with each breath:
- Can be increased to increase ventilation (↓ PaCO₂)
- Can be lowered to reduce ventilation (↑ PaCO₂)
- Respiratory rate (RR) is the value set for breaths/min:
- Can be increased to increase ventilation (↓ PaCO₂)
- Can be lowered to reduce ventilation (↑ PaCO₂)
- Flow rate is the maximum flow (in L/min) that a ventilator can deliver a set tidal volume:
- Can be increased with a possible increase in ventilation effect (↓ PaCO₂)
- Can be lowered with a possible reduction in ventilation effect (↑ PaCO₂)
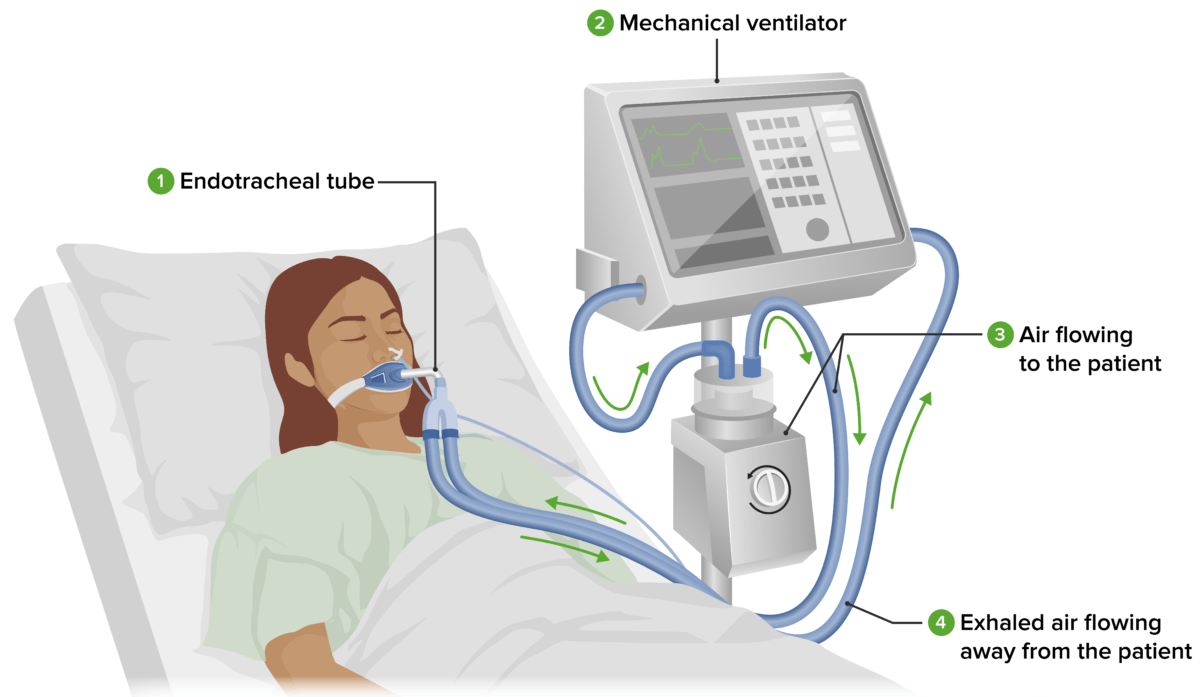
An endotracheal tube (or tracheostomy) (1) placed in the individual’s trachea is attached to the tubing of the mechanical ventilator (2). The mechanical ventilator delivers oxygenated air through tubes into the individual’s respiratory tract. Air flowing to the individual (3) passes through a humidifier, where it is warmed and moistened. Exhaled air flowing away from the individual (4) is returned to the ventilator. The nurse periodically checks the individual and ventilator.Image by Lecturio.
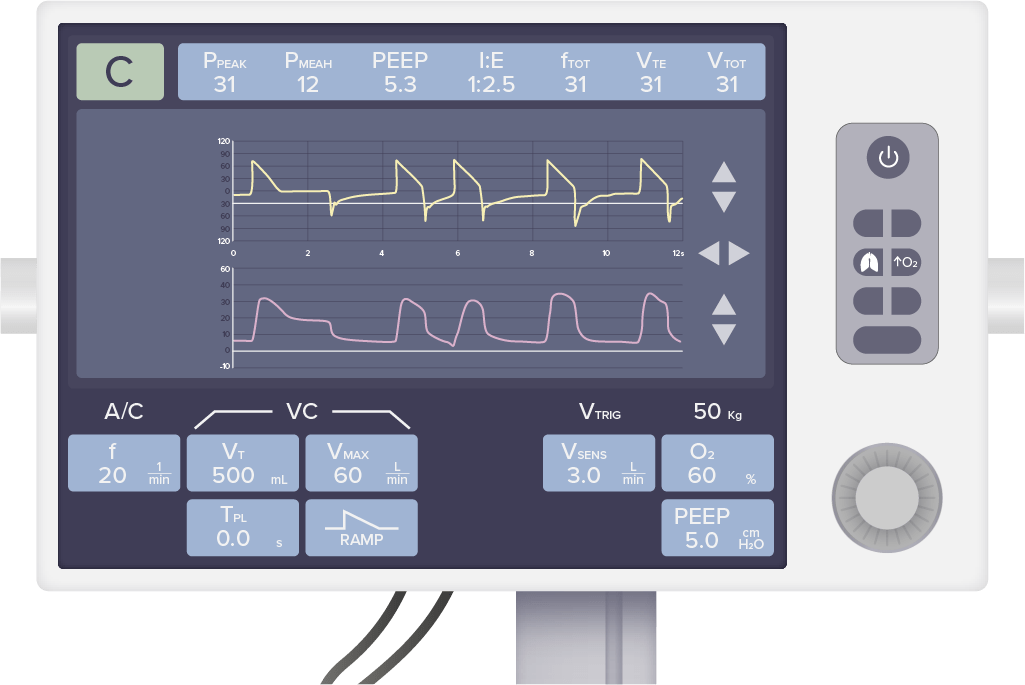
The top row of values displays respiratory parameters generated by the individual. The bottom row of values displays ventilator settings that can be manipulated by the operator depending on the clinical scenario and the needs of the individual.Image by Lecturio.
Common Modes
Controlled mode
- Commonly used in critically ill individuals who have a significantly suppressed or absent respiratory drive
- All spontaneous patient breaths sensed by the ventilator are assisted with a preset volume or pressure specified by the operator.
- Patient-/time-triggered and volume-/pressure-cycled modes
- The 2 most common modes are:
- Assist-control (AC) volume-control (VC) ventilation
- AC pressure-control (PC) ventilation
Spontaneous/supported mode
- Used after a significant improvement of the critical state of individuals who can breathe spontaneously and are being considered for weaning
- Patient-triggered and flow-cycled modes
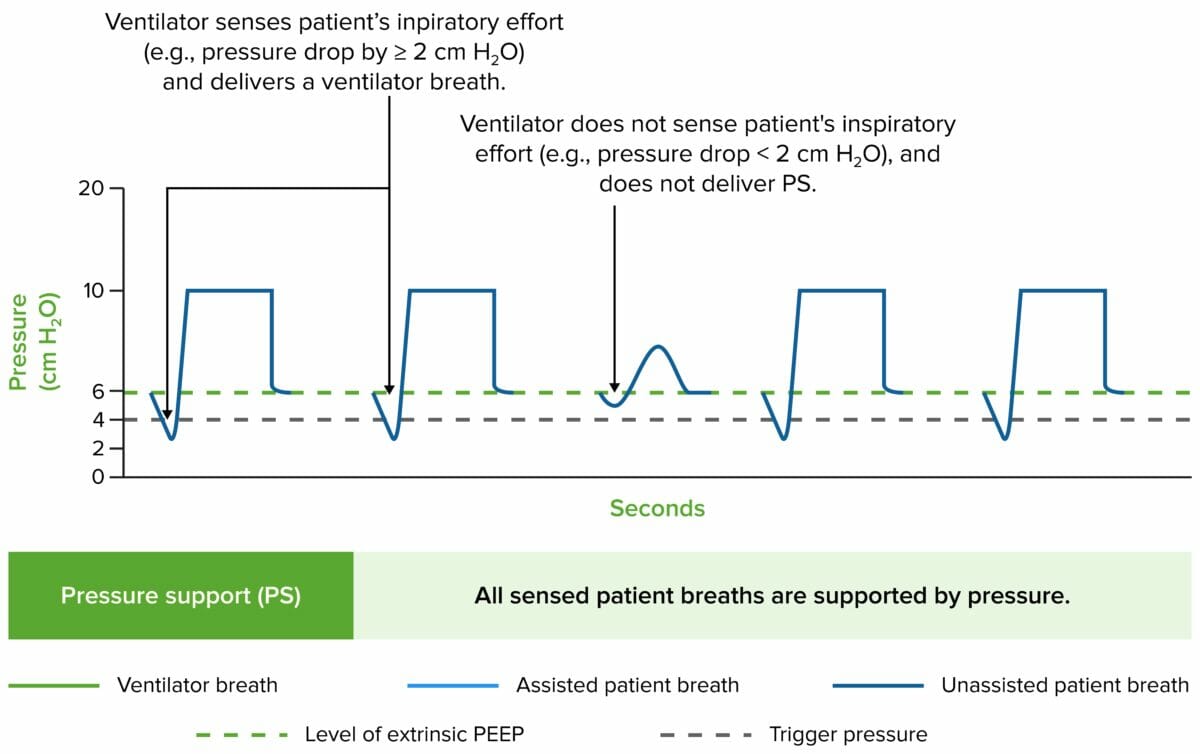
- Pressure-support (PS) ventilation is the most common: All spontaneous patient breaths sensed by the ventilator are supported with a preset pressure specified by the operator.
Combined (controlled + spontaneous/supported) mode
- Commonly used for individuals on maintenance ventilation and for weaning
- A preset number (not all) of patient breaths are assisted by the ventilator, as described for controlled mode; the remaining spontaneous patient breaths are supported as described for spontaneous/supported mode PS ventilation.
- Also known as synchronized intermittent mandatory ventilation (SIMV)
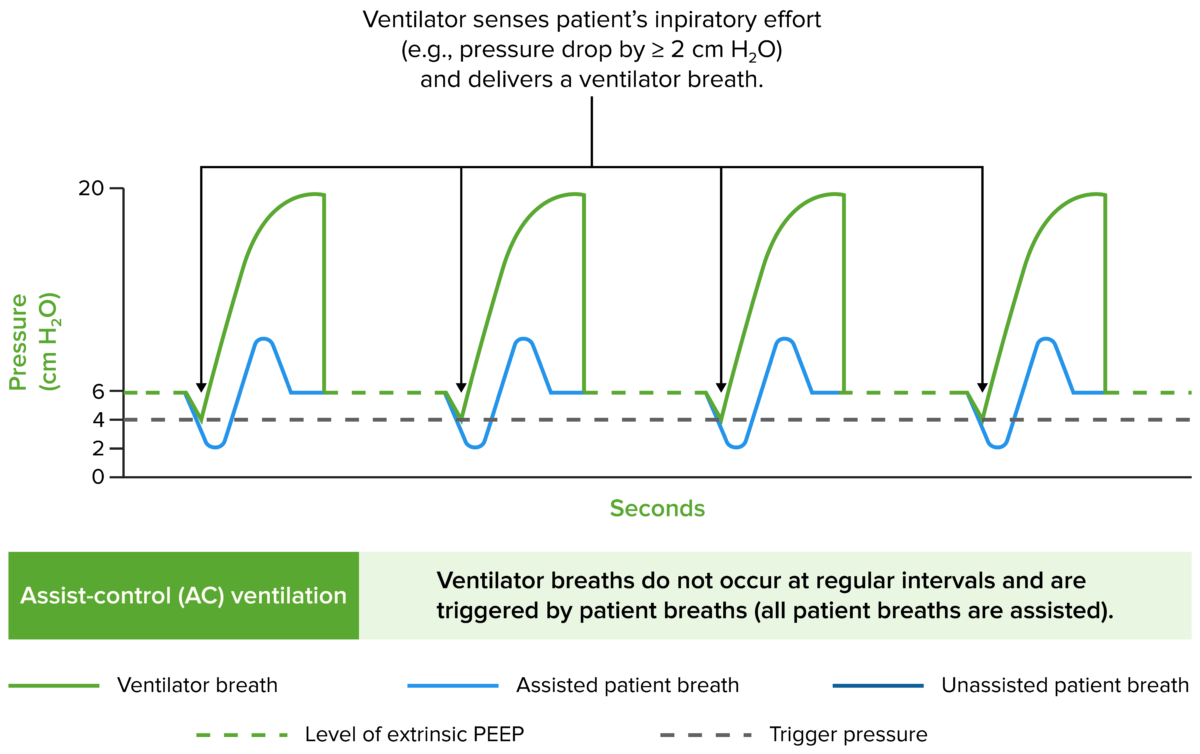
Assist-control volume-control ventilation
- Most commonly used initial mode of ventilation
- Assists every sensed inspiratory effort made by the individual, thereby reducing the work of breathing
- Trigger:
- Time triggered, if the individual’s inspiratory effort is not sensed: The ventilator delivers a preset number of mandatory breaths per minute.
- Patient triggered, if the individual’s inspiratory effort is sensed: All inspiratory efforts are assisted by the ventilator.
- Volume-cycled ventilation:
- Inspiratory phase ends when a preset volume exits the ventilator.
- Inspiratory volume is an independent variable because it is set by the operator and does not vary between breaths.
- Inspiratory pressure is a dependent variable because it is not set by the operator and varies between breaths.
- Pressure-limited ventilation:
- Preset by the ventilator to abort the inspiratory phase if dangerous levels of airway pressure are reached
- Helps prevent VILI
- Examples:
- In an individual on AC/VC ventilation who has spontaneous breaths of 20/min and with RR set at 20/min:
- All breaths are efficient enough to be sensed by the ventilator.
- All breaths are assisted immediately after patient initiation.
- Thus, the ventilator frequency is 20/min.
- If the individual’s spontaneous breaths increase to 30/min while on AC/VC:
- The ventilator frequency becomes 30/min.
- The additional 10 breaths are assisted by the ventilator.
- An individual has 4 spontaneous breaths/minute on AC/VC while the RR is set at 12/min:
- The ventilator assists with 4 breaths of the individual.
- The ventilator adds 8 breaths every minute to reach the minimum number set by the operator.
- In an individual on AC/VC ventilation who has spontaneous breaths of 20/min and with RR set at 20/min:
- Problems:
- Respiratory alkalemia in individuals with tachypnea due to anxiety, pain, or airway irritation
- Auto-PEEP: dynamic hyperinflation of lungs when air builds up due to insufficient expiratory time
Assist-control pressure-control ventilation
- Appropriate when the control of peak airway pressures is important (i.e., consider for individuals with previous barotrauma or after thoracic surgery)
- Time-triggered, time-cycled, and pressure-limited ventilation
- Inspiratory pressure is an independent variable because it is set by the operator and does not vary between breaths.
- Inspiratory volume is a dependent variable because it is not set by the operator and varies between breaths:
- Increasing volume at constant settings reflects improved pulmonary compliance.
- Decreasing volume at constant settings reflects worsening pulmonary compliance.
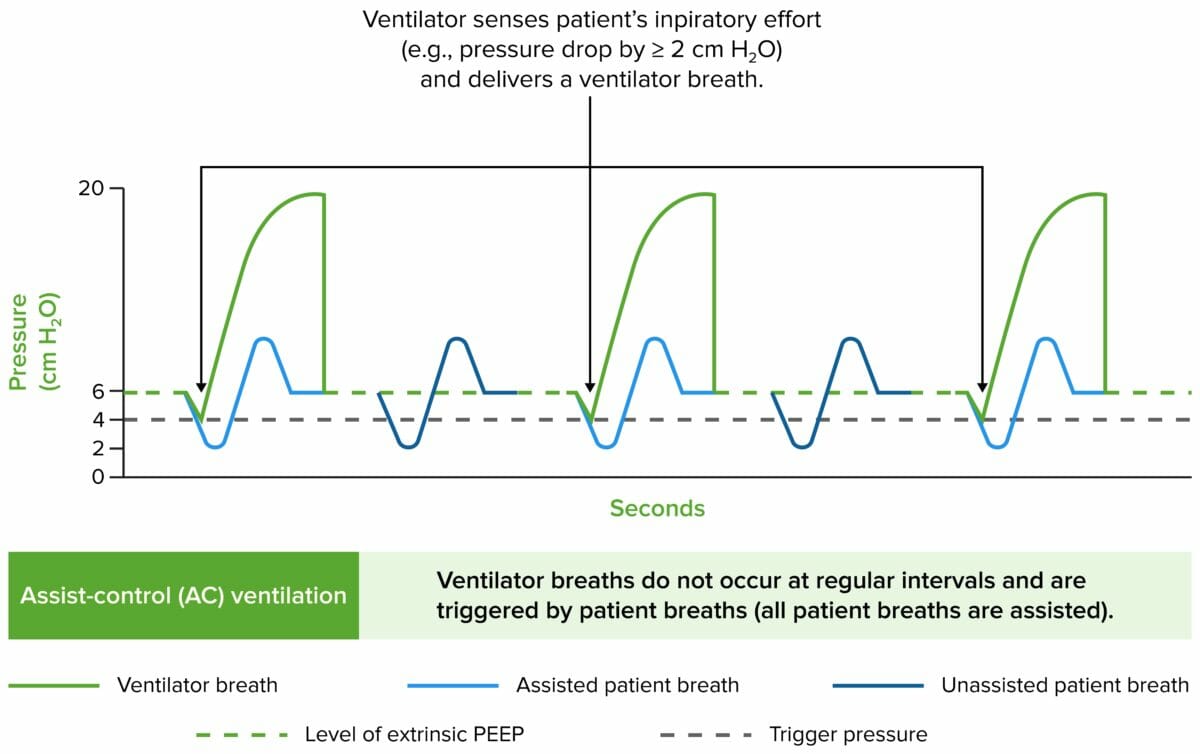
Synchronized intermittent mechanical ventilation/VC ventilation
- More commonly used in surgical ICUs as opposed to medical ICUs
- Previously thought to be best for weaning individuals off the ventilator
- Allows the individual to practice unassisted breathing between assisted synchronized mandatory breaths
- Trigger:
- Patient-triggered process if the individual’s inspiratory effort is sensed:
- Some of the sensed inspiratory efforts are assisted by the ventilator.
- Number of assisted breaths/minute is determined by the operator.
- Patient breaths in excess of the operator’s settings remain unassisted.
- Time-triggered process if the individual’s inspiratory effort is not sensed: The ventilator delivers a preset number of mandatory breaths/minute.
- Patient-triggered process if the individual’s inspiratory effort is sensed:
- Volume-cycled ventilation:
- Inspiratory phase ends when a preset volume exits the ventilator.
- Inspiratory volume is an independent variable because it is set by the operator and does not vary between breaths.
- Inspiratory pressure is a dependent variable because it is not set by the operator and varies between breaths.
- Pressure-limited ventilation:
- Preset by the ventilator to abort the inspiratory phase if dangerous levels of airway pressure are reached
- Helps prevent VILI
- Example for SIMV mode:
- An individual has 20 spontaneous breaths while intubated, and the ventilator frequency is set to 12/min.
- The ventilator delivers each of the 12 mandatory breaths in a synchronized fashion when the individual initiates a spontaneous breath.
- Of the individual’s total 20 spontaneous breaths/minute, 12 are assisted by the ventilator and 8 remain unassisted.
- The total number of breaths remains 20/min.
- Problems:
- Reduced minute ventilation:
- When tachypneic, the individual exhales during the ventilator inspiratory phase.
- Causes a rapid rise in airway pressure beyond the pressure limits set by the operator
- Will lead to premature cessation of ventilator-delivered breaths
- A switch to AC ventilation mode would increase the number of assisted breaths and minute ventilation.
- SIMV is usually delivered in combination with PS ventilation to support unassisted breaths with a preset pressure.
- Reduced minute ventilation:
Pressure-support ventilation
- Commonly used in combination with SIMV to ensure volume-cycled backup.
- Patient-triggered, flow-cycled, pressure-limited ventilation
- Operator sets the pressure that must be reached during each inspiratory phase by the ventilator.
- PS ventilation is always patient triggered: All sensed inspiratory efforts are supported by the ventilator to reach the pressure set by the operator.
- Once the flow in the airway reaches a level below a minimum threshold, the PS is terminated.
Complications
Ventilator-associated pneumonia (VAP)
- Requires a minimum of 3 days on mechanical ventilation
- Risk factors:
- Advanced age
- Higher degree of comorbidities
- Prolonged length of hospital/ICU stay
- Prolonged length of IMV
- Exposure to invasive procedures
- Typically diagnosed via imaging along with:
- Increased respiratory secretions
- Culture data (bronchoalveolar lavage or tracheal aspirate)
- Presence of sepsis (worsening or new)
- Most common organisms:
- Staphylococcus aureus
- Pseudomonas aeruginosa
- Klebsiella pneumoniae
- Enterobacter species
- Actinobacter species
- Treatment is with antibiotics.
Subtypes of VILI
- Barotrauma:
- High lung inflation pressure that results in:
- High transpulmonary pressure
- Lung overdistension
- Air leakage
- High lung inflation pressure that results in:
- Atelectrauma: high shear forces that open and close recruitable atelectatic lung units
- Volutrauma:
- Alveolar overdistension causing epithelial strain and lipid mobilization
- Lipid mobilization causes cellular detachment of vascular endothelial cells:
- Alveolar epithelium breaks down.
- Results in alveolar and interstitial edema
- Biotrauma: inflammatory response from mechanical injury via cytokines and other inflammatory mediators
- Practices preventing VILI include:
- Low tidal volumes
- Moderate amount of PEEP
- Prone positioning
- Neuromuscular blocking agents to prevent patient/ventilator dyssynchrony
Oxygen toxicity
- Results from reactive O₂ species that cause:
- Cellular damage
- Inflammation
- Genetic alterations
- To avoid toxicity, it is recommended to use the lowest FiO₂ to achieve targeted oxygenation.
Auto-PEEP
- Results of persistent end-expiratory airflow that compounds after each breath, contributing to increasing pulmonary hyperinflation
- Also known as “air stacking” or “intrinsic PEEP”
- Most commonly seen in asthma, COPD, and ARDS
- Results in alveolar overdistension and reduced lung compliance (barotrauma)
- Increases intrathoracic pressure
- Increases in intrathoracic pressure can result in:
- Decreased venous return
- Reduced cardiac preload
- Increased left ventricular afterload
- Reduced cardiac output leading to hypotension
- Suspect when the individual has:
- Patient/ventilator dyssynchrony
- Pulsus paradoxus
- Hypoxia
- High plateau pressure
- Hypotension
- Therapeutic interventions depend on the ventilator mode, but include:
- Lowering PEEP
- Reducing inspiratory time to allow more expiratory time
- Reducing respiratory rate
- Disconnecting from the ventilator and pressing down on the chest briefly
- Hemodynamic support for hypotension, if needed
Peptic ulcers
- Common in mechanically ventilated individuals becasue of gastric colonization
- Can be associated with upper GI bleeding
- Prevention strategies (note: may increase the risk of VAP):
- Histamine-2 receptor antagonist
- Proton pump inhibitors
Ventilator bundles
Commonly used to prevent ventilator-associated complications.
- 30–45 degrees head-of-bed elevation and semirecumbent position: reduces the risk of gastric reflux, aspiration, and VAP
- General infection-control measures (vary by hospital)
- Peptic ulcer prophylaxis
- Deep venous thrombosis prophylaxis
- Daily spontaneous breathing trials
- Spontaneous awakening trials/periodic interruption of sedation
- Maintenance of endotracheal cuff pressure between 20 and 30 cm H₂O
- Frequent subglottic suctions
- Oral care with chlorhexidine gluconate
- Pressure care for wound prevention
- Early mobilization
Weaning and Extubation
Approach to weaning
- Ventilator weaning should be approached based on the following metrics:
- Has the underlying issue been addressed and improved?
- Is the individual headed toward hemodynamic stability?
- Is the O₂ saturation consistently improving?
- Is the individual able to breathe comfortably on minimal ventilator settings?
- If all the above questions are answered affirmatively, it may be time to start a spontaneous breathing trial (SBT).
Spontaneous breathing trial
An SBT consists of minimal ventilator settings that can be used to predict the chances of successful extubation.
- PS ventilation with:
- PS of 8–5 cm H₂O
- PEEP of 5–0 cm H₂O
- FiO₂ < 40%
- T-piece trial:
- Use of an adapter piece that disconnects the individual from the ventilator
- Allows the endotracheal tube to remain in place
- Should be trialed from 30–120 minutes on these minimal settings
- Sedation should be weaned off or set at minimum prior to SBT (exception is during dexmedetomidine use, as it does not suppress respiratory drive).
When to consider extubation
- Improvement in original cause of respiratory distress or when limited airway protection is required
- No severe tachypnea or apneic episodes
- SpO₂ > 92%
- Tidal volumes consistently > 325 mL
- No tachycardia
- Normotensive
- Mental status: capable of following 1-step commands
- Cuff leak (checks for subglottic edema)
- Minimal secretions
- Plan for the day (consider waiting after procedures or imaging studies).
- Rapid shallow breathing index:
- Respiratory rate/tidal volume < 105
- Most reliable predictor
Post-extubation considerations
When extubating, consider trialing higher levels of supplemental O₂:
- High-flow nasal cannula in individuals with hypoxic respiratory failure (ARDS)
- BiPAP in hypertensive individuals with left heart failure or mitral regurgitation




 Shop From Rxharun..
About Us...
Editorial Board Members..
Developers Team...
Team Rxharun.
Shop From Rxharun..
About Us...
Editorial Board Members..
Developers Team...
Team Rxharun.