Scoliosis is a spinal deformity consisting of lateral curvature and rotation of the vertebrae. Scoliosis is defined as a deviation of the normal vertical line of the spine, consisting of a lateral curvature with rotation of the vertebrae within the curve. Typically, for scoliosis to be considered, there should be at least 10° of spinal angulation on the posterior-anterior radiograph associated with vertebral rotation (rx).The causes of scoliosis vary and are classified broadly as congenital, neuromuscular, syndrome-related, idiopathic and spinal curvature due to secondary reasons. Congenital scoliosis is due to a vertebral abnormality causing the mechanical deviation of the normal spinal alignment. Scoliosis can be due to neurological conditions (eg, cerebral palsy or paralysis), muscular abnormalities (eg, Duchenne muscular dystrophy) or other syndromes (eg, Marfan syndrome and neurofibromatosis). Occasionally, significant lateral deviation of the spine can occur with little or no rotation of the spine and without bony abnormalities. In these cases, the ‘scoliosis’ can be the result of pain, spinal cord abnormalities, tumors (both intraspinal and extraspinal) and infection.
Scoliosis is a spinal disorder where the spine curves sideways in an “S” or “C” shape rather than remaining straight. This curvature can vary in degree and may affect body symmetry, posture, and sometimes lead to discomfort or pain. Scoliosis is most common in children and adolescents, although it can affect adults as well.
Medical literature often has more specific names or terms for scoliosis:
- Kyphoscoliosis: a combination of outward and lateral spine curvature
- Dextroscoliosis: the curvature of the spine to the right
- Rotoscoliosis (rotatory): the curvature of the vertebral column turned on its axis
- Levoconvex: the curvature of the spine to the left
- Thoracolumbar: curvature related to both the thoracic and lumbar regions of the spine
- Scoliosis can be classified into several types based on the cause and age of onset:
-
Idiopathic Scoliosis:
The most common type, especially in adolescents. Its cause is unknown but may have a genetic component.-
Adolescent Idiopathic Scoliosis (AIS): Occurs during the growth spurt just before puberty.
-
Adult Idiopathic Scoliosis: May continue from adolescent cases or develop later in life.
-
-
Congenital Scoliosis:
Develops from abnormalities in the vertebrae at birth due to improper spinal formation. -
Neuromuscular Scoliosis:
Occurs in individuals with neuromuscular conditions such as cerebral palsy, muscular dystrophy, or spinal muscular atrophy. -
Degenerative Scoliosis (or Adult Scoliosis):
Associated with aging changes in the spine, including disc degeneration and arthritis. -
Syndromic Scoliosis:
Associated with specific syndromes such as Marfan syndrome or Ehlers-Danlos syndrome.
-
As stated above, idiopathic scoliosis and its subtypes comprise over 80% of all scoliosis patients. However, there are three other main types of scoliosis:
- Functional: In this type of scoliosis, the spine is normal, but an abnormal curve develops because of a problem somewhere else in the body. This could be caused by one leg being shorter than the other, carrying heavy loads that cause unequal weight-bearing, or by muscle spasms in the back.
- Neuromuscular: In this type of scoliosis, there is a problem when the bones of the spine are formed. Either the bones of the spine fail to form completely or they fail to separate from each other during fetal development. This type of congenital scoliosis develops in people with other disorders, including birth defects, muscular dystrophy, cerebral palsy, or Marfan syndrome (an inherited connective tissue disease). People with these conditions often develop a long C-shaped curve and have weak muscles that are unable to hold them up straight. If the curve is present at birth, it is called congenital scoliosis. This type of scoliosis is often much more severe (severe scoliosis) and needs more aggressive treatment than other forms of scoliosis.
- Degenerative: Unlike the other forms of scoliosis that are found in children and teens, degenerative scoliosis occurs in older adults. It is caused by changes in the spine due to arthritis known as spondylosis. Weakening of the normal ligaments and other soft tissues of the spine combined with abnormal bone spurs can lead to an abnormal curvature of the spine. The spine can also be affected by osteoporosis, vertebral compression fractures, and disc degeneration.
There are other potential causes of scoliosis, including spine tumors such as osteoid osteoma. This is a benign tumor that can occur in the spine and cause pain. The pain causes people to lean to the opposite side to reduce the amount of pressure applied to the tumor. This can lead to a spinal deformity. In addition, researchers suggest that genetics (hereditary), muscle disorders, and/or abnormal fibrillin metabolism may play a role in causing or contributing to scoliosis development.
Types over all
There are many ways to group scoliosis. Below are the main types, explained in simple words.
-
Idiopathic scoliosis
Idiopathic means “cause not known.” This is the most common type, especially in healthy children and teenagers. The spine slowly curves as the child grows, usually between 10 and 18 years of age. Doctors think genes, growth, and hormones may all play a role, but no single clear cause is found. -
Infantile idiopathic scoliosis
This type appears in babies and very young children, usually under age 3. The curve can sometimes improve on its own as the child grows, but some children need close follow-up or treatment to stop the curve getting worse. -
Juvenile idiopathic scoliosis
This type starts roughly between 4 and 9 years of age. Because children still have many years of growth ahead, the curve can slowly become larger if doctors do not watch and treat it in time. -
Adolescent idiopathic scoliosis (AIS)
AIS begins in the teenage years and is the classic form many people think about when they hear “scoliosis.” It often shows up during a growth spurt. Girls are affected more often than boys, and curves may progress quickly when growth is fast. -
Adult idiopathic scoliosis
Some teenagers with scoliosis are not treated or their curve remains mild and stable. As they become adults, the same curve is still present and may slowly cause back pain, stiffness, or posture problems. This is called adult idiopathic scoliosis. -
Adult degenerative (de-novo) scoliosis
In this type the spine is straight in youth, but later in adult life the discs and joints wear out unevenly. This uneven wear causes the spine to tilt and twist, making a new curve appear. It is often linked with arthritis, osteoporosis, and spinal stenosis. -
Congenital scoliosis
Here the scoliosis is present from birth because the vertebrae (spinal bones) did not form normally in the womb. Some bones may be half-formed or fused together. These structural problems create a fixed curve that often worsens as the child grows. -
Neuromuscular scoliosis
Neuromuscular scoliosis happens when muscles cannot support the spine properly because of nerve or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida. Weak or unbalanced muscles let gravity pull the spine into a curve, often severe. -
Syndromic scoliosis
This type is part of a wider syndrome, such as Marfan syndrome, Ehlers-Danlos syndrome, neurofibromatosis, or other connective tissue and genetic disorders. The curve is only one piece of a bigger picture, so doctors must also manage the other health issues. -
Functional or postural scoliosis
In functional scoliosis the bones of the spine are normal. The curve happens because of something outside the spine, such as one leg being shorter or a painful muscle spasm. When the cause is corrected, the curve often becomes smaller or disappears.
Causes of scoliosis
-
Genetic factors and family history
Many people with idiopathic scoliosis have a close relative with a similar curve, which suggests that certain genes raise the risk. Research has found several gene regions linked with adolescent idiopathic scoliosis, although no single “scoliosis gene” explains all cases. -
Abnormal vertebral formation before birth
In congenital scoliosis, some vertebrae are wedge-shaped, half-formed, or fused. These errors in bone formation happen early in pregnancy and cause an uneven spine from the start of life, which then curves more as the child grows. -
Abnormal vertebral segmentation
Sometimes the problem is not how the vertebrae form but how they separate. If several vertebrae fail to separate properly, they can stay joined or “blocked.” This block pulls the spine sideways and leads to a stiff curve that does not correct when bending. -
Neuromuscular diseases (cerebral palsy, muscular dystrophy)
Conditions that weaken or paralyze muscles around the spine make it difficult to sit or stand straight. Over time the spine bends toward the weaker side, creating neuromuscular scoliosis that may progress rapidly and affect sitting balance and lung function. -
Spina bifida and spinal cord defects
In spina bifida and some spinal cord malformations, the nerves that control trunk muscles do not work normally. This imbalance in muscle control around the spine lets it curve and twist, often together with hip and leg deformities. -
Connective tissue disorders (Marfan, Ehlers-Danlos)
In these conditions the tissues that hold joints and ligaments firm are too stretchy or weak. The spine, which depends on ligaments and discs for support, may gradually bend and rotate because it is not held straight as strongly as in a healthy person. -
Neurofibromatosis and spinal tumors
Tumors along the spine or in the nerves, as seen in neurofibromatosis, can weaken one side of the vertebrae or cause pain and muscle spasm. This uneven support and tension can pull the spine into a curve and may make an existing spinal deformity worse. -
Leg length discrepancy
When one leg is shorter than the other, the pelvis tilts. To keep the eyes level and stay balanced, the spine curves sideways. Over time a small functional curve can become more permanent if the difference is large and not corrected with shoe lifts or treatment. -
Muscle imbalance or weakness around the spine
Weak core and back muscles, or strong muscles on one side and weak on the other, can gradually pull the spine sideways. This situation is more common in people with long-term neuromuscular problems or poor posture habits. -
Degenerative disc and facet joint disease
In older adults, wear and tear of discs and facet joints can happen more on one side than the other. The spine then tilts and rotates around these damaged segments, leading to adult degenerative scoliosis with pain and stiffness. -
Osteoporosis and vertebral fractures
Thin, fragile bones are more likely to collapse or break. If several vertebrae on one side crumble, the column loses its straight support and bends sideways. This process can create or worsen scoliosis in older adults, especially women after menopause. -
Previous spine surgery or structural loss
Surgery that removes bone, disc, or part of a vertebra on one side, or scarring that pulls unevenly, can change the way forces pass through the spine. Over years this imbalance may lead to a new curve near the operated area. -
Spinal infections and inflammatory disease
Infections such as vertebral osteomyelitis or spinal tuberculosis can damage one part of a vertebra more than another. Inflammatory diseases like ankylosing spondylitis can also deform the spine and change its alignment, sometimes causing secondary scoliosis. -
Metabolic bone disease (rickets, vitamin D deficiency)
Poor mineralization of bone makes vertebrae soft and easily deformed. If the weight of the body presses unevenly because of posture or muscle imbalance, the spine may bend into a curve as it tries to support the head and trunk. -
Rapid growth during puberty
In adolescents, the spine lengthens quickly. If mild imbalance or genetic susceptibility is present, this rapid growth phase can allow a small curve to grow larger in a short time, especially in girls during their teenage years. -
Abnormal posture and carrying habits
Although simple bad posture alone usually does not cause true structural scoliosis, long-term leaning to one side, carrying heavy loads on one shoulder, or sitting crooked can create functional curves that stress the spine and may contribute to pain and mild deformity. -
Syndromes with chest and abdominal deformity
Some syndromes that involve the ribs, chest, or abdominal wall also change the way the spine grows. When ribs are fused or the chest is narrow, the vertebrae may twist and bend to fit the limited space, creating complex scoliosis. -
Tethered spinal cord and syringomyelia
Conditions where the spinal cord is stuck (tethered) or has a fluid-filled cavity (syrinx) can damage nerve pathways that control trunk muscles. This nerve damage leads to imbalance and neuromuscular scoliosis, often with pain or neurological signs. -
Trauma and spinal injury
Accidents that fracture or dislocate vertebrae can heal in a crooked position. When healing is uneven, the spine may be permanently tilted, and later degeneration around the injured area can increase the curve. -
Idiopathic (unknown) causes
Even after careful tests, in many people no clear cause is found. These idiopathic cases likely arise from a mix of genes, growth patterns, and subtle muscle or balance issues that scientists are still studying.
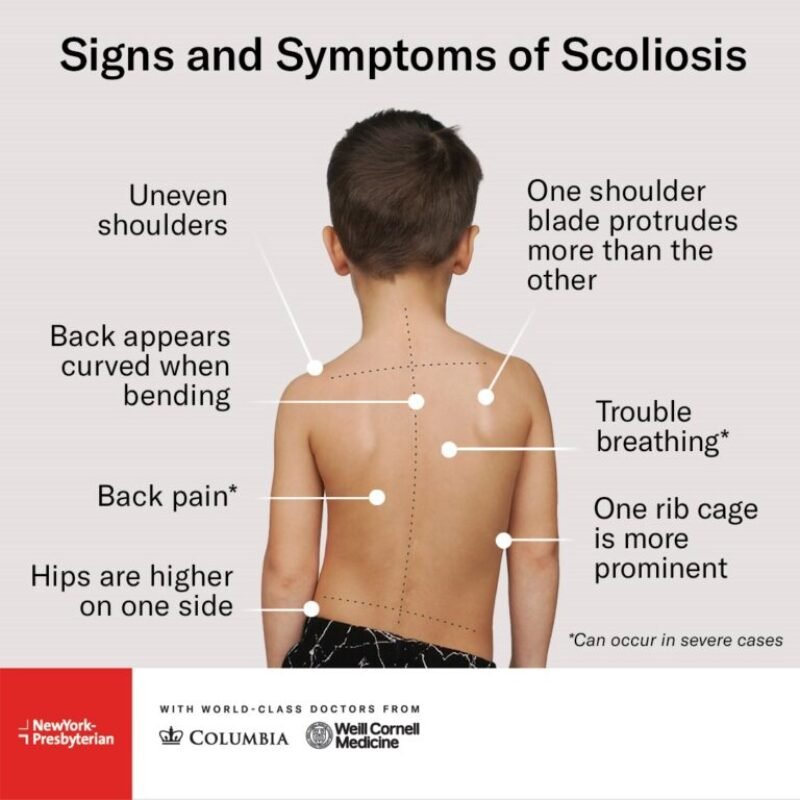
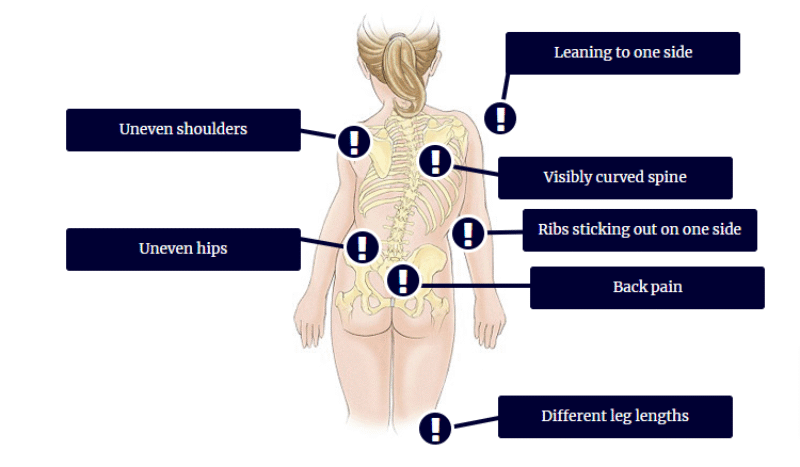
Symptoms of scoliosis
-
Uneven shoulders
One shoulder may look higher than the other when standing. Clothes can slide off one shoulder more easily, and photographs from behind often show this difference clearly. This is one of the earliest signs parents or friends may notice. -
One shoulder blade sticking out
The shoulder blade on the curved side may look more prominent or “sticking out.” This happens because the spine not only bends but also rotates, pushing the rib cage and shoulder blade backward. -
Uneven waist or hips
One side of the waist may have a deeper curve, and one hip may appear higher or more pushed out. Pants or skirts can seem to hang crooked even when they are worn correctly. -
Leaning to one side
The person may seem to lean or tilt to one side when standing or walking. They might feel as if they always stand “crooked,” even if they try to straighten up. -
Rib hump on bending forward
When bending forward, one side of the back or ribs may rise higher than the other, forming a “hump.” This is because the rotated spine carries the ribs with it, a typical sign seen in the Adams forward bend test. -
Back pain or aching
Many children have little pain, but teenagers and adults with scoliosis can feel aching or sharp pain in the back, especially after long periods of sitting or standing. Muscles and joints on the curved side may be overworked. -
Fatigue in back muscles
Because the spine is not aligned, back and core muscles must work harder to keep the body upright. This can lead to early tiredness, stiffness, or muscle spasms, especially later in the day. -
Reduced flexibility or stiffness
People with scoliosis may find it harder to bend, twist, or move the trunk smoothly. Tight muscles and joint changes around the curve can limit movement and make certain activities uncomfortable. -
Difference in leg length feeling
Even if the legs are the same length, the pelvic tilt from scoliosis can make it feel like one leg is longer. People may complain that one foot hits the ground more heavily or that they need a shoe insert. -
Clothes not hanging straight
Shirts, dresses, or jackets may twist to one side or look uneven at the hemline. This practical sign often alerts families that something is wrong with alignment. -
Shortness of breath in severe curves
Large curves in the chest (thoracic) area can reduce the space for the lungs to expand. In serious cases this can cause breathlessness on exertion, poor exercise tolerance, or feelings of tightness in the chest. -
Chest pain or rib discomfort
Misalignment of the ribs can lead to local pain, pressure, or tenderness around the chest wall. The rib cage can press against muscles and nerves, causing aching or sharp pains. -
Numbness, tingling, or weakness in limbs
If the curve narrows the spinal canal or nerve openings, nerves going to the arms or legs can be compressed. This may cause tingling, burning, numbness, or weakness, especially in adults with degenerative scoliosis. -
Head not centered over pelvis
In more advanced scoliosis, the head may not line up over the midline of the pelvis. This imbalance can be seen from behind and may cause a feeling of instability or poor balance. -
Low self-esteem or body image concerns
Visible deformity, posture changes, and the need for braces or surgery can affect how people, especially teenagers, feel about their body. They may feel shy, anxious, or depressed because of the appearance of their back.
Diagnostic tests for scoliosis
Physical exam tests
-
General posture and alignment inspection
The doctor first looks at the person standing from behind, from the side, and from the front. They check if the shoulders, hips, and waist are level, and whether the spine looks straight or curved. This simple visual check helps decide if further tests are needed. -
Gait (walking) assessment
The person is asked to walk normally. The doctor looks for limping, uneven steps, body leaning, or arm swing differences. Abnormal gait can suggest leg length difference, muscle weakness, or nerve problems that may be linked with scoliosis. -
Adams forward bend test
In this classic test, the person bends forward with arms hanging and knees straight. The examiner looks along the spine for a rib hump or muscle bulge on one side. A visible hump strongly suggests structural scoliosis rather than simple bad posture. -
Neurological examination
Doctors test muscle strength, reflexes, sensation, and balance. They also look for signs like abnormal reflexes, spasticity, or foot deformities. These findings can point to underlying spinal cord or nerve disease that may be causing a secondary scoliosis. -
Respiratory and cardiovascular assessment
In moderate to severe curves, especially in the chest region, doctors listen to the lungs and heart, and may measure breathing capacity. They look for signs that the spinal deformity is affecting lung expansion or heart function.
Manual tests
-
Scoliometer measurement during forward bend
A scoliometer is a small device placed on the back while the person bends forward. It measures the angle of trunk rotation. If this angle is above a certain value, it suggests a significant curve and the need for X-rays and specialist review. -
Leg length measurement
Using a tape measure or visual landmarks, the examiner compares the length of both legs. A real leg length difference can cause functional scoliosis, so identifying and correcting it is important to reduce the curve and prevent pain. -
Pelvic tilt and hip range of motion tests
The doctor feels the top of the hip bones and checks whether the pelvis is level, then moves the hips through their range of motion. Limited or uneven hip movement can contribute to abnormal posture and must be considered when planning treatment. -
Spinal flexibility and side-bending tests
By gently bending the spine sideways, forward, and backward, the examiner checks how flexible the curve is. A flexible curve can often be improved with bracing and exercises, while a very stiff curve may need surgical correction. -
Manual muscle testing of trunk and limbs
The doctor or therapist asks the person to push or pull against resistance with different muscle groups, especially around the trunk and hips. Weakness or imbalance helps identify neuromuscular causes of scoliosis and guides rehabilitation programs.
Lab and pathological tests
-
Complete blood count (CBC)
A CBC checks red and white blood cells and platelets. While it does not diagnose scoliosis itself, it helps rule out infection, anemia, or blood disorders, and is important before surgery or when a systemic disease is suspected along with scoliosis. -
Inflammatory markers (ESR, CRP)
Blood tests like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) rise in infection or active inflammation. If a child has scoliosis with fever or severe pain, these tests help search for underlying spinal infection or inflammatory disease. -
Calcium, phosphate, and vitamin D levels
These tests look for metabolic bone disease such as rickets or severe vitamin D deficiency. Weak, poorly mineralized bones can deform more easily, so correcting these problems is important in managing scoliosis in growing children. -
Genetic and syndromic testing
When scoliosis appears with other signs like very tall stature, hyperflexible joints, skin spots, or heart problems, doctors may order genetic tests for syndromes such as Marfan or neurofibromatosis. Finding the specific syndrome guides both treatment and family counselling.
Electrodiagnostic tests
-
Nerve conduction studies (NCS)
NCS measure how fast and how well nerves carry electrical signals. In scoliosis with numbness, tingling, or weakness, NCS can show whether peripheral nerves are damaged or compressed, helping separate spinal nerve problems from other nerve diseases. -
Electromyography (EMG)
EMG uses a fine needle to record electrical activity directly from muscles. It helps doctors see if weakness or wasting is due to nerve damage, muscle disease, or spinal cord problems. EMG is especially useful in neuromuscular scoliosis and adults with radiculopathy. -
Somatosensory evoked potentials (SSEPs)
SSEPs record how signals travel through the sensory pathways of the spinal cord and brain after small electrical stimulation. They are used in some complex scoliosis cases and during surgery to make sure the spinal cord is functioning safely. -
Motor evoked potentials (MEPs)
MEPs check how well movement signals travel from the brain down the spinal cord to the muscles. Like SSEPs, they are often used during scoliosis surgery in high-risk curves to monitor spinal cord health and reduce the chance of nerve injury.
Imaging tests
-
Standing spinal X-rays with Cobb angle measurement
X-rays taken while the person stands show the full spine from neck to pelvis. Doctors measure the Cobb angle, which is the standard way to quantify how large the curve is. These images are essential for diagnosis, follow-up, and treatment planning. -
MRI, CT, and low-dose EOS imaging
MRI scans show the spinal cord, discs, and soft tissues, and are used when there are “red flag” symptoms like severe pain or nerve signs. CT scans give detailed images of bone, useful in complex congenital curves. EOS is a special low-dose 3D X-ray system that allows full-body images with less radiation, helpful for repeated follow-up in children.
Non-Pharmacological Treatments for Scoliosis
-
Observation and regular checkups
For small curves, doctors often choose “watchful waiting.” They examine you, check your height and growth, and repeat X-rays every few months to see if the curve is stable or getting worse. This can avoid unnecessary treatment while still catching curves that suddenly grow during puberty. -
Scoliosis-specific physiotherapy (Schroth and similar methods)
Special 3-D exercises are designed just for scoliosis. Therapists teach breathing, muscle-strengthening, and posture drills to try to de-rotate and lengthen the spine. These programs may improve posture, reduce pain, and sometimes slow curve progression when used together with bracing. -
General core-strengthening exercises
Strong belly, back, and hip muscles help support the curved spine like a natural brace. Simple supervised exercises such as planks, gentle back extensions, and hip strengthening can improve stability, balance, and confidence, even though they do not “straighten” the bones themselves. -
Stretching and flexibility training
Curves often make one side of the trunk tight and the other side weak. Regular stretching of hamstrings, hip flexors, and chest muscles can reduce stiffness and improve movement. Better flexibility may help with daily activities and make it easier to stand and sit in a healthier posture. -
Posture training and body awareness
Many teenagers do not notice that they lean to one side or drop one shoulder. Therapists use mirrors, tape on the skin, or simple cues to teach self-correction. Learning how to sit, stand, study, and use screens with better alignment can reduce fatigue and back strain. -
Bracing (day-time braces)
For growing children with moderate curves, a custom plastic brace is often the main non-surgical treatment. The brace fits tightly around the chest, waist, and hips and is worn for many hours each day. Its goal is not to straighten the curve permanently but to stop it from getting worse while the child grows. -
Night-time bending braces
Some patients use special braces mainly at night. These braces push the spine in the opposite direction of the curve while you sleep. They are less visible during the day, which can help with comfort and self-esteem, but are usually most useful in selected curve patterns and must be chosen carefully by specialists. -
Activity modification and back-care education
Doctors and therapists often teach ways to protect the spine in daily life, such as avoiding repeated heavy lifting, changing study posture, and using both shoulder straps on a backpack. These simple changes cannot cure scoliosis but can reduce muscle strain and pain around the curve. -
Manual therapy and spinal mobilization
Some physiotherapists and other professionals gently move and stretch the joints and soft tissues around the spine. This may temporarily improve mobility and comfort, but research evidence shows limited effect on curve size, so it is considered a supportive option rather than a main treatment. -
Massage therapy
Massage helps relax tight muscles on the convex side of the curve and may ease pain and anxiety. It does not change the bone shape, but many patients feel more comfortable and sleep better when massage is combined with exercise and bracing. -
Hydrotherapy (water-based exercise)
Exercising in warm water reduces pressure on spine and joints. Water supports body weight, so people with scoliosis can move more easily and work their muscles without too much pain. This can improve endurance, balance, and confidence for land-based exercise. -
Yoga (adapted for scoliosis)
Gentle, supervised yoga poses can stretch tight muscles and encourage deep breathing and body awareness. Certain poses should be adapted to avoid over-bending or twisting. Under professional guidance, yoga may support posture, flexibility, and stress control in people with scoliosis. -
Pilates-based training
Pilates focuses on core control, breathing, and precise movement. Programs adapted for spinal curves may help balance muscle use on both sides of the trunk. Again, it does not fix bone deformity but can reduce fatigue, improve posture, and support brace use. -
Breathing and rib-cage expansion exercises
In larger curves, the rib cage can become uneven, and breathing may feel shallow. Scoliosis-specific exercises often include side-lying or sitting breathing drills that expand the collapsed side of the chest. This can improve lung pattern and comfort with physical activity. -
Psychological support and pain-coping strategies
Curves and braces can affect body image, mood, and social life. Counseling, cognitive behavioral therapy, or group support may help patients cope with chronic pain, fear of surgery, and school or peer stress, improving overall quality of life. -
Heat and cold therapy
Warm packs relax tight muscles and improve blood flow, while cold packs can reduce inflammation after activity. These simple home methods can temporarily ease back discomfort so that patients can tolerate exercise and bracing better. -
Transcutaneous electrical nerve stimulation (TENS)
TENS uses small electrical currents on the skin to change pain signals going to the brain. Some people with scoliosis-related back pain feel short-term relief with TENS, especially when medicine options are limited, though evidence is mixed. -
Custom foot orthotics (insoles)
If legs are not the same length or feet are misaligned, the pelvis and spine can tilt more. Corrective insoles or shoe lifts may improve balance and reduce some mechanical stress, especially in mild structural imbalances. -
Weight management and general fitness
Extra body weight increases load on the spine and may worsen pain. Healthy food choices and regular aerobic activity like walking or cycling help control weight, improve blood flow, and support muscles that protect the spine. -
Education and family support programs
Clear education about what scoliosis is, what a brace or surgery can and cannot do, and what to expect in follow-up visits reduces fear. Family involvement with brace schedules and exercise routines often leads to better long-term results.
Drug Treatments for Scoliosis-Related Problem
Important: Medicines below are examples commonly used for pain, muscle spasm, or nerve pain linked to scoliosis. They do not “cure” the curve. Exact drug choice, dose, and timing must always be decided by a doctor using official prescribing information. Never start or change these medicines on your own.
-
Acetaminophen (paracetamol)
Acetaminophen relieves mild to moderate pain without affecting inflammation. It is often the first medicine doctors suggest because it is easier on the stomach than many other painkillers when used correctly. It is taken by mouth, usually in divided doses through the day, and must be kept within the maximum daily dose to avoid liver damage. -
Ibuprofen (oral NSAID)
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that reduces pain and swelling by blocking prostaglandin production. It can ease back pain and muscle soreness around the curve. It is taken with food to reduce stomach upset, at the smallest effective dose and for the shortest possible time because it can affect the stomach, kidneys, and heart. -
Naproxen (oral NSAID)
Naproxen is another NSAID used for longer-lasting pain relief. It stays in the body longer than some other NSAIDs, so doses are usually spaced further apart. Doctors use official naproxen prescribing information to choose dose and schedule, especially in people with heart, kidney, or stomach problems. -
Diclofenac (oral or topical NSAID)
Diclofenac blocks inflammatory pathways and can be given as tablets or gel on the skin. Topical gel may help localized back pain with less total drug in the body. Doctors watch for possible stomach, liver, and heart side effects and follow FDA safety warnings and dosing guidance. -
Celecoxib (selective COX-2 NSAID)
Celecoxib targets COX-2 enzymes that drive inflammation while sparing some COX-1 activity, which may lower ulcer risk compared with older NSAIDs. It is used for chronic musculoskeletal pain when other NSAIDs are not tolerated. Dose and duration are chosen carefully because it can still raise cardiovascular and kidney risks. -
Muscle relaxant: Cyclobenzaprine
Cyclobenzaprine acts on the central nervous system to reduce muscle spasm. In scoliosis, tight back muscles may cause extra pain and sleep problems. This drug is usually used short-term and can cause drowsiness and dry mouth, so it is often taken at night. -
Muscle relaxant: Baclofen
Baclofen reduces muscle spasticity by acting on GABA receptors in the spinal cord. It is especially useful if scoliosis is linked to neuromuscular conditions like cerebral palsy. Dose is increased slowly to limit dizziness and weakness, and stopping suddenly can cause serious withdrawal symptoms. -
Muscle relaxant: Tizanidine
Tizanidine also works on the central nervous system to reduce nerve signals that cause muscle tightening. It may be used in selected patients with painful muscle spasm. Doctors monitor blood pressure and liver tests, and adjust dose based on day-time sleepiness and blood pressure changes. -
Gabapentin (for nerve-related pain)
Gabapentin is approved for certain nerve pain and seizures. It calms overactive nerve signaling, which may help shooting or burning pain in the leg if scoliosis compresses nerves. Dose is increased stepwise, and common side effects are dizziness and sleepiness. Prescribing information stresses not to stop suddenly to avoid withdrawal or seizure risk. -
Pregabalin (for neuropathic pain)
Pregabalin is similar to gabapentin and reduces neuropathic pain by binding to calcium channels in nerve cells. It can improve sleep and pain scores in chronic nerve pain. Doctors adjust doses based on kidney function and watch for dizziness, swelling, and mood changes. -
Tramadol (weak opioid and serotonin/norepinephrine modulator)
Tramadol is used for moderate to moderately severe pain that does not respond to simple painkillers. It has both opioid and non-opioid actions. Because it can cause dependence, nausea, sleepiness, and rare seizures, doctors prefer short-term, carefully supervised use, following detailed label guidance. -
Short-acting strong opioids (e.g., oxycodone combinations)
Strong opioids may be used for acute, severe pain after major scoliosis surgery. They act on opioid receptors to block pain signals but can cause constipation, nausea, drowsiness, breathing problems, and addiction. Guidelines recommend the lowest effective dose for the shortest possible time, with a clear taper plan. -
Topical lidocaine patches
Lidocaine patches numb superficial nerves in a small area. They are mainly used for localized nerve-related pain and may be helpful when a specific tender spot near the curve is very sensitive. Systemic absorption is low, but patches must be used within labeled time limits to avoid toxicity. -
Topical NSAID gels (e.g., diclofenac gel)
These gels are rubbed onto the painful area over the back muscles. They deliver anti-inflammatory medicine through the skin with much less drug in the bloodstream. This can give mild to moderate relief with fewer stomach and heart risks than long-term oral NSAIDs, when used as labeled. -
Duloxetine (serotonin–norepinephrine reuptake inhibitor)
Duloxetine is approved for several chronic pain conditions. It changes brain chemicals that process pain signals and can also treat anxiety or depression related to long-term pain. Doctors start at low doses and monitor blood pressure, sleep, and mood, as it can cause nausea and rare suicidal thoughts. -
Amitriptyline (tricyclic antidepressant for pain)
At low doses, amitriptyline can help chronic nerve and muscle pain and improve sleep. It works by changing serotonin and norepinephrine levels. It may cause dry mouth, constipation, and drowsiness, so doctors often advise taking it at night and adjusting the dose very slowly. -
Calcitonin (bone-active hormone for osteoporosis-related pain)
In adults with scoliosis and osteoporosis, calcitonin nasal spray or injection may help bone pain and support other osteoporosis treatments. It slows bone breakdown. Because long-term safety and benefit are limited, guidelines use it cautiously and often for short periods. -
Bisphosphonates (e.g., alendronate) in adults with weak bones
These drugs slow bone loss and can reduce fracture risk in adults with low bone density, which may coexist with degenerative scoliosis. They must be taken exactly as directed to protect the esophagus and reduce side effects such as stomach pain and rare jaw problems. -
Vitamin D prescription forms (for deficiency)
If blood tests show low vitamin D, high-dose prescription vitamin D may be used for a short time. Vitamin D helps the body absorb calcium and build strong bones, which is important for any spine condition. Doses and treatment length are based on lab results to avoid toxicity. -
Proton pump inhibitors or stomach protectors (with NSAIDs)
In patients who must take NSAIDs for scoliosis-related pain and have stomach-ulcer risk, doctors may add medicines like proton pump inhibitors to protect the stomach lining. These do not treat scoliosis itself but make pain treatment safer.
Dietary Molecular Supplements
Note: Supplements can interact with medicines and are not a replacement for bracing or surgery. Always discuss any supplement with a doctor.
-
Calcium
Calcium is a key mineral for bone strength. Adequate intake from food or supplements (if diet is low) supports the vertebrae that form the spine. It works with vitamin D to keep bones dense. Too much can cause kidney stones, so amounts should be tailored to age and diet. -
Vitamin D
Vitamin D helps the gut absorb calcium and supports bone remodeling. Many children and adults have low levels, especially with little sun exposure. Correcting deficiency can improve overall bone health, which is important in any spinal deformity, though it does not directly change the curve. -
Magnesium
Magnesium is involved in muscle relaxation and bone structure. Balanced magnesium intake may help reduce muscle cramps and support normal nerve function. Very high supplement doses can cause diarrhea and heart rhythm changes, so medical supervision is advised. -
Omega-3 fatty acids (fish oil)
Omega-3 fats have anti-inflammatory effects and may slightly reduce chronic pain in some conditions. In scoliosis, they may support general joint and muscle health. They can thin the blood at high doses, so people on blood thinners must use them carefully. -
Vitamin K2
Vitamin K2 helps guide calcium into bones and away from blood vessels. Adequate intake may support bone quality, especially when combined with vitamin D and calcium. High-dose supplements can interact with blood-thinning medicines, so doctor guidance is important. -
Collagen peptides
Collagen is a main protein in cartilage, ligaments, and bone. Collagen supplements may modestly support joint comfort and bone metabolism. They are usually taken as powder mixed with water. Evidence for scoliosis specifically is limited, so they are considered supportive only. -
Glucosamine and chondroitin
These molecules are building blocks of cartilage and are often used for spine and joint pain. Some adults report small pain improvements, but study results are mixed. They may interact with some medicines and should be avoided in shellfish allergy in certain products. -
Curcumin (from turmeric)
Curcumin has anti-inflammatory and antioxidant properties and might modestly reduce chronic pain in some musculoskeletal conditions. Absorption is better when taken with pepper extract or fat. It can interact with blood-thinning medicines and should be used carefully before surgery. -
Antioxidant vitamins (C and E)
Vitamins C and E help protect cells from oxidative stress and support collagen formation and tissue repair. A diet rich in fruits and vegetables usually provides enough. High-dose pills can cause side effects, so supplements should be used only when diet is clearly inadequate. -
Probiotics
Probiotics support gut health and may help with nutrient absorption and inflammation balance. For people taking pain medicines that irritate the stomach, keeping gut flora healthy may indirectly improve comfort and nutrition, though direct scoliosis effects are not proven.
Immunity-Booster / Regenerative / Stem-Cell-Related Drugs
These options are not standard scoliosis treatments. Some are used for bone health in special cases or are still in research.
-
Teriparatide (PTH analog)
Teriparatide is an anabolic (bone-building) medicine for severe osteoporosis. It stimulates osteoblasts to form new bone. In adults with weak bones facing complex spinal surgery, improving bone strength may help fusion success, but use is limited to certain high-risk patients under close specialist care. -
Romosozumab (sclerostin antibody)
Romosozumab increases bone formation and decreases bone breakdown. It is used for high-risk osteoporosis and may potentially support spinal fusion in selected adults. It carries heart-risk warnings, so it is not used broadly and always requires specialist evaluation. -
Recombinant BMP-2 (bone morphogenetic protein)
BMP-2 is a bioactive protein sometimes used during spinal fusion surgery to encourage bone growth between vertebrae. It is placed at the surgical site, not taken as pills. It can improve fusion rates but may also cause extra bone growth and swelling, so surgeons weigh benefits and risks carefully. -
Mesenchymal stem cell therapies (research stage)
Mesenchymal stem cells can develop into bone, cartilage, and muscle cells. Experimental studies are exploring their use to improve spinal fusion or repair damaged discs. These therapies remain mostly in clinical trials and are not routine care for scoliosis; patients should avoid unregulated clinics. -
Platelet-rich plasma (PRP)
PRP is prepared from a patient’s own blood and concentrates growth factors. It is injected into tissues to try to support healing. Evidence for PRP in scoliosis-related back pain or fusion success is limited, so it is considered experimental and should only be used in controlled settings. -
Growth hormone therapy (in selected endocrine conditions)
Some children with growth hormone deficiency receive GH injections to help them grow. In rare situations, such therapy may influence spinal growth and scoliosis behaviour, so specialists monitor curves closely. It is not a scoliosis treatment and must be managed by pediatric endocrinologists and orthopedists together.
Surgical Treatments for Scoliosis
The two main types of surgery are:
- Anterior fusion: This surgical approach is through an incision at the side of the chest wall.
- Posterior fusion: This surgical approach is through an incision on the back and involves the use of metal instrumentation to correct the curve. One or both of these surgical procedures may be needed. The surgery may be done in one or two stages and, on average, takes four to eight hours. A Cochrane review could not draw conclusions on how effective surgical interventions were when compared to non-surgical interventions in patients with adolescent idiopathic scoliosis.[rx]
-
Posterior spinal fusion with instrumentation
This is the most common scoliosis surgery. The surgeon reaches the spine from the back, places screws and rods on the vertebrae, gently straightens the curve, and adds bone graft to fuse the operated levels into one solid block. It is done to stop curve progression, improve alignment, and protect lungs and nerves in larger curves. -
Anterior spinal fusion (front approach) in selected cases
In some curves, surgeons approach the spine from the chest or abdomen. They remove discs between vertebrae, place bone graft, and insert implants to hold the correction. This method is used less often today but can be helpful for specific curve patterns and patient needs. -
Vertebral body tethering (growth-modulation surgery)
In some growing children with idiopathic scoliosis, surgeons can place a flexible cord along the outer side of the curve. As the child grows, the tether slows growth on that side, letting the other side catch up and partially straighten the spine. It is less rigid than fusion but is newer, with limited long-term data. -
Growing-rod or magnetically controlled rod systems
In young children with early-onset scoliosis, surgeons attach rods to the spine or ribs to control the curve while allowing the chest and lungs to keep growing. Newer magnetically controlled rods can be lengthened in clinic without repeated open surgeries. These procedures are complex and reserved for serious early curves. -
Revision surgery for failed or painful previous fusion – Adults who had earlier scoliosis surgery may later develop broken hardware, non-union of the fusion, or painful imbalance. Revision surgery aims to repair fusion, adjust alignment, and relieve nerve or lung pressure. It is technically demanding, with higher complication risks, so is carefully planned by experienced spine teams. Surgery for scoliosis is performed by a surgeon specializing in spine surgery. For various reasons, it is usually impossible to completely straighten a scoliotic spine, but in most cases, significant corrections are achieved.
-
Spinal fusion with instrumentation – Spinal fusion is the most widely performed surgery for scoliosis. In this procedure, bone [either harvested from elsewhere in the body (autograft) or from a donor (allograft)] is grafted to the vertebrae so when they heal, they form one solid bone mass and the vertebral column becomes rigid. This prevents worsening of the curve, at the expense of some spinal movement. This can be performed from the anterior (front) aspect of the spine by entering the thoracic or abdominal cavities, or more commonly, performed from the back (posterior). A combination may be used in more severe cases, though the modern pedicle screw system has largely negated the need for this.[rx]
In recent years all-screw systems have become the gold-standard technique for adolescent idiopathic scoliosis. Pedicle screws achieve better fixation of the vertebral column and have better biomechanical properties than previous techniques, so enabling greater correction of the curve in all planes.[rx]
Pedicle screw-only posterior spinal fusion may improve major curve correction at two years among patients with adolescent idiopathic scoliosis (AIS)[rx] as compared to hybrid instrumentation (proximal hooks with distal pedicle screws) (65% versus 46%) according to a retrospective, matched-cohort study.[rx] The prospective cohorts were matched to the retrospective cohorts according to patient age, fusion levels, Lenke curve type, and operative method. The two groups were not significantly different in regard to age, Lenke AIS curve type, or Riser grade. The numbers of fused vertebrae were significantly different (11.7±1.6 for pedicle screw versus 13.0±1.2 for hybrid group). This study’s results may be biased due to the pedicle screw group’s being analyzed prospectively versus retrospective analysis of the hybrid instrumentation group.
In general, modern spinal fusions have good outcomes with high degrees of correction and low rates of failure and infection. However a systematic review of PubMed papers in 2008 concluded “Scoliosis surgery has a varying but high rate of complications”, although the non-standardised data on complications was difficult to assess and was incomplete.[rx] Patients with fused spines and permanent implants tend to have normal lives with unrestricted activities when they are younger; it remains to be seen whether those that have been treated with the newer surgical techniques develop problems as they age.[rx]
Thoracoplasty
A complementary surgical procedure a surgeon may recommend is called thoracoplasty (also called costoplasty). This is a procedure to reduce the rib hump that affects most scoliosis patients with a thoracic curve. A rib hump is evidence of some rotational deformity to the spine. Thoracoplasty may also be performed to obtain bone grafts from the ribs instead of the pelvis, regardless of whether a rib hump is present. Thoracoplasty can be performed as part of a spinal fusion or as a separate surgery, entirely.
Thoracoplasty is the removal (or resection) of typically four to six segments of adjacent ribs that protrude. Each segment is one to two inches long. The surgeon decides which ribs to resect based on either their prominence or their likelihood to be realigned by correction of the curvature alone. The ribs grow back straight.
Thoracoplasty has risks, such as increased pain in the rib area during recovery or reduced pulmonary function (10–15% is typical) following surgery. This impairment can last anywhere from a few months to two years. Because thoracoplasty may lengthen the duration of surgery, patients may also lose more blood or develop complications from the prolonged anesthesia. A more significant, though far less common, risk is the surgeon might inadvertently puncture the pleura, a protective coating over the lungs. This could cause blood or air to drain into the chest cavity, hemothorax or pneumothorax, respectively.[rx]
Surgery without fusion for growing children
Implants that aim to delay spinal fusion and to allow more spinal growth in young children is the gold standard for surgical treatment of early onset scoliosis. Surgery without fusion can be divided into three principles: distraction of the entire spine, compression of the short segment of spine, and guided-growth techniques. Distraction-based systems include Vertical, Expandable Prosthetic Titanium Ribs (VEPTR) & growing rods. The concept uses distraction to create additional soft-tissue space in-between the vertebrae, for the bone to later grow into. Its universal application was thrusted through the use of traditional growth rods which required repeated invasive surgeries every 6–12 months for the sustenance of growth, via distraction. Nowadays developed countries only use MAGEC (MAGnetic Expansion Control) rods to non-invasively lengthen the spine. In contrast, developing and under-developed countries still use traditional growing rods, which require invasive surgery every 6–12 months, because of high initial cost associated with procurement of MAGEC rods. Compression-based system include tethering using a flexible rope-like implant and are relatively new to receive FDA approval. Guided-growth technique include SHILLA (named after a hotel in Korea, where the concept was initiated). SHILLA has the advantage of being one-time surgery and is technologically less demanding compared with MAGEC rod. However, there are still two major disadvantages of using SHILLA: loss of correction and need for osteotomies.[rx][rx]
The failure of most of these standalone techniques has shown that the concept of “one size fits all” is not applicable for the surgical management of EOS. Therefore, newer concepts employing two or more of the above philosophies, i.e. various combinations of distraction-based, guided-growth, and compression-based approaches might be more suitable and biomechanically-speaking, a more optimal surgical intervention. One such combination currently used for surgery includes active apex correction (APC). It is a hybrid of guided-growth and compression-based management of deformity. The technique simply consists of replacing the apical fusion (of traditional SHILLA) with unilateral compression (via pedicle screws or any other means) on the convex side. The latest clinical results presented by spine researchers Aakash Agarwal and Alaaedldin Azmi Ahmad on APC shows good clinical results with no economic barrier to use the technology.[rx][rx][rxx]
Physiotherapy Treatment
While scoliosis does not usually require immediate medical attention or endanger one’s life, it can greatly impede the quality of life due to immobility difficulties, pain and fatigue. After a spinal cord injury, one must be keenly aware of scoliosis. Most people with a spinal cord injury experience some paralysis of their torso muscles, which leads to difficulty in holding the backbone in its natural position.
Many people with spinal cord injuries have bad posture because of this, which leads to scoliosis as the years’ progress. This, however, does not to be inevitable. Scoliosis can be prevented after an SCI. And if you do get scoliosis, there are many options available to treat it. Here are the options available for people with paralysis to prevent, maintain and correct scoliosis.
Annual X-Rays
It is important to get annual X-rays of your back to monitor any curves that may be forming. You’ll want to find an orthopedic surgeon familiar with scoliosis, or a rehab medicine doctor who can monitor your scoliosis, and make sure that it isn’t getting worse. The main goal is to ensure that no scoliosis occurs, but if it does, you’ll want a doctor who can monitor the curvature and to make sure it is not endangering any important organs, such as your lungs.
Stay Active
Moving as much as possible if you have movement in your upper body can help a lot in preventing scoliosis post-injury. It is also important to do a daily range of motion exercises to keep your back in the natural position as often as possible.
Maintain a Healthy Weight
Eating healthy and maintaining a healthy weight post-injury can go a long way in preventing and maintaining scoliosis. Eating healthy can minimize the symptoms of scoliosis as well. Also, making sure you’re getting enough Vitamin D, can also make a huge difference in preventing osteoporosis, which can lead to scoliosis. To monitor osteoporosis, annual DEXA scans are also suggested. Talk to your doctor about getting one.
Stretch Your Back
Keeping your back long and limber can make a huge impact when it comes to preventing and minimizing the effects of scoliosis. Muscle memory is a real thing and is still something you can tap into. By stretching your back daily, this will force your back into its natural position. Massage of the curve and muscles affected can also help if done regularly.
Scoliosis Specific Exercise
Scoliosis specific exercises have been found to improve treatment outcomes when utilized in addition to bracing and other standards of care.[rx] Scoliosis specific exercises include methods such as Schroth[rx] which specifically aim to correct aesthetic differences and strengthened muscles and connective tissue that may have atrophied as a result of scoliosis and asymmetric posture. The Schroth method is a three-dimensional exercise approach aiming to improve spinal curvature and vertebral rotational angles. A physical therapist guides the patient through breathing techniques and exercises to strengthen weak muscle sand and relieve overactive ones. In addition to spinal realignment, the Schroth method improves self-image, quality of life, and lumbar extensor strength.[rx] Schroth exercises and other scoliosis specific exercises should be utilized in conjunction with bracing and other standards of care,[rx] and be performed under the guidance of a trained professional to ensure the exercises are effective and target the individual’s curve pattern so that the correct muscles are strengthened. Strengthening spinal muscles is a crucial preventive measure. This is because the muscles in the back are essential when it comes to supporting the spinal column and maintaining the spine’s proper shape. Exercises that will help improve the strength of the muscles in the back include rows and leg and arm extensions.[rx] Elastic resistance exercise may also be able to sustain the progression of spinal curvature.[rx] This type of exercise is able to sustain progression by equalizing the strength of the torso muscles found on each side of the body.
Self-care
Disability caused by scoliosis, as well as physical limitations during recovery from treatment-related surgery, often affects an individual’s ability to perform self-care activities.[rx] One of the first treatments of scoliosis is the attempt to prevent further curvature of the spine. Depending on the size of the curvature, this is typically done in one of three ways: bracing, surgery, or postural positioning through customized cushioning.[rx][rx][rx] Stopping the progression of the scoliosis can prevent the loss of function in many activities of daily living by maintaining range of motion, preventing deformity of the rib cage, and reducing pain during activities such as bending or lifting.
Occupational therapists are often involved in the process of selection and fabrication of customized cushions. These individualized postural supports are used to maintain the current spinal curvature, or they can be adjusted to assist in the correction of the curvature. This type of treatment can help to maintain mobility for a wheelchair user by preventing the deformity of the rib cage and maintaining an active range of motion in the arms.[rx]
For other self-care activities (such as dressing, bathing, grooming, personal hygiene, and feeding), several strategies can be used as a part of occupational therapy treatment. Environmental adaptations for bathing could include a bath bench, grab bars installed in the shower area, or a handheld shower nozzle.[rx] For activities such as dressing and grooming, various assistive devices and strategies can be used to promote independence. An occupational therapist may recommend a long-handled reacher that can be used to assist self-dressing by allowing a person to avoid painful movements such as bending over; a long-handled shoehorn can be used for putting on and removing shoes. Problems with activities such as cutting meat and eating can be addressed by using specialized cutlery, kitchen utensils, or dishes.
Productivity
Productive activities include paid or unpaid work, household chores, school, and play.[rx] Recent studies in healthcare have led to the development of a variety of treatments to assist in the management of scoliosis thereby maximizing productivity for people of all ages. Assistive technology has undergone dramatic changes over the past 20 years; the availability and quality of the technology has improved greatly.[rx] As a result of using assistive technology, functional changes may range from improvements in abilities, performance in daily activities, participation levels, and quality of life.[rx]
A common assistive technology intervention is specialized seating and postural control. For children with poor postural control, a comfortable seating system that provides them with the support needed to maintain a sitting position can be essential for raising their overall level of well-being.[rx] A child’s well-being in a productive sense involves the ability to participate in classroom and play activities.[rx] Specialized wheelchair seating has been identified as the most common prescription in the management of scoliosis in teenagers with muscular dystrophy.[rx]
With comfortable wheelchair seating, teenagers are able to participate in classroom activities for longer periods with less fatigue. By tilting the seating position 20° forward (toward the thighs), seating pressure is significantly redistributed, so sitting is more comfortable. If an office worker with scoliosis can sit for longer periods, increased work output is likely to occur and could improve quality of life. Tall, forward-sloping seats or front parts of seats, and when possible with tall desk with the opposite slope, can, in general, reduce pains and the need of bending significantly while working or studying, and that is particularly important with braced, fragile, or tender backs. An open hip angle can benefit the used lung volume and respiration.[rx][rx]
For those not using a wheelchair, bracing may be used to treat scoliosis. Lifestyle changes are made to compensate for the proper use of spine braces.
Leisure
Physical symptoms such as chest pains, back pains, shortness of breath, and limited spinal movement can hamper or preclude participation in leisure activities of a physical nature. The occupational therapist’s role is to facilitate participation by helping the patient manage these symptoms.
Bracing is a common strategy recommended by an occupational therapist, in particular, for individuals engaging in sports and exercise.[rx] An OT is responsible for educating an individual on the advantages and disadvantages of different braces, proper ways to wear the brace, and the day-to-day care of the brace.
To help a person manage heart and lung symptoms, such as shortness of breath or chest pains, an occupational therapist can teach the individual energy conservation techniques.[rx] This includes scheduling routine breaks during the activity, as suitable for the individual. For example, an occupational therapist can recommend that a swimmer take breaks between laps to conserve energy. Adapting or modifying the exercise or sport is another way a person with scoliosis can do it.[rx] Adapting the activity may change the difficulty of the sport or exercise. For example, it might mean taking breaks throughout an exercise. If a person with scoliosis is unable to participate in a sport or exercise, an OT can help the individual explore other physical activities that are suitable to his/her interests and capabilities. An occupational therapist and the person with scoliosis can explore enjoyable and meaningful participation in the sport/exercise in another capacity, such as coaching or refereeing.
Bracing
Bracing is most effective when the patient has bone growth remaining (is skeletally immature) and should aim to both prevent progression of the curve (prevent progression to surgery), as well as reduce the scoliosis curve. Reduction of the curve is important as the natural history of idiopathic scoliosis suggests it can continue to progress at a rate ~1 degree per year in adulthood,[rx] while the treatment results of bracing have been shown to hold over >15 years.[rx] In some cases with juveniles, bracing has reduced curves significantly, going from a 40 degrees (of the curve, mentioned in length above.) out of the brace to 18 degrees in it. Braces are sometimes prescribed for adults to relieve pain related to scoliosis. Bracing involves fitting the patient with a device that covers the torso; in some cases, it extends to the neck. The most commonly used brace is a TLSO, such as a Cheneau type brace, a corset-like appliance that fits from armpits to hips and is custom-made from fiberglass or plastic. It is worn upwards of 18–23 hours a day, depending on the doctor’s prescription, and applies pressure on the curves in the spine. The effectiveness of the brace depends not only on brace design and orthotist skill; patient compliance; and amount of wear per day, but also the “stiffness” of the spine resulting from a shortened spinal cord[rx][rx] and/or nerve tension.[rx] as evidence by the force necessary (mean force ~121 lbs) to physically correct scoliosis during spinal surgery[rx] The typical use of braces for idiopathic scoliosis is to prevent progression to surgical range as well as reduce the scoliotic curve of the spine as spinal fusion surgery can reduce mobility due to fusion of the vertebrate while potentially increasing pain long term.[rx] For non-idiopathic scoliosis (ie. neuromuscular, congenital, etc.) and those with additional comorbidities (ie. Marfans Syndrome) spinal surgery may be required due to structural changes in the spine.
Indications for Scoliosis Bracing: Scoliosis professionals determine the proper bracing method for a patient after a complete clinical evaluation. The patient’s growth potential, age, maturity, and scoliosis (Cobb angle, rotation, and sagittal profile) are also considered. Immature patients who present with Cobb angles less than 20 degrees should be closely monitored and proactively treated based on their risk of progression[rx] as surgery can be prevented with early intervention of conservative treatment.[rx] Immature patients who present with Cobb angles of 20 degrees to 29 degrees should be braced according to the risk of progression by considering age, Cobb angle increase over a six-month period, Risser sign, and clinical presentation. Immature patients who present with Cobb angles greater than 30 degrees should be braced. However, these are guidelines and not every patient will fit into this table. For example, an immature patient with a 17-degree Cobb angle and significant thoracic rotation or flatback could be considered for nighttime bracing. On the opposite end of the growth spectrum, a 29-degree Cobb angle and a Risser sign three or four might not need to be braced because there is reduced potential for progression.[rx]
Surgery is indicated by the Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) at 45 degrees to 50 degrees[rx] and by the Scoliosis Research Society (SRS) at a Cobb angle of 45 degrees.[rx] SOSORT uses the 45-degree to 50-degree threshold as a result of the well-documented, plus or minus five degrees measurement error that can occur while measuring Cobb angles.
Scoliosis braces are usually comfortable for the patient, especially when it is well designed and fit; also after the 7- to 10-day break-in period. A well fit and functioning scoliosis brace provides comfort when it is supporting the deformity and redirecting the body into a more corrected and normal physiological position.[rx]
The Scoliosis Research Society’s recommendations for bracing include curves progressing to larger than 25°, curves presenting between 30 and 45°, Risser sign 0, 1, or 2 (an X-ray measurement of a pelvic growth area), and less than six months from the onset of menses in girls.[rx]
Progressive scolioses exceeding 25° Cobb angle in the pubertal growth spurt should be treated with a pattern-specific brace like the Chêneau brace and its derivatives, with an average brace-wearing time of 16 hours/day (23 hours/day assures the best possible result).
The latest standard of brace construction is with CAD/CAM technology. With the help of this technology, it has been possible to standardize the pattern-specific brace treatment. Severe mistakes in brace construction are largely ruled out with the help of these systems. This technology also eliminates the need to make a plaster cast for brace construction. The measurements can be taken in any place and are simple (and not comparable to plastering). Available CAD/CAM braces include the Regnier-Chêneau brace, the Rigo-System-Chêneau-brace (RSC brace), the Silicon Valley Brace, and the Gensingen brace; braces can and should be customized to fit the individual’s curve pattern and reduce the curve as much as possible as immediate in-brace correction has been shown to be associated with better treatment outcomes.[rx][rx] Many patients prefer the “Chêneau light” brace as it has good in-brace corrections reported in international literature and is easier to wear than other braces in use today.[rx][rx] However, this brace is not available for all curve patterns.
Prior to 2013 the efficacy of bracing has not been definitively demonstrated in randomised clinical studies, with more limited studies giving inconsistent conclusions.[rx] In 2013 the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST) published results establishing benefits of bracing in adolescents with idiopathic scoliosis. In the randomized cohort, 72% in the group instructed to wear a brace for 18 hours per day against 48% in the observation group sustained curve progression to under 50 degrees, the proxy used for not requiring surgery. Additionally results suggested that the more a patient wore the brace, the better the result.[rx][rx]
Casting
In progressive infantile and sometimes juvenile scoliosis, a plaster jacket applied early may be used instead of a brace. It has been proven possible[rx] to permanently correct cases of infantile idiopathic scoliosis by applying a series of plaster casts (EDF: elongation, derotation, flexion) on a specialized frame under corrective traction, which helps to “mould” the infant’s soft bones and work with their growth spurts. This method was pioneered by UK scoliosis specialist Min Mehta.[rx] EDF casting is now the only clinically known nonsurgical method of complete correction in progressive infantile scoliosis. Complete correction may be obtained for curves less than 50° if the treatment begins before the second year of life.[rx][rx]
Complications
The risk of undergoing surgery for scoliosis was estimated in 2008 to be varying, but with a high rate of complications. Possible complications may be inflammation of the soft tissue or deep inflammatory processes, breathing impairments, bleeding and nerve injuries. It is not yet clear what to expect from spine surgery in the long term.[rx][rx] Taking into account that signs and symptoms of spinal deformity cannot be changed by surgical intervention, surgery remains primarily a cosmetic indication, only especially in patients with adolescent idiopathic scoliosis, the most common form of scoliosis never exceeding 80°.[rx][rx] However, the cosmetic effects of surgery are not necessarily stable.[rx]
For spinal fusion surgery on AIS cases, with instrumentation attached using pedicle screws, complication rates were reported in 2011 as transient neurological injuries between 0% to 1.5%, a pedicle fracture rate of 0.24%, screw malposition assessed by radiography at 1.5%, 6% when assessed by CT scans though these patients were asymptomatic not requiring screw revision, and screw loosening noted in 0.76% of patients.[rx]
For surgery without fusion in growing children, substantial percentage of patients undergoing SHILLA technique experience loss of correction via crankshafting or adding-on (eg, distal migration). In addition, the need for osteotomies on the concave side has the potential of severe complications. For MAGEC rods, higher distraction magnitude resulted in the generation of higher distraction forces, and this in combination with off-axis loading (exemplified by “growth marks”) result in wear and breakage of MAGEC rod’s components.[rx][rx]
After-surgery care
Pain medication
In the event of surgery to correct scoliosis, pain medications and anesthesia will be administered. Before the surgery, the patient will receive anesthesia. With adults, the anesthesia will be administered through an IV in the antecubital region of the arm. With young children, however, the child will be asked to breathe in nitrous oxide, or laughing gas. Because needles can be frightening for a young child, the nitrous oxide will put them to sleep so the anesthesiologist can then insert the IV in order to give them the anesthesia. After the surgery, the patient will most likely be given morphine. Until the patient is ready to take the medicine by mouth, an IV will be giving them their medication. Morphine is the most common pain medicine used after scoliosis surgery, and is often administered through a patient-controlled analgesia (PCA) system. The PCA system allows the patient to push a button when they are feeling pain, and the PCA will emit the drugs into the IV and then into the body. To prevent overdoses, there is a limit on the number of times a patient can push the button. If a patient pushes the button too much at once, the PCA will reject the request.[rx]
Bowel and bladder function
For the patient’s bladder control, a catheter will be inserted so that a patient can urinate without having to move. A catheter is inserted because the patient will not have much free movement to be able to get up and walk to the bathroom. The most common type of catheter used after major surgeries is an indwelling Foley catheter. The indwelling Foley catheter is most often put in the urethra, with a tube leading into a drainage bag. Once the catheter is inserted into the urethra, a balloon is blown up inside the bladder in order to keep it from falling out. The balloon allows the catheter to remain inside the urethra until the patient is able to get up and go to the bathroom on their own.[rx] The drainage bag is connected to the side of the bed, and must be changed or emptied out once it is full.
Bowel control can vary from patient to patient. The combination of no food, very little fluids, and a lot of prescription drugs has the potential to cause many patients to become constipated. The body is used to a normal diet, and used to excreting waste in a system. Interrupting the system can cause bowel problems. This constipation can be resolved in a couple of ways. The first way, and the most common way, is to administer a rectal suppository. A rectal suppository is administered through the anus, and into the rectum. They are bullet-shaped and contain medicine that will help the patient’s bowels get back on track. Once the suppository is inserted, it is designed to melt off the wax-like case, and put the medicine in the body.[rx] If the suppository does not work, a laxative may be continued at home to keep the bowels in full function.
Diet
When first returning home after surgery, a nutritional diet is necessary in order to keep the body operating correctly. Junk food is not a good idea, as the grease and sugar can irregulate the bowels. Fruit, vegetables, and juices will be a vital part in the diet.[rx] Food and drink will be limited for the patient after surgery. Because the bowels are not fully active because of anesthetic, clear water and ice may be the only acceptable thing to ingest. After the digestive tract is back up to speed, soft food and drink like pudding, soup broth, and orange juice are acceptable.[rx] Very dark urine with a strong odor means that the person is most likely dehydrated and needs more fluids. In order for the urine to become a pale or clear color, the patient will need to drink a lot of water. Juices such as prune juice are a healthy option and prune juice also helps with constipation, a common factor after surgery. When it comes to food, whole grains should be added into the diet. Whole grains can be broken down easily by the body whereas processed grains and flour cannot be broken down easily. Processed grains and flour also add to constipation.[rx]
Prevention and Early Detection
-
Scoliosis itself often cannot be completely prevented because many cases are idiopathic and related to genetics and growth patterns.
-
Regular school or clinic screening during growth spurts helps detect curves early, when bracing can still work.
-
Parents can watch for uneven shoulders, a rib hump when the child bends forward, or clothes hanging unevenly, and seek medical advice early.
-
Encouraging daily physical activity supports strong muscles and bones, which helps the spine cope better with curves.
-
Providing a balanced diet rich in calcium, vitamin D, and protein supports bone growth through childhood and adolescence.
-
Avoiding smoking and second-hand smoke in older teens and adults helps protect bone quality and disc health.
-
Teaching good backpack habits (both straps, not overloaded) can reduce muscle strain in children with or without scoliosis.
-
Managing neuromuscular and connective tissue diseases early may limit the severity of secondary scoliosis in those conditions.
-
Keeping follow-up appointments and following brace and exercise plans can prevent many curves from reaching surgical size.
-
Educating teenagers about their condition helps them take ownership of treatment and make healthier daily choices.
When to See a Doctor
You should see a doctor or spine specialist if you or your child notice uneven shoulders, a leaning posture, or one side of the rib cage sticking out when bending forward. These can be early signs of scoliosis that need proper examination and possibly X-rays.
Medical review is urgent if there is rapidly increasing back pain, weakness, numbness, problems with walking, bladder or bowel changes, or trouble breathing. These red-flag symptoms are uncommon in simple adolescent idiopathic scoliosis and may mean another serious spine or nerve problem that must be checked quickly.
Anyone already diagnosed with scoliosis should keep all follow-up visits. If a brace no longer fits, pain suddenly worsens, or the curve seems to be changing quickly, contact the treatment team for earlier review instead of waiting for the routine appointment.
What to Eat and What to Avoid
-
Eat calcium-rich foods like milk, yogurt, cheese, tofu, and leafy greens to support strong vertebrae and ribs.
-
Get enough vitamin D from safe sun exposure and foods such as fortified milk and oily fish, or supplements if advised.
-
Choose lean proteins (fish, eggs, beans, chicken) to help muscles repair after exercises and brace use.
-
Include plenty of fruits and vegetables to provide vitamins, minerals, and antioxidants for tissue healing and general health.
-
Use healthy fats like olive oil, nuts, seeds, and omega-3-rich fish to support joint and heart health.
-
Limit sugary drinks and junk food, which add calories but no helpful nutrients and can contribute to weight gain that stresses the spine.
-
Avoid crash diets, especially in teenagers, because rapid weight loss and low nutrient intake can weaken bones and muscles.
-
Limit very salty processed foods, which may affect bone balance when eaten in large amounts over time.
-
Be careful with caffeine and energy drinks, as high intake may reduce calcium absorption and disturb sleep that is needed for growth and healing.
-
Avoid smoking and alcohol (for older teens and adults) because both damage bone and disc health and can worsen recovery after spine surgery.
Frequently Asked Questions
-
Can exercise cure scoliosis?
Exercise alone cannot straighten bones that are already curved, but scoliosis-specific physiotherapy and general strengthening can improve posture, reduce pain, and support bracing or surgery results. Think of exercise as a powerful helper, not a magic cure. -
Will scoliosis get worse as I grow?
During growth spurts, some curves stay stable, while others grow quickly. Risk depends on curve size, age, and remaining growth. Regular checkups and X-rays help doctors see which curves are likely to progress and choose treatment early. -
Does every person with scoliosis need a brace?
No. Small curves in nearly grown children may only need observation. Braces are usually suggested for moderate curves in growing children to stop them getting worse. The decision is based on careful measurements and discussion with the family. -
Is scoliosis painful?
Many teenagers with idiopathic scoliosis have no or only mild pain, but adults and some children can develop back and muscle pain, especially with larger curves or degenerative changes. Pain treatment is personalized and may involve exercise, medicines, and sometimes injections or surgery. -
Can scoliosis affect breathing or the heart?
Very large curves, especially in the upper back, can deform the chest and restrict lung expansion, and in extreme cases can affect heart and lung function. This is one reason doctors try to control severe curves early. -
Will I still be able to play sports?
Many people with mild to moderate scoliosis can safely join sports and physical education. Activity helps muscle strength and mental health. Contact sports or heavy weightlifting may need limits in some cases, especially after surgery; your specialist will guide you. -
Does carrying a heavy school bag cause scoliosis?
Carrying heavy bags on one shoulder can cause muscle strain and poor posture but does not usually cause structural scoliosis. However, good backpack habits are still important to reduce discomfort in people with or without curves. -
Can scoliosis be prevented?
Most common adolescent idiopathic scoliosis cannot be fully prevented because the cause is not known. What we can do is detect it early, support bone and muscle health, and follow treatment plans to prevent serious progression. -
Is surgery always necessary for scoliosis?
Surgery is needed only in a small percentage of patients, usually when curves are large, progressing, or causing serious symptoms. Many people manage well for life with observation, bracing, and non-surgical care. -
How long do I have to wear a brace?
Most children wear a brace until they finish most of their growth. This can mean several years. The exact hours per day and total duration depend on curve size, brace type, and growth stage. Close follow-up and good brace “time” are key for success. -
Can scoliosis come back after surgery?
After a solid fusion, the fused part of the spine usually stays stable, but small changes can happen above or below the fused area over many years. Sometimes new degeneration appears and needs monitoring, especially in adults. -
Is scoliosis hereditary?
Scoliosis tends to run in families, and several genes appear to be involved, but inheritance is complex. Having a relative with scoliosis increases risk slightly, so siblings may need screening during growth. -
Can I get pregnant and have children if I have scoliosis?
Most people with scoliosis, including many who had surgery, can have healthy pregnancies. Back pain may increase, and obstetric and anesthesia teams should know about the spinal curve or fusion. Planning with your doctors before pregnancy is helpful. -
Will scoliosis affect my height?
Large curves can slightly reduce final height because the spine is more curved instead of straight, but many people with mild or moderate scoliosis reach near-normal height. Treating curves during growth helps preserve height and body balance. -
Who should manage scoliosis care?
Ideal care comes from a team including pediatricians or primary doctors, spine surgeons, rehabilitation doctors, physiotherapists, orthotists, and sometimes psychologists or dietitians. Team care helps combine safe monitoring, exercise, bracing, pain control, and, when needed, surgery.
Disclaimer: Each person’s journey is unique, treatment plan, life style, food habit, hormonal condition, immune system, chronic disease condition, geological location, weather and previous medical history is also unique. So always seek the best advice from a qualified medical professional or health care provider before trying any treatments to ensure to find out the best plan for you. This guide is for general information and educational purposes only. Regular check-ups and awareness can help to manage and prevent complications associated with these diseases conditions. If you or someone are suffering from this disease condition bookmark this website or share with someone who might find it useful! Boost your knowledge and stay ahead in your health journey. We always try to ensure that the content is regularly updated to reflect the latest medical research and treatment options. Thank you for giving your valuable time to read the article.
The article is written by Team Rxharun and reviewed by the Rx Editorial Board Members
Last Update: April 16, 2025.




